Introduction
Credentialing is an essential component to improve patient safety, healthcare quality, and regulatory compliance. It makes sure that healthcare providers and organizations meet established professional standards before providing care, billing insurers, or practicing in a facility.
Credentialing is not a single process; it comprises three different but interconnected types in today’s complex healthcare environment. Understanding these types of credentialing helps providers, healthcare organizations, and administrators to avoid delays, compliance risks, and revenue disruptions.
This blog explains three main types of credentialing: provider, payer, and facility or hospital credentialing, and why each one matters.
For a more comprehensive perspective:
How to Simplify Hospital Credentialing for Faster Compliance
Provider Credentialing
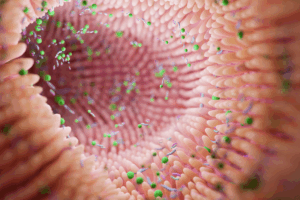
Provider credentialing focuses on verifying the qualifications and professional background of individual healthcare providers. This process confirms that the provider is properly licensed, trained, and competent to deliver patient care.
What is verified during provider credentialing:
- Identity and education history
- Residency, fellowship, and training programs
- State medical or professional licenses
- Board certifications
- Work history and references
- Malpractice insurance and claims history
- Disciplinary actions or sanctions
Provider credentialing is conducted by healthcare systems, hospitals, credentialing organizations, or medical staffing companies by using primary source verifications. The purpose is to protect patients, meet regulatory standards, and reduce institutional risk.
Provider credentialing serves as the foundation for licensing and privileging decisions.
Learn more from
How Licensing Relies on Credentialing and Primary Source Verification
Payer Credentialing (Insurance Credentialing)
Payer credentialing, also called insurance credentialing or provider enrollment, is the process of enrolling healthcare providers with insurance companies, so they can bill for services and get reimbursement.
Payer credentialing mainly focuses on administrative and financial eligibility, while provider credentialing focuses on clinical qualifications.
Key elements of payer credentialing include:
- Enrollment with private insurers, Medicare, and Medicaid
- Completion and maintenance of a CAQH profile
- Submission of payer-specific applications and contracts
- Verification of licensure, malpractice coverage, and practice locations
Providers are unable to get payment even if they are fully licensed and clinically credentialed without successful payer credentialing. Each payer has unique requirements, timelines, and recredentialing cycles, which makes this process specifically complex.
For more guidance on staffing and expertise, see What Type of Credentialing Specialist Should I Hire?
Facility or Hospital Credentialing (Privileging)
Facility or hospital credentialing, referred to as privileging, determines what specific clinical services a provider is authorized to perform in a healthcare facility. Privileging goes beyond verifying credentials; it assesses whether a provider has experience, training, and has shown competence to perform specific procedures or services.
The privileging process includes:
Review by medical staff committees
Evaluation of training and case experience
Approval by hospital governing bodies
Ongoing performance monitoring and reappointment
This type of credentialing is important for patient safety, legal protection, and accreditation compliance. It is very important for nontraditional care models like telemedicine.
For more information, see How Hospitals Handle Credentialing for Telehealth Providers.
Conclusion
These three types of credentialing provider credentialing, payer credentialing, and facility or hospital credentialing each serve a different purpose, but none can replace the others. They form a comprehensive system that supports quality care, regulatory compliance, and financial stability.
Healthcare organizations that develop strong processes in all three credentialing types are better positioned to decrease risk, improve efficiency, and support providers’ success.
Medtigo’s credentialing services help organizations to manage all aspects of credentialing through a centralized, compliant, and scalable approach.
Check the details here
or contact support@medtigo.com
FAQs
1. Can one credentialing type substitute for another, or are all required?
No, each type serves a different function, and most providers and organizations require all three.
2. How often should each type of credentialing be updated or renewed?
Provider and hospital credentialing typically occur every two to three years, while payer credentialing differs by insurer and program.
3. What common challenges differentiate each type of credentialing?
Provider credentialing often involves verification delays, payer credentialing impacts reimbursement timelines, and hospital privileging can be committee-driven and time-intensive.
4. How does technology improve efficiency across these different credentialing types?
Credentialing software and managed services reduce manual errors, improve tracking, and streamline renewals and documentation.
5. Are there providers exempt from certain types of credentialing?
Some non-billing or non-clinical roles may not require payer credentialing, but licensure and facility requirements apply in most cases.