Human Doctor or AI? Understanding Patient Preferences in AI-Assisted Medical Care
March 6, 2026
Background
Creutzfeldt-Jakob Disease (CJD) is a rare, degenerative, and fatal neurological disorder that belongs to a group of conditions known as prion diseases. Prion diseases are characterized by the accumulation and misfolding of abnormal prion proteins in the brain, leading to progressive damage and dysfunction of brain cells. CJD affects about 1 in every 1 million individuals worldwide, with no specific age, gender, or geographic predilection.
There are different forms of CJD, including sporadic, familial, and acquired variants. The most common form is sporadic CJD, which occurs spontaneously without any known cause. Sporadic CJD accounts for about 85% of all cases. Familial CJD is caused by mutations in the PRNP gene and is inherited in an autosomal dominant pattern. Acquired CJD can result from exposure to infected brain or nervous system tissue, typically through medical procedures or contaminated surgical instruments.
Epidemiology
Creutzfeldt-Jakob Disease (CJD) is a rare neurological disorder with a low prevalence in the general population. The epidemiology of CJD varies based on different forms of the disease and geographic regions. Here are some key points regarding the epidemiology of CJD:
Anatomy
Pathophysiology
Creutzfeldt-Jakob Disease (CJD) is a neurodegenerative disorder that belongs to a group of diseases known as transmissible spongiform encephalopathies (TSEs) or prion diseases. The pathophysiology of CJD involves the accumulation and misfolding of abnormal prion proteins in the brain, leading to the progressive destruction of brain tissue and neurological dysfunction. Here is an overview of the key aspects of the pathophysiology of CJD:
Prion Proteins: Prion diseases are caused by the misfolding of normal cellular prion proteins (PrP^C) into an abnormal isoform called scrapie prion protein (PrP^Sc). This isoform has a different conformation and is highly resistant to degradation by normal cellular processes.
Prion Propagation: The abnormal PrP^Sc isoform can induce the misfolding of normal PrP^C proteins into the pathological isoform. This conversion process leads to the accumulation of PrP^Sc in the brain, forming insoluble aggregates and fibrils.
Neurotoxicity and Neurodegeneration: The accumulation of abnormal PrP^Sc protein in the brain disrupts normal cellular function and leads to neurotoxicity. The exact mechanisms underlying the neurotoxic effects of PrP^Sc are not fully understood, but several hypotheses have been proposed, including oxidative stress, disruption of calcium homeostasis, and activation of inflammatory responses. These processes contribute to the progressive degeneration and death of neurons in the affected areas of the brain.
Spongiform Changes: One characteristic feature of CJD is the presence of spongiform changes in the brain tissue. These changes are caused by the loss of neuronal cells, resulting in the formation of small vacuoles within the neuropil. The accumulation of PrP^Sc is thought to contribute to the development of these spongiform changes.
Inflammatory Response: The presence of abnormal PrP^Sc protein and the neurodegenerative process in CJD can trigger an inflammatory response in the brain. Activated microglia and astrocytes release inflammatory cytokines and other immune molecules, leading to further tissue damage and inflammation.
Spread of Prions: The misfolded PrP^Sc protein has the ability to spread and propagate within the brain, potentially moving from one region to another. This spread can contribute to the widespread neuronal damage observed in CJD.
The pathophysiology of CJD is complex and involves intricate interactions between misfolded prion proteins, neurotoxicity, inflammation, and neuronal degeneration. The progressive accumulation and spread of abnormal PrP^Sc protein disrupt normal cellular function and ultimately lead to the characteristic clinical manifestations and severe neurological impairment seen in CJD.
Etiology
Creutzfeldt-Jakob Disease (CJD) is caused by the accumulation and misfolding of abnormal prion proteins in the brain. These abnormal prions are the etiological agents responsible for the development of the disease. Here are the key aspects regarding the etiology of CJD:
Abnormal Prions: The primary etiological factor in CJD is the presence of abnormal isoforms of the prion protein (PrP). Prions are misfolded, infectious proteins that can induce the misfolding of normal cellular prion proteins into the abnormal isoform. The abnormal prions are highly stable and resistant to degradation by normal cellular processes.
Sporadic CJD: The majority of CJD cases (about 85%) are sporadic, meaning they occur spontaneously without any apparent cause or predisposing factors. In sporadic CJD, the origin of the abnormal prions is not fully understood. It is believed to involve spontaneous misfolding of normal cellular prion proteins, resulting in the development of the disease.
Genetic Mutations: Some cases of CJD are caused by genetic mutations in the PRNP gene, which encodes the prion protein. These mutations lead to the production of abnormal prion proteins or increased susceptibility to the misfolding process. Familial forms of CJD result from these inherited mutations in an autosomal dominant pattern. However, familial cases account for a smaller proportion of overall CJD cases (about 10-15%).
Acquired CJD: Acquired forms of CJD can occur due to exposure to infected brain or nervous system tissue. The most well-known example of acquired CJD is variant CJD (vCJD), which is associated with consumption of prion-contaminated meat products, particularly beef, from cattle affected by bovine spongiform encephalopathy (BSE or “mad cow” disease). Other forms of acquired CJD, known as iatrogenic CJD, can result from medical procedures involving infected tissues or contaminated surgical instruments.
Transmission: CJD is not considered a contagious disease in the usual sense. It does not spread through casual contact or respiratory droplets. However, transmission can occur through direct exposure to infected tissues or through certain medical procedures. The transmission routes for acquired and iatrogenic CJD are well-documented, while the transmission route for sporadic and familial CJD remains uncertain.
The etiology of CJD is primarily linked to the misfolding and accumulation of abnormal prion proteins in the brain. While the exact mechanisms underlying spontaneous misfolding or genetic mutations leading to abnormal prion formation are not fully understood, extensive research has provided valuable insights into the role of prions in the development of CJD.
Genetics
Prognostic Factors
The prognosis for individuals with CJD is generally poor, and the disease typically leads to severe disability and death within a relatively short period of time. Here are key aspects of the prognosis in CJD:
Rapid Disease Progression: CJD is characterized by a rapid progression of symptoms over weeks to months. As the disease advances, individuals experience worsening cognitive decline, neurological deficits, and functional impairment. The duration of illness varies, but most individuals succumb to the disease within a year of symptom onset.
Neurological Decline: CJD affects various areas of the brain, leading to a wide range of neurological symptoms. These symptoms include cognitive impairment, memory loss, behavioral changes, motor abnormalities, visual disturbances, and difficulties with coordination and balance. The neurological decline in CJD can result in profound disability, with individuals becoming bedridden and requiring assistance with activities of daily living.
Lack of Effective Treatment: Currently, there is no known cure for CJD, and no specific treatment can halt or reverse the disease progression. While supportive care measures can help manage symptoms and improve comfort, they do not alter the underlying course of the disease.
Variable Disease Duration: The duration of illness can vary among individuals with CJD. Sporadic and genetic forms of CJD often have a more rapid progression compared to acquired forms, such as variant CJD (vCJD). However, the disease course is generally characterized by a relentless decline.
Impact on Quality of Life: CJD significantly affects the quality of life of individuals and their families. The rapid decline in neurological function and the loss of independence and cognitive abilities can be emotionally challenging for both the affected individual and their loved ones.
Fatal Outcome: CJD is ultimately fatal, with most individuals succumbing to the disease within months of symptom onset. Death is typically due to complications associated with severe neurological dysfunction, such as respiratory failure or infections.
Clinical History
Clinical history
The clinical history of Creutzfeldt-Jakob Disease (CJD) typically involves the progressive development of neurological symptoms over a relatively short period of time. The duration of symptoms can vary but is usually measured in months rather than years. Here are some key aspects of the clinical history of CJD:
Rapidly Progressive Cognitive Decline: One of the hallmark features of CJD is the rapid onset and progressive decline in cognitive function. Individuals may experience memory loss, difficulty with attention and concentration, confusion, disorientation, and problems with language and speech. These cognitive changes tend to worsen rapidly over weeks to months.
Neurological Symptoms: CJD can also involve a variety of neurological symptoms, which may vary among individuals. These symptoms can include changes in behavior and personality, mood disturbances, anxiety, depression, and irritability. In addition, individuals may experience difficulties with coordination and balance, muscle stiffness, involuntary movements (such as myoclonus or chorea), and sensory abnormalities.
Visual Disturbances: Visual symptoms are common in CJD and may include blurred vision, visual hallucinations, and visual field deficits. These disturbances can range from subtle changes to significant visual impairment.
Sleep Disturbances: Sleep abnormalities, including disrupted sleep patterns, excessive daytime sleepiness, and rapid eye movement (REM) sleep behavior disorder, can occur in some individuals with CJD.
Neurological Examination Findings: The neurological examination may reveal various abnormalities depending on the stage of the disease. These can include cognitive impairment, changes in behavior and personality, abnormalities in muscle tone and movement, abnormal eye movements, and signs of cerebellar dysfunction.
Absence of Systemic Features: CJD primarily affects the central nervous system and does not typically present with systemic symptoms such as fever or weight loss. The absence of systemic manifestations helps to distinguish CJD from other conditions.
Physical Examination
Physical examination
The physical examination of an individual suspected to have Creutzfeldt-Jakob Disease (CJD) focuses on assessing neurological findings and other associated signs. The examination aims to evaluate the presence and severity of neurological deficits and exclude other possible causes for the symptoms. Here are key aspects of the physical examination in CJD:
Neurological Examination:
Extra neurological Findings:
Systemic Examination:
Age group
Associated comorbidity
Associated activity
Acuity of presentation
Differential Diagnoses
Differential diagnosis
Creutzfeldt-Jakob Disease (CJD) is a rare neurological disorder with symptoms that can overlap with other conditions. Therefore, it is important to consider a range of differential diagnoses when evaluating individuals suspected of having CJD. Here are some key conditions to consider in the differential diagnosis of CJD:
Other Prion Diseases: Other prion diseases can present with similar clinical features to CJD. These include variant Creutzfeldt-Jakob Disease (vCJD), which is associated with bovine spongiform encephalopathy (BSE or “mad cow” disease), and other rare prion diseases such as Gerstmann-Sträussler-Scheinker syndrome (GSS) and fatal familial insomnia (FFI).
Other Neurodegenerative Disorders: Several other neurodegenerative disorders may exhibit clinical features similar to CJD. These include Alzheimer’s disease, frontotemporal dementia, Lewy body dementia, and progressive supranuclear palsy. Distinguishing features and specific diagnostic criteria can aid in differentiating these conditions from CJD.
Autoimmune Encephalitis: Autoimmune encephalitis, such as anti-NMDA receptor encephalitis or Hashimoto’s encephalopathy, can present with rapidly progressive cognitive decline, behavioral changes, and neurological symptoms that can mimic CJD. Clinical history, specific antibody testing, and neuroimaging findings may help differentiate autoimmune encephalitis from CJD.
Metabolic Disorders: Certain metabolic disorders, such as Wilson’s disease, mitochondrial disorders, and other lysosomal storage disorders, may have overlapping neurological features with CJD. Laboratory tests, genetic testing, and imaging studies can assist in differentiating these conditions from CJD.
Paraneoplastic Syndromes: Paraneoplastic syndromes associated with certain cancers, such as paraneoplastic limbic encephalitis, can manifest with cognitive and neurological symptoms resembling CJD. Close evaluation of clinical history, tumor markers, and appropriate imaging and laboratory investigations are important in making the distinction.
Infectious Diseases: In rare cases, infectious diseases that affect the central nervous system, such as viral encephalitis or prion diseases other than CJD, can present with similar symptoms. Detailed clinical history, cerebrospinal fluid analysis, and appropriate diagnostic testing can help differentiate these conditions from CJD.
Psychiatric Disorders: Certain psychiatric disorders, such as psychosis or rapidly progressive dementia associated with severe depression, may share some features with CJD. Psychiatric evaluation, longitudinal assessment, and response to appropriate treatment interventions are essential in distinguishing psychiatric disorders from CJD.
Distinguishing CJD from other conditions can be challenging, and a comprehensive evaluation is necessary. This typically includes a detailed medical history, neurological examination, neuropsychological testing, neuroimaging (such as MRI), electroencephalogram (EEG), cerebrospinal fluid analysis, and occasionally brain biopsy or genetic testing. Consultation with neurologists, neuropsychiatrists, or specialists in prion diseases is recommended for accurate diagnosis and appropriate management.
Laboratory Studies
Imaging Studies
Procedures
Histologic Findings
Staging
Treatment Paradigm
Currently, there is no known cure or specific treatment that can halt or reverse the progression of Creutzfeldt-Jakob Disease (CJD). The management of CJD primarily focuses on providing supportive care to improve quality of life and alleviate symptoms. Treatment is typically palliative and aims to address the specific needs and complications associated with the disease. Here are some aspects of the treatment approach for CJD:
Symptom Management: Various medications may be used to manage specific symptoms and improve the individual’s comfort. These may include medications to control muscle stiffness (spasticity) or myoclonus (sudden muscle jerks), medications to address mood disturbances or psychiatric symptoms, and sleep aids to manage sleep disturbances.
Nutritional Support: As the disease progresses, individuals with CJD may experience difficulty swallowing (dysphagia) and weight loss. Nutritional support, such as modified diets or feeding tubes, may be necessary to ensure adequate nutrition and hydration.
Pain Management: Pain can be associated with CJD, and appropriate pain management strategies, including medications or non-pharmacological approaches, should be implemented to alleviate discomfort.
Supportive Care: Comprehensive supportive care is crucial for individuals with CJD. This involves addressing their physical, emotional, and psychological needs. Supportive care may include physical therapy to maintain mobility and prevent contractures, occupational therapy to assist with daily activities, and speech therapy to manage speech and swallowing difficulties.
End-of-Life Care: CJD is a progressive and ultimately fatal disease. As the disease advances, individuals may require end-of-life care, including hospice or palliative care services. These services focus on maximizing comfort, providing emotional support to individuals and their families, and ensuring a dignified and peaceful end-of-life experience.
by Stage
by Modality
Chemotherapy
Radiation Therapy
Surgical Interventions
Hormone Therapy
Immunotherapy
Hyperthermia
Photodynamic Therapy
Stem Cell Transplant
Targeted Therapy
Palliative Care
Medication
Future Trends
References
https://www.ncbi.nlm.nih.gov/books/NBK507860/
Creutzfeldt-Jakob Disease (CJD) is a rare, degenerative, and fatal neurological disorder that belongs to a group of conditions known as prion diseases. Prion diseases are characterized by the accumulation and misfolding of abnormal prion proteins in the brain, leading to progressive damage and dysfunction of brain cells. CJD affects about 1 in every 1 million individuals worldwide, with no specific age, gender, or geographic predilection.
There are different forms of CJD, including sporadic, familial, and acquired variants. The most common form is sporadic CJD, which occurs spontaneously without any known cause. Sporadic CJD accounts for about 85% of all cases. Familial CJD is caused by mutations in the PRNP gene and is inherited in an autosomal dominant pattern. Acquired CJD can result from exposure to infected brain or nervous system tissue, typically through medical procedures or contaminated surgical instruments.
Creutzfeldt-Jakob Disease (CJD) is a rare neurological disorder with a low prevalence in the general population. The epidemiology of CJD varies based on different forms of the disease and geographic regions. Here are some key points regarding the epidemiology of CJD:
Creutzfeldt-Jakob Disease (CJD) is a neurodegenerative disorder that belongs to a group of diseases known as transmissible spongiform encephalopathies (TSEs) or prion diseases. The pathophysiology of CJD involves the accumulation and misfolding of abnormal prion proteins in the brain, leading to the progressive destruction of brain tissue and neurological dysfunction. Here is an overview of the key aspects of the pathophysiology of CJD:
Prion Proteins: Prion diseases are caused by the misfolding of normal cellular prion proteins (PrP^C) into an abnormal isoform called scrapie prion protein (PrP^Sc). This isoform has a different conformation and is highly resistant to degradation by normal cellular processes.
Prion Propagation: The abnormal PrP^Sc isoform can induce the misfolding of normal PrP^C proteins into the pathological isoform. This conversion process leads to the accumulation of PrP^Sc in the brain, forming insoluble aggregates and fibrils.
Neurotoxicity and Neurodegeneration: The accumulation of abnormal PrP^Sc protein in the brain disrupts normal cellular function and leads to neurotoxicity. The exact mechanisms underlying the neurotoxic effects of PrP^Sc are not fully understood, but several hypotheses have been proposed, including oxidative stress, disruption of calcium homeostasis, and activation of inflammatory responses. These processes contribute to the progressive degeneration and death of neurons in the affected areas of the brain.
Spongiform Changes: One characteristic feature of CJD is the presence of spongiform changes in the brain tissue. These changes are caused by the loss of neuronal cells, resulting in the formation of small vacuoles within the neuropil. The accumulation of PrP^Sc is thought to contribute to the development of these spongiform changes.
Inflammatory Response: The presence of abnormal PrP^Sc protein and the neurodegenerative process in CJD can trigger an inflammatory response in the brain. Activated microglia and astrocytes release inflammatory cytokines and other immune molecules, leading to further tissue damage and inflammation.
Spread of Prions: The misfolded PrP^Sc protein has the ability to spread and propagate within the brain, potentially moving from one region to another. This spread can contribute to the widespread neuronal damage observed in CJD.
The pathophysiology of CJD is complex and involves intricate interactions between misfolded prion proteins, neurotoxicity, inflammation, and neuronal degeneration. The progressive accumulation and spread of abnormal PrP^Sc protein disrupt normal cellular function and ultimately lead to the characteristic clinical manifestations and severe neurological impairment seen in CJD.
Creutzfeldt-Jakob Disease (CJD) is caused by the accumulation and misfolding of abnormal prion proteins in the brain. These abnormal prions are the etiological agents responsible for the development of the disease. Here are the key aspects regarding the etiology of CJD:
Abnormal Prions: The primary etiological factor in CJD is the presence of abnormal isoforms of the prion protein (PrP). Prions are misfolded, infectious proteins that can induce the misfolding of normal cellular prion proteins into the abnormal isoform. The abnormal prions are highly stable and resistant to degradation by normal cellular processes.
Sporadic CJD: The majority of CJD cases (about 85%) are sporadic, meaning they occur spontaneously without any apparent cause or predisposing factors. In sporadic CJD, the origin of the abnormal prions is not fully understood. It is believed to involve spontaneous misfolding of normal cellular prion proteins, resulting in the development of the disease.
Genetic Mutations: Some cases of CJD are caused by genetic mutations in the PRNP gene, which encodes the prion protein. These mutations lead to the production of abnormal prion proteins or increased susceptibility to the misfolding process. Familial forms of CJD result from these inherited mutations in an autosomal dominant pattern. However, familial cases account for a smaller proportion of overall CJD cases (about 10-15%).
Acquired CJD: Acquired forms of CJD can occur due to exposure to infected brain or nervous system tissue. The most well-known example of acquired CJD is variant CJD (vCJD), which is associated with consumption of prion-contaminated meat products, particularly beef, from cattle affected by bovine spongiform encephalopathy (BSE or “mad cow” disease). Other forms of acquired CJD, known as iatrogenic CJD, can result from medical procedures involving infected tissues or contaminated surgical instruments.
Transmission: CJD is not considered a contagious disease in the usual sense. It does not spread through casual contact or respiratory droplets. However, transmission can occur through direct exposure to infected tissues or through certain medical procedures. The transmission routes for acquired and iatrogenic CJD are well-documented, while the transmission route for sporadic and familial CJD remains uncertain.
The etiology of CJD is primarily linked to the misfolding and accumulation of abnormal prion proteins in the brain. While the exact mechanisms underlying spontaneous misfolding or genetic mutations leading to abnormal prion formation are not fully understood, extensive research has provided valuable insights into the role of prions in the development of CJD.
The prognosis for individuals with CJD is generally poor, and the disease typically leads to severe disability and death within a relatively short period of time. Here are key aspects of the prognosis in CJD:
Rapid Disease Progression: CJD is characterized by a rapid progression of symptoms over weeks to months. As the disease advances, individuals experience worsening cognitive decline, neurological deficits, and functional impairment. The duration of illness varies, but most individuals succumb to the disease within a year of symptom onset.
Neurological Decline: CJD affects various areas of the brain, leading to a wide range of neurological symptoms. These symptoms include cognitive impairment, memory loss, behavioral changes, motor abnormalities, visual disturbances, and difficulties with coordination and balance. The neurological decline in CJD can result in profound disability, with individuals becoming bedridden and requiring assistance with activities of daily living.
Lack of Effective Treatment: Currently, there is no known cure for CJD, and no specific treatment can halt or reverse the disease progression. While supportive care measures can help manage symptoms and improve comfort, they do not alter the underlying course of the disease.
Variable Disease Duration: The duration of illness can vary among individuals with CJD. Sporadic and genetic forms of CJD often have a more rapid progression compared to acquired forms, such as variant CJD (vCJD). However, the disease course is generally characterized by a relentless decline.
Impact on Quality of Life: CJD significantly affects the quality of life of individuals and their families. The rapid decline in neurological function and the loss of independence and cognitive abilities can be emotionally challenging for both the affected individual and their loved ones.
Fatal Outcome: CJD is ultimately fatal, with most individuals succumbing to the disease within months of symptom onset. Death is typically due to complications associated with severe neurological dysfunction, such as respiratory failure or infections.
Clinical history
The clinical history of Creutzfeldt-Jakob Disease (CJD) typically involves the progressive development of neurological symptoms over a relatively short period of time. The duration of symptoms can vary but is usually measured in months rather than years. Here are some key aspects of the clinical history of CJD:
Rapidly Progressive Cognitive Decline: One of the hallmark features of CJD is the rapid onset and progressive decline in cognitive function. Individuals may experience memory loss, difficulty with attention and concentration, confusion, disorientation, and problems with language and speech. These cognitive changes tend to worsen rapidly over weeks to months.
Neurological Symptoms: CJD can also involve a variety of neurological symptoms, which may vary among individuals. These symptoms can include changes in behavior and personality, mood disturbances, anxiety, depression, and irritability. In addition, individuals may experience difficulties with coordination and balance, muscle stiffness, involuntary movements (such as myoclonus or chorea), and sensory abnormalities.
Visual Disturbances: Visual symptoms are common in CJD and may include blurred vision, visual hallucinations, and visual field deficits. These disturbances can range from subtle changes to significant visual impairment.
Sleep Disturbances: Sleep abnormalities, including disrupted sleep patterns, excessive daytime sleepiness, and rapid eye movement (REM) sleep behavior disorder, can occur in some individuals with CJD.
Neurological Examination Findings: The neurological examination may reveal various abnormalities depending on the stage of the disease. These can include cognitive impairment, changes in behavior and personality, abnormalities in muscle tone and movement, abnormal eye movements, and signs of cerebellar dysfunction.
Absence of Systemic Features: CJD primarily affects the central nervous system and does not typically present with systemic symptoms such as fever or weight loss. The absence of systemic manifestations helps to distinguish CJD from other conditions.
Physical examination
The physical examination of an individual suspected to have Creutzfeldt-Jakob Disease (CJD) focuses on assessing neurological findings and other associated signs. The examination aims to evaluate the presence and severity of neurological deficits and exclude other possible causes for the symptoms. Here are key aspects of the physical examination in CJD:
Neurological Examination:
Extra neurological Findings:
Systemic Examination:
Differential diagnosis
Creutzfeldt-Jakob Disease (CJD) is a rare neurological disorder with symptoms that can overlap with other conditions. Therefore, it is important to consider a range of differential diagnoses when evaluating individuals suspected of having CJD. Here are some key conditions to consider in the differential diagnosis of CJD:
Other Prion Diseases: Other prion diseases can present with similar clinical features to CJD. These include variant Creutzfeldt-Jakob Disease (vCJD), which is associated with bovine spongiform encephalopathy (BSE or “mad cow” disease), and other rare prion diseases such as Gerstmann-Sträussler-Scheinker syndrome (GSS) and fatal familial insomnia (FFI).
Other Neurodegenerative Disorders: Several other neurodegenerative disorders may exhibit clinical features similar to CJD. These include Alzheimer’s disease, frontotemporal dementia, Lewy body dementia, and progressive supranuclear palsy. Distinguishing features and specific diagnostic criteria can aid in differentiating these conditions from CJD.
Autoimmune Encephalitis: Autoimmune encephalitis, such as anti-NMDA receptor encephalitis or Hashimoto’s encephalopathy, can present with rapidly progressive cognitive decline, behavioral changes, and neurological symptoms that can mimic CJD. Clinical history, specific antibody testing, and neuroimaging findings may help differentiate autoimmune encephalitis from CJD.
Metabolic Disorders: Certain metabolic disorders, such as Wilson’s disease, mitochondrial disorders, and other lysosomal storage disorders, may have overlapping neurological features with CJD. Laboratory tests, genetic testing, and imaging studies can assist in differentiating these conditions from CJD.
Paraneoplastic Syndromes: Paraneoplastic syndromes associated with certain cancers, such as paraneoplastic limbic encephalitis, can manifest with cognitive and neurological symptoms resembling CJD. Close evaluation of clinical history, tumor markers, and appropriate imaging and laboratory investigations are important in making the distinction.
Infectious Diseases: In rare cases, infectious diseases that affect the central nervous system, such as viral encephalitis or prion diseases other than CJD, can present with similar symptoms. Detailed clinical history, cerebrospinal fluid analysis, and appropriate diagnostic testing can help differentiate these conditions from CJD.
Psychiatric Disorders: Certain psychiatric disorders, such as psychosis or rapidly progressive dementia associated with severe depression, may share some features with CJD. Psychiatric evaluation, longitudinal assessment, and response to appropriate treatment interventions are essential in distinguishing psychiatric disorders from CJD.
Distinguishing CJD from other conditions can be challenging, and a comprehensive evaluation is necessary. This typically includes a detailed medical history, neurological examination, neuropsychological testing, neuroimaging (such as MRI), electroencephalogram (EEG), cerebrospinal fluid analysis, and occasionally brain biopsy or genetic testing. Consultation with neurologists, neuropsychiatrists, or specialists in prion diseases is recommended for accurate diagnosis and appropriate management.
Currently, there is no known cure or specific treatment that can halt or reverse the progression of Creutzfeldt-Jakob Disease (CJD). The management of CJD primarily focuses on providing supportive care to improve quality of life and alleviate symptoms. Treatment is typically palliative and aims to address the specific needs and complications associated with the disease. Here are some aspects of the treatment approach for CJD:
Symptom Management: Various medications may be used to manage specific symptoms and improve the individual’s comfort. These may include medications to control muscle stiffness (spasticity) or myoclonus (sudden muscle jerks), medications to address mood disturbances or psychiatric symptoms, and sleep aids to manage sleep disturbances.
Nutritional Support: As the disease progresses, individuals with CJD may experience difficulty swallowing (dysphagia) and weight loss. Nutritional support, such as modified diets or feeding tubes, may be necessary to ensure adequate nutrition and hydration.
Pain Management: Pain can be associated with CJD, and appropriate pain management strategies, including medications or non-pharmacological approaches, should be implemented to alleviate discomfort.
Supportive Care: Comprehensive supportive care is crucial for individuals with CJD. This involves addressing their physical, emotional, and psychological needs. Supportive care may include physical therapy to maintain mobility and prevent contractures, occupational therapy to assist with daily activities, and speech therapy to manage speech and swallowing difficulties.
End-of-Life Care: CJD is a progressive and ultimately fatal disease. As the disease advances, individuals may require end-of-life care, including hospice or palliative care services. These services focus on maximizing comfort, providing emotional support to individuals and their families, and ensuring a dignified and peaceful end-of-life experience.
https://www.ncbi.nlm.nih.gov/books/NBK507860/
Creutzfeldt-Jakob Disease (CJD) is a rare, degenerative, and fatal neurological disorder that belongs to a group of conditions known as prion diseases. Prion diseases are characterized by the accumulation and misfolding of abnormal prion proteins in the brain, leading to progressive damage and dysfunction of brain cells. CJD affects about 1 in every 1 million individuals worldwide, with no specific age, gender, or geographic predilection.
There are different forms of CJD, including sporadic, familial, and acquired variants. The most common form is sporadic CJD, which occurs spontaneously without any known cause. Sporadic CJD accounts for about 85% of all cases. Familial CJD is caused by mutations in the PRNP gene and is inherited in an autosomal dominant pattern. Acquired CJD can result from exposure to infected brain or nervous system tissue, typically through medical procedures or contaminated surgical instruments.
Creutzfeldt-Jakob Disease (CJD) is a rare neurological disorder with a low prevalence in the general population. The epidemiology of CJD varies based on different forms of the disease and geographic regions. Here are some key points regarding the epidemiology of CJD:
Creutzfeldt-Jakob Disease (CJD) is a neurodegenerative disorder that belongs to a group of diseases known as transmissible spongiform encephalopathies (TSEs) or prion diseases. The pathophysiology of CJD involves the accumulation and misfolding of abnormal prion proteins in the brain, leading to the progressive destruction of brain tissue and neurological dysfunction. Here is an overview of the key aspects of the pathophysiology of CJD:
Prion Proteins: Prion diseases are caused by the misfolding of normal cellular prion proteins (PrP^C) into an abnormal isoform called scrapie prion protein (PrP^Sc). This isoform has a different conformation and is highly resistant to degradation by normal cellular processes.
Prion Propagation: The abnormal PrP^Sc isoform can induce the misfolding of normal PrP^C proteins into the pathological isoform. This conversion process leads to the accumulation of PrP^Sc in the brain, forming insoluble aggregates and fibrils.
Neurotoxicity and Neurodegeneration: The accumulation of abnormal PrP^Sc protein in the brain disrupts normal cellular function and leads to neurotoxicity. The exact mechanisms underlying the neurotoxic effects of PrP^Sc are not fully understood, but several hypotheses have been proposed, including oxidative stress, disruption of calcium homeostasis, and activation of inflammatory responses. These processes contribute to the progressive degeneration and death of neurons in the affected areas of the brain.
Spongiform Changes: One characteristic feature of CJD is the presence of spongiform changes in the brain tissue. These changes are caused by the loss of neuronal cells, resulting in the formation of small vacuoles within the neuropil. The accumulation of PrP^Sc is thought to contribute to the development of these spongiform changes.
Inflammatory Response: The presence of abnormal PrP^Sc protein and the neurodegenerative process in CJD can trigger an inflammatory response in the brain. Activated microglia and astrocytes release inflammatory cytokines and other immune molecules, leading to further tissue damage and inflammation.
Spread of Prions: The misfolded PrP^Sc protein has the ability to spread and propagate within the brain, potentially moving from one region to another. This spread can contribute to the widespread neuronal damage observed in CJD.
The pathophysiology of CJD is complex and involves intricate interactions between misfolded prion proteins, neurotoxicity, inflammation, and neuronal degeneration. The progressive accumulation and spread of abnormal PrP^Sc protein disrupt normal cellular function and ultimately lead to the characteristic clinical manifestations and severe neurological impairment seen in CJD.
Creutzfeldt-Jakob Disease (CJD) is caused by the accumulation and misfolding of abnormal prion proteins in the brain. These abnormal prions are the etiological agents responsible for the development of the disease. Here are the key aspects regarding the etiology of CJD:
Abnormal Prions: The primary etiological factor in CJD is the presence of abnormal isoforms of the prion protein (PrP). Prions are misfolded, infectious proteins that can induce the misfolding of normal cellular prion proteins into the abnormal isoform. The abnormal prions are highly stable and resistant to degradation by normal cellular processes.
Sporadic CJD: The majority of CJD cases (about 85%) are sporadic, meaning they occur spontaneously without any apparent cause or predisposing factors. In sporadic CJD, the origin of the abnormal prions is not fully understood. It is believed to involve spontaneous misfolding of normal cellular prion proteins, resulting in the development of the disease.
Genetic Mutations: Some cases of CJD are caused by genetic mutations in the PRNP gene, which encodes the prion protein. These mutations lead to the production of abnormal prion proteins or increased susceptibility to the misfolding process. Familial forms of CJD result from these inherited mutations in an autosomal dominant pattern. However, familial cases account for a smaller proportion of overall CJD cases (about 10-15%).
Acquired CJD: Acquired forms of CJD can occur due to exposure to infected brain or nervous system tissue. The most well-known example of acquired CJD is variant CJD (vCJD), which is associated with consumption of prion-contaminated meat products, particularly beef, from cattle affected by bovine spongiform encephalopathy (BSE or “mad cow” disease). Other forms of acquired CJD, known as iatrogenic CJD, can result from medical procedures involving infected tissues or contaminated surgical instruments.
Transmission: CJD is not considered a contagious disease in the usual sense. It does not spread through casual contact or respiratory droplets. However, transmission can occur through direct exposure to infected tissues or through certain medical procedures. The transmission routes for acquired and iatrogenic CJD are well-documented, while the transmission route for sporadic and familial CJD remains uncertain.
The etiology of CJD is primarily linked to the misfolding and accumulation of abnormal prion proteins in the brain. While the exact mechanisms underlying spontaneous misfolding or genetic mutations leading to abnormal prion formation are not fully understood, extensive research has provided valuable insights into the role of prions in the development of CJD.
The prognosis for individuals with CJD is generally poor, and the disease typically leads to severe disability and death within a relatively short period of time. Here are key aspects of the prognosis in CJD:
Rapid Disease Progression: CJD is characterized by a rapid progression of symptoms over weeks to months. As the disease advances, individuals experience worsening cognitive decline, neurological deficits, and functional impairment. The duration of illness varies, but most individuals succumb to the disease within a year of symptom onset.
Neurological Decline: CJD affects various areas of the brain, leading to a wide range of neurological symptoms. These symptoms include cognitive impairment, memory loss, behavioral changes, motor abnormalities, visual disturbances, and difficulties with coordination and balance. The neurological decline in CJD can result in profound disability, with individuals becoming bedridden and requiring assistance with activities of daily living.
Lack of Effective Treatment: Currently, there is no known cure for CJD, and no specific treatment can halt or reverse the disease progression. While supportive care measures can help manage symptoms and improve comfort, they do not alter the underlying course of the disease.
Variable Disease Duration: The duration of illness can vary among individuals with CJD. Sporadic and genetic forms of CJD often have a more rapid progression compared to acquired forms, such as variant CJD (vCJD). However, the disease course is generally characterized by a relentless decline.
Impact on Quality of Life: CJD significantly affects the quality of life of individuals and their families. The rapid decline in neurological function and the loss of independence and cognitive abilities can be emotionally challenging for both the affected individual and their loved ones.
Fatal Outcome: CJD is ultimately fatal, with most individuals succumbing to the disease within months of symptom onset. Death is typically due to complications associated with severe neurological dysfunction, such as respiratory failure or infections.
Clinical history
The clinical history of Creutzfeldt-Jakob Disease (CJD) typically involves the progressive development of neurological symptoms over a relatively short period of time. The duration of symptoms can vary but is usually measured in months rather than years. Here are some key aspects of the clinical history of CJD:
Rapidly Progressive Cognitive Decline: One of the hallmark features of CJD is the rapid onset and progressive decline in cognitive function. Individuals may experience memory loss, difficulty with attention and concentration, confusion, disorientation, and problems with language and speech. These cognitive changes tend to worsen rapidly over weeks to months.
Neurological Symptoms: CJD can also involve a variety of neurological symptoms, which may vary among individuals. These symptoms can include changes in behavior and personality, mood disturbances, anxiety, depression, and irritability. In addition, individuals may experience difficulties with coordination and balance, muscle stiffness, involuntary movements (such as myoclonus or chorea), and sensory abnormalities.
Visual Disturbances: Visual symptoms are common in CJD and may include blurred vision, visual hallucinations, and visual field deficits. These disturbances can range from subtle changes to significant visual impairment.
Sleep Disturbances: Sleep abnormalities, including disrupted sleep patterns, excessive daytime sleepiness, and rapid eye movement (REM) sleep behavior disorder, can occur in some individuals with CJD.
Neurological Examination Findings: The neurological examination may reveal various abnormalities depending on the stage of the disease. These can include cognitive impairment, changes in behavior and personality, abnormalities in muscle tone and movement, abnormal eye movements, and signs of cerebellar dysfunction.
Absence of Systemic Features: CJD primarily affects the central nervous system and does not typically present with systemic symptoms such as fever or weight loss. The absence of systemic manifestations helps to distinguish CJD from other conditions.
Physical examination
The physical examination of an individual suspected to have Creutzfeldt-Jakob Disease (CJD) focuses on assessing neurological findings and other associated signs. The examination aims to evaluate the presence and severity of neurological deficits and exclude other possible causes for the symptoms. Here are key aspects of the physical examination in CJD:
Neurological Examination:
Extra neurological Findings:
Systemic Examination:
Differential diagnosis
Creutzfeldt-Jakob Disease (CJD) is a rare neurological disorder with symptoms that can overlap with other conditions. Therefore, it is important to consider a range of differential diagnoses when evaluating individuals suspected of having CJD. Here are some key conditions to consider in the differential diagnosis of CJD:
Other Prion Diseases: Other prion diseases can present with similar clinical features to CJD. These include variant Creutzfeldt-Jakob Disease (vCJD), which is associated with bovine spongiform encephalopathy (BSE or “mad cow” disease), and other rare prion diseases such as Gerstmann-Sträussler-Scheinker syndrome (GSS) and fatal familial insomnia (FFI).
Other Neurodegenerative Disorders: Several other neurodegenerative disorders may exhibit clinical features similar to CJD. These include Alzheimer’s disease, frontotemporal dementia, Lewy body dementia, and progressive supranuclear palsy. Distinguishing features and specific diagnostic criteria can aid in differentiating these conditions from CJD.
Autoimmune Encephalitis: Autoimmune encephalitis, such as anti-NMDA receptor encephalitis or Hashimoto’s encephalopathy, can present with rapidly progressive cognitive decline, behavioral changes, and neurological symptoms that can mimic CJD. Clinical history, specific antibody testing, and neuroimaging findings may help differentiate autoimmune encephalitis from CJD.
Metabolic Disorders: Certain metabolic disorders, such as Wilson’s disease, mitochondrial disorders, and other lysosomal storage disorders, may have overlapping neurological features with CJD. Laboratory tests, genetic testing, and imaging studies can assist in differentiating these conditions from CJD.
Paraneoplastic Syndromes: Paraneoplastic syndromes associated with certain cancers, such as paraneoplastic limbic encephalitis, can manifest with cognitive and neurological symptoms resembling CJD. Close evaluation of clinical history, tumor markers, and appropriate imaging and laboratory investigations are important in making the distinction.
Infectious Diseases: In rare cases, infectious diseases that affect the central nervous system, such as viral encephalitis or prion diseases other than CJD, can present with similar symptoms. Detailed clinical history, cerebrospinal fluid analysis, and appropriate diagnostic testing can help differentiate these conditions from CJD.
Psychiatric Disorders: Certain psychiatric disorders, such as psychosis or rapidly progressive dementia associated with severe depression, may share some features with CJD. Psychiatric evaluation, longitudinal assessment, and response to appropriate treatment interventions are essential in distinguishing psychiatric disorders from CJD.
Distinguishing CJD from other conditions can be challenging, and a comprehensive evaluation is necessary. This typically includes a detailed medical history, neurological examination, neuropsychological testing, neuroimaging (such as MRI), electroencephalogram (EEG), cerebrospinal fluid analysis, and occasionally brain biopsy or genetic testing. Consultation with neurologists, neuropsychiatrists, or specialists in prion diseases is recommended for accurate diagnosis and appropriate management.
Currently, there is no known cure or specific treatment that can halt or reverse the progression of Creutzfeldt-Jakob Disease (CJD). The management of CJD primarily focuses on providing supportive care to improve quality of life and alleviate symptoms. Treatment is typically palliative and aims to address the specific needs and complications associated with the disease. Here are some aspects of the treatment approach for CJD:
Symptom Management: Various medications may be used to manage specific symptoms and improve the individual’s comfort. These may include medications to control muscle stiffness (spasticity) or myoclonus (sudden muscle jerks), medications to address mood disturbances or psychiatric symptoms, and sleep aids to manage sleep disturbances.
Nutritional Support: As the disease progresses, individuals with CJD may experience difficulty swallowing (dysphagia) and weight loss. Nutritional support, such as modified diets or feeding tubes, may be necessary to ensure adequate nutrition and hydration.
Pain Management: Pain can be associated with CJD, and appropriate pain management strategies, including medications or non-pharmacological approaches, should be implemented to alleviate discomfort.
Supportive Care: Comprehensive supportive care is crucial for individuals with CJD. This involves addressing their physical, emotional, and psychological needs. Supportive care may include physical therapy to maintain mobility and prevent contractures, occupational therapy to assist with daily activities, and speech therapy to manage speech and swallowing difficulties.
End-of-Life Care: CJD is a progressive and ultimately fatal disease. As the disease advances, individuals may require end-of-life care, including hospice or palliative care services. These services focus on maximizing comfort, providing emotional support to individuals and their families, and ensuring a dignified and peaceful end-of-life experience.
https://www.ncbi.nlm.nih.gov/books/NBK507860/
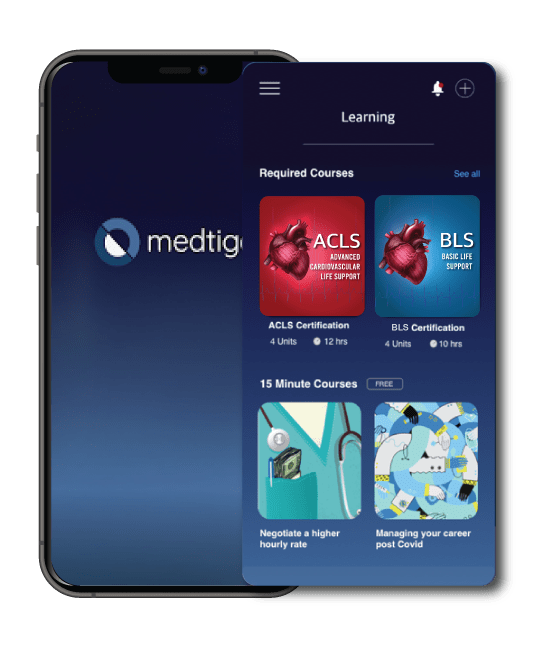
Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.
On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.
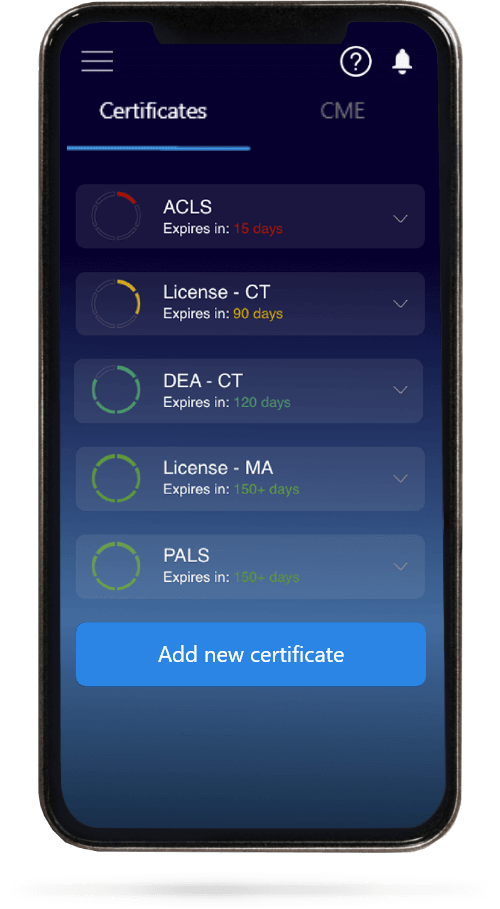
When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.