Credentialing is important to bring new providers into clinical practice, yet it is one of the most frustrating parts of onboarding. Poor communication, unclear timeline, and repeated document requests contribute to delay, dissatisfaction, and early turnover. As organizations work to improve retention and deliver better onboarding experiences, communication and transparency are quickly becoming the main competitive advantages. This article has five practical strategies that can improve provider experience and accelerate credentialing.
Why Provider Experience Matters in Credentialing
Credentialing has a direct effect on operational and morale efficiency. Surveys show that around 40% of providers detect credentialing delays as their top frustration, which may lead to onboarding setbacks and lost clinical time. When the process is smooth, providers are more likely to stay engaged, recommend the organization to peers, and speak positively about their onboarding experience. Many hospitals are shifting from traditional process-heavy methods to a provider-centered model, which values support, communication, and clarity at every stage.
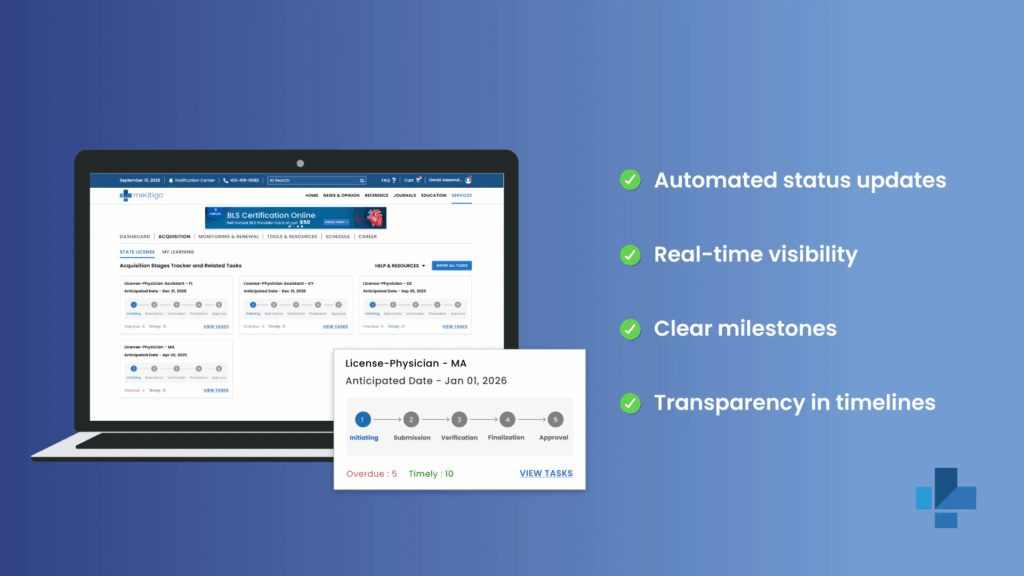
Strategy 1: Automated Status Updates and Dashboards
Real-time visibility is one of the most effective ways to decrease anxiety around credentialing. The self-service portal helps providers track exactly where their application stands without the necessity to send repeated emails. These platforms offer a timeline view of progress, highlight pending tasks, and send automatic alerts when documents are needed or milestones are met. Providers get immediate clarity, and administrative teams spend less time fielding status inquiries.
Strategy 2: Dedicated Provider Liaisons
Assigning a single point of contact creates a more reliable and personal experience, specifically for complex cases involving many states, telehealth, or locum tenens arrangements. A dedicated liaison ensures consistent communication, resolves issues sooner, and helps providers feel supported instead of lost in the bureaucratic process. Many telehealth programs rely on this model because it streamlines workflows and reduces confusion.
Strategy 3: Transparent Timelines and Expectation Setting
Providers feel frustrated simply because they do not know what to expect. Publishing average timelines, noting how long each credentialing phase takes, and providing weekly check-ins, even if nothing has changed. It helps to eliminate uncertainty. Orientation calls at the start of the process can walk providers through the full journey, helping them understand verification steps, committee reviews, and any potential bottlenecks.
Strategy 4: Proactive Document Management Communication
Any missing or outdated documents can lead to delays. It is better to give a clear checklist at the beginning, combined with easy digital upload options and friendly reminders as deadlines approach. It makes sure that providers stay ahead of requirements. Mobile upload tools are specifically helpful for busy clinicians who need flexibility.
Strategy 5: Feedback Loops and Continuous Improvement
Collecting direct feedback from the newly credentialed providers helps organizations detect communication gaps, unclear steps, pr recurring frustrations. Short post-credentialing surveys or quick feedback requests allow hospitals to refine the experience. Over time, these insights lead to faster and more reliable processes.
Technology and Communication Integration
Credentialing improves significantly when technology streamlines communication. A single portal that houses status updates, document management, message tools, and support channels to remove the need for many systems or confusing email chains. AI-powered chatbots can answer routine questions instantly while integrating with HER or EMR systems to reduce duplicate data entry and improve accuracy. Medtigo’s credentialing platform has all these capabilities together, which offer a fluid, provider-centered experience that uses efficiency and transparency.
Conclusion
Communication and transparency are no longer an option in modern credentialing; they are important. Organizations that clearly share timelines, maintain consistent communication, and use technology to enhance visibility see credentialing completed up to 30% faster, with providers reporting high satisfaction and few frustrations.
If your organization is ready to transform credentialing workflow, Medtigo’s platform delivers an intuitive, provider-focused solution designed to increase both experience and speed.
FAQs
1. What KPIs should hospitals track to measure provider credentialing satisfaction?
Turnaround time, provider satisfaction score, response time, and rates of missing documentation are among the most valuable metrics.
2. How should organizations respond to provider complaints during credentialing delays?
Acknowledge concerns promptly, explain the cause, offer revised timelines, and ensure they have a single contact for follow-up.
4. What is the best communication cadence during credentialing?
Weekly updates work well with additional messages for main milestones or document needs.
5. Is it helpful to share credentialing committee timelines with providers?
Yes, transparency helps providers plan and reduces unnecessary follow-up.
5. How does Medtigo’s liaison service improve the provider experience?
By offering personalized guidance, quicker issue resolution, and consistent communication throughout the credentialing process.