Introduction
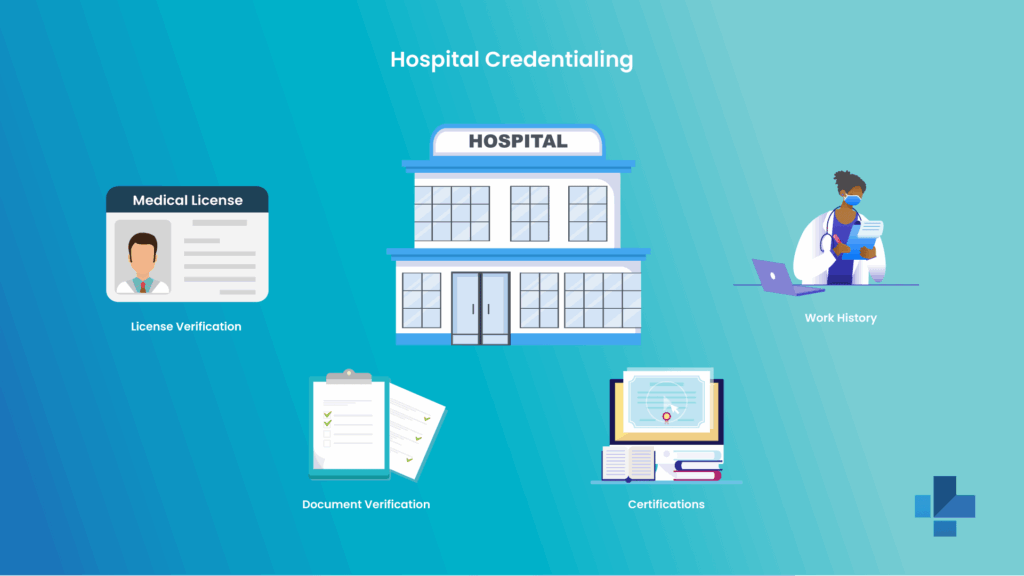
Hospital credentialing is a formal procedure used to confirm that healthcare providers like physicians, nurses, and allied clinicians have the required qualifications, training, and licenses to provide safe and effective patient care. This step is important for hospital compliance, quality assurance, and meeting regulatory standards.
It makes sure that access to a healthcare facility is restricted to qualified and verified professionals. To understand why credentialing and licensing work together, Understanding Medical License and Credentialing for Healthcare Professionals
Understand What Hospital Credentialing Involves
Hospital credentialing involves a comprehensive evaluation of the provider:
- Clinical competency
- Certification
- Professional training
- Licensure
- Educational background
There are two types of credentialing performed:
1. Initial Credentialing
Completed when a provider initially applies to join a hospital’s medical staff.
2. Recredentialing
It should be performed every 2 to 3 years to ensure continued competency, current licensure, and compliance. For in-depth information on each step, How to Simplify Hospital Credentialing for Faster Compliance
Gather Necessary Documentation and Information
A full and complete document set accelerates the credentialing procedure. Providers need:
- Government ID and background check
- Claims history or NPDB report
- Malpractice insurance certificate
- Professional reference
- Hospital affiliations
- Undated CV with complete work history
- Residency and fellowship certificate
- DEA registration
- Board certification
- Active medical license
Tips for Secure Document Management:
- Store credentials securely in cloud-based portals.
- Ensure consistent name standards for all files.
- Update the expired documents regulatory to avoid delays.
Complete the Credentialing Application
Complete and accurate applications can prevent unnecessary time and energy.
Steps to Fill Out Credentialing Forms Correctly
- Provide legal name and contact information as listed on your licenses.
- Ensure work history has no gaps; if it has, clarify it.
- List all the previous malpractice claims with full details.
- Review all hospital-specific privilege criteria and select the proper options.
- Double check all documents for accuracy and expiry dates.
Common Errors to Avoid:
- Omitting training dates
- Not listing all prior hospital affiliations
- Discrepancies between CV and application
- Leaving gaps in employment history
How to avoid delays, Common Challenges in Medical Licensing, and How Professional Services Can Help
Submit Credentials for Primary Source Verification
The credentialing or hospital team will verify all your submitted credentials directly from the original source. This includes:
- Malpractice carriers
- Previous employers or hospitals
- Certification board
- State licensing board
- Medical school
- Training programs
Tracking Verification Progress:
- Maintain all access to your application portal.
- Follow up on the pending verification.
- Respond fast to requests for clarification.
Undergo Credentialing Committee Review
Your file will be moved to the credentialing committee or medical staff committee once the verification is complete. They evaluate:
- Requested privileges
- Professional conduct
- Past performance
- Clinical competence
- Verified qualifications
The committee may approve, deny, or request any additional information. For compliance relevance of this step, The Role of Credentialing in Malpractice Risk Management
Receive Credentialing Decision and Appeal Process
The hospital will notify you of the result after review:
Approve: Privileges are granted for defined terms.
Denied: A Clear explanation will be given along with the next steps.
Conditional approval: Additional oversight or documents can be needed.
Providers can file an appeal, submit documentation, or request reconsideration on the basis of hospital bylaws if it is denied.
Maintain Ongoing Credentialing and Compliance
Credentialing does not end with approval. Hospitals need continuous monitoring of provider qualifications.
Providers must:
- Complete recredentialing every 2 to 3 years
- Maintain active and unrestricted licenses
- Update malpractice insurance
- Complete CME or continuing education
- Stay compliant with facility policy
- Respond to audits or update promptly
For long-term compliance support, How Professional Credentialing Services Can Streamline Your Practice Setup
Conclusion
Hospital credentialing is an important procedure that ensures patient safety, regulatory compliance, and high-quality healthcare delivery. A well-managed credentialing system reduces errors, speeds onboarding, and strengthens trust in the medical staff.
Discover medtigo’s professional credentialing services for a smooth, fast, and more compliant credentialing experience designed to support providers and healthcare facilities.
FAQs
1. How long does the hospital credentialing process typically take?
Credentialing takes 60 to 120 days on the basis of document completeness, verification speed, and hospital workflow.
2. What are the most common reasons for credentialing application delays or denials?
Common causes involve incomplete application, inconsistent work history, missing documents, malpractice discrepancies, or slow primary source responses.
3. How can providers expedite their credentialing approval?
They can submit all the documents early, avoid gaps in the work history, respond quickly to requests, and use professional credentialing services.
4. What happens if discrepancies are found during primary source verification?
The hospital may request clarification, place the application on hold, or forward the issue to the crediting committee for evaluation.
5. Is hospital credentialing required for telemedicine providers?
Yes, telemedicine clinicians must go for credentialing at each facility where they provide patient care, although some states allow credentialing by proxy.