Ostarine: The ‘Invisible’ Doping Threat Trapping Innocent Athletes
February 18, 2026
Background
Eosinophilic gastroenteritis (EGE) is an uncommon inflammatory bowel disease. It affects both kids and grownups. The hallmark is over twenty eosinophils per high-power field (HPF). These eosinophils infiltrate stomach, duodenum, esophagus, and sometimes colon. Symptoms like weight loss, nausea, throwing up, diarrhea, and belly pain occur. Often, there’s no clear reason for the high eosinophils. EGE typically involves the mucosal lining, muscle layer, or outer serosa of the GI tract. Clinical features depend on where the eosinophils accumulate. Many patients have food allergies or atopic conditions like asthma. Though first described by Kaijser in 1937, later case studies expanded our knowledge. Still, treatments often fail, and the long-term outlook remains uncertain.
Epidemiology
Eosinophilic gastroenteritis is a condition that’s tricky to understand how common it is. This is because it’s often not diagnosed correctly. However, cases have been reported all over the world. It seems to be more frequent in Asian patients. These patients are more likely to have eosinophilic infiltration of the colon compared to White patients. Studies show that the symptoms can vary between different races. For instance, Asian patients with eosinophilic esophagitis tend to experience less difficulty swallowing and heartburn. But they have more vomiting and abdominal pain. Several reports from places like Seoul, Korea, China, and India have described new EGE cases over time. This indicates it occurs globally. The estimated incidence is around 1 case per 100,000 people. And the prevalence is 28 cases per 100,000 in the United States. While EGE is mainly linked to White individuals, some Asians can get it too, with a slight tendency towards affecting more males. It can happen at any age, but usually becomes clinically apparent in the 3rd or 5th decade of life.
Anatomy
Pathophysiology
The cause for eosinophilic gastroenteritis remains unclear. Eosinophils in the small intestine or stomach characterize it. It’s either primary or secondary. Primary types include familial, nonatopic, atopic. Also called idiopathic or allergic. Which layer of the GI tract is affected determines symptoms. Secondary types include hypereosinophilic disorders, vasculitis, IBD, celiac disease. Research shows eosinophils, eotaxin, T helper 2 cytokines play key roles. Eosinophils express MHC class II molecules. They release factors causing inflammation. Some patients have high total IgE levels, suggesting atopy. Others have non-IgE mechanism, with thymic stromal lymphopoietin (TSLP) upregulation.
Etiology
As we look at eosinophilic gastroenteritis, a tricky condition puzzles doctors. What exactly triggers this buildup of eosinophils in the gut? Patients often show high levels of IgE and eosinophils in tissues and blood. One idea is an imbalance in the T-cell system. This leads to too much of certain interleukins like IL-13, IL-4, and IL-5. These interleukins boost IgE production and eosinophil levels. Interestingly, studies found key cytokines (IL-3, GM-CSF, IL-5) inside eosinophil granules. This hints that eosinophil invasion in intestines may release these, worsening inflammation. Grasping these underlying pathways could guide better eosinophilic gastroenteritis treatment.
Genetics
Prognostic Factors
Eosinophilic gastroenteritis (EGE) remains a poorly-researched condition. Few studies exist on how common it is and how it progresses. EGE causes symptoms that come and go. They can be mild or severe. Mild cases may only need monitoring. More severe flare-ups require oral steroids to control. Studies show that finding food triggers can lead to EGE going away in childhood. This is especially true if it starts in infancy. A study by De Chambrun et al. found EGE can follow three patterns over time. Some cases have only a single outbreak lasting less than three months. Others have flare-ups off-and-on. Still others have constant, ongoing symptoms. While EGE can cause serious issues like intestinal blockages or tears, fatal outcomes are very rare. It does not increase cancer risk. Bloody diarrhea mimicking inflammatory bowel disease and intestinal perforations needing surgery are possible complications. In some cases, EGE spreads outside the intestines. This can cause jaundice, gallbladder/pancreas inflammation with bile duct blockage, and liver inflammation from eosinophils.
Clinical History
Eosinophilic gastroenteritis, also known as EGE, is an illness that brings varying symptoms. This depends on how much the intestinal walls are affected. EGE commonly targets the small intestine. To diagnose EGE, doctors check for high eosinophil levels. They also look at tissue samples under a microscope. EGE must be distinguished from other conditions too. Lab results may show increased eosinophils in blood tests. Also, serum albumin levels are often low with EGE. Imaging scans can reveal thickened intestine walls. An endoscopy procedure can confirm EGE diagnosis. During this, biopsies are taken to check for high eosinophil counts. Treatment involves oral corticosteroid medication for flare-ups. However, experts still don’t fully understand EGE’s long-term progression.
Physical Examination
Most people have different Eosinophilic gastroenteritis symptoms. Kids often have conditions like hay fever and asthma. Grownups may have trouble swallowing or belly pain. Growth can be slow for children. Muscle layer problems may block the intestines. More often, the stomach is affected than the small intestine. People feel sick, throw up, and have belly aches. Those with mucosal disease usually have allergy histories. Rarely, the serosal layer is inflamed, causing fluid buildup in the abdomen.
Age group
Associated comorbidity
Associated activity
Acuity of presentation
Differential Diagnoses
Laboratory Studies
Imaging Studies
Procedures
Histologic Findings
Staging
Treatment Paradigm
Doctors use these key methods to handle eosinophilic gastroenteritis. They ask many questions about health history. They examine the body carefully. They check for too many eosinophils (a type of white blood cell) in the gastrointestinal tract. They assess symptoms related to this condition. Ruling out other causes of high eosinophil levels helps diagnose this disorder. Simple treatments often help many patients. One option is removing certain foods from the diet. Another is taking steroid medicines like glucocorticosteroids. Follow-up visits every six months are smart. New treatments targeting a protein called IL-5 look promising. They may lower eosinophil counts well. Omalizumab and clarithromycin show potential benefits too, though effects vary. Surgery should only happen for chronic obstruction cases. Even after surgery, symptoms can return sometimes. So doctors avoid operating unless absolutely needed. Gastroenterologists and allergy experts provide specialized care. They evaluate further and manage treatment, especially for ongoing symptoms and high eosinophil levels overall.
by Stage
by Modality
Chemotherapy
Radiation Therapy
Surgical Interventions
Hormone Therapy
Immunotherapy
Hyperthermia
Photodynamic Therapy
Stem Cell Transplant
Targeted Therapy
Palliative Care
lifestyle-modifications
Lifestyle modifications
Patients with eosinophilic gastroenteritis should get info on seeking medical help when needed. They should avoid foods that make symptoms worse. At first, an elimination diet without milk, eggs, wheat, gluten, soy, and beef may help. Food hypersensitivity tests like RAST or skin tests may be considered if reactions seem likely. Restrictive or elemental diets have shown promise for managing symptoms. Still, strong clinical data is lacking. Based on available studies, trying to eliminate six common allergenic foods – milk, soy, wheat, eggs, peanuts/tree nuts, and fish/shellfish – may be attempted. The American Partnership for Eosinophilic Disorders (APFED) provides support and educational resources. Monitoring eosinophil counts after dietary changes can assess therapeutic response. But pinpointing specific trigger foods remains hard.
Use of corticosteroids
Eosinophilic gastroenteritis causes obstructive symptoms. Treating this requires medication. Corticosteroids work best, improving symptoms in most patients Prednisone treats effectively. Other corticosteroids prescribed include fluticasone, prednisolone, budesonide.
Fluticasone inhaled
Fluticasone helps asthma by reducing inflammation, eosinophil recruitment when inhaled.
Budesonide oral suspension
Budesonide oral suspension and prednisolone reduce inflammation, capillary permeability too.
Prednisolone
Budesonide oral suspension and prednisolone reduce inflammation, capillary permeability too.
Use of glucocorticosteroids (Mast cell stabilizers)
Many patients with eosinophilic gastroenteritis affecting the mucosal layer find relief from anti-inflammatory drugs and diet therapy. Oral glucocorticoids and oral cromolyn work by stopping mast cell degranulation caused by allergen exposure. They help people with food intolerance or allergy.
Cromolyn
Cromolyn specifically prevents mast cells from releasing histamine and other inflammatory substances. It also reduces neutrophil inflow and the production of damaging oxygen radicals by NADPH oxidase. Diet elimination therapy, when combined with these medications, can offer relief.
Use of antihistamines (leukotriene receptor antagonists)
Eosinophilic gastroenteritis has treatment options. Antihistamines and mast cell stabilizers help by stopping histamine’s inflammation effects. Also suggested are alternative Chinese medicines and drugs like mycophenolate mofetil and montelukast, though effectiveness is low.
Montelukast
Montelukast is selective agonist of leukotriene D4 at cysteinyl leukotriene receptor (CysLT1), but limited action.
Use of Macrolides
Clarithromycin
Bacteria need ribosomes to make proteins and grow. The antibiotic clarithromycin binds to one part of bacterial ribosomes. It stops the ribosomes from working right. This keeps new proteins from being made. Without new proteins, the bacteria can’t grow.
Monitoring for long-term
Eosinophilic gastroenteritis (EGE) has diverse symptoms, so there aren’t strict rules for long-term check-ups. Some patients have flare-ups now and then, while others experience just one episode or ongoing illness. Yearly visits might be wise. The American Partnership For Eosinophilic Disorders (APFED) created an online patient registry to gather data on how the disease progresses. With EGE, endoscopy and imaging tests can seem normal, yet still prove useful for follow-up exams when needed.
phases-of-management
Phase of diagnosis:
Handling Acute Symptoms:
Maintenance Therapy:
Nutritional Assistance:
Cooperation with Experts:
Patient Instruction:
Frequent Monitoring
Medication
Future Trends
Eosinophilic gastroenteritis (EGE) is an uncommon inflammatory bowel disease. It affects both kids and grownups. The hallmark is over twenty eosinophils per high-power field (HPF). These eosinophils infiltrate stomach, duodenum, esophagus, and sometimes colon. Symptoms like weight loss, nausea, throwing up, diarrhea, and belly pain occur. Often, there’s no clear reason for the high eosinophils. EGE typically involves the mucosal lining, muscle layer, or outer serosa of the GI tract. Clinical features depend on where the eosinophils accumulate. Many patients have food allergies or atopic conditions like asthma. Though first described by Kaijser in 1937, later case studies expanded our knowledge. Still, treatments often fail, and the long-term outlook remains uncertain.
Eosinophilic gastroenteritis is a condition that’s tricky to understand how common it is. This is because it’s often not diagnosed correctly. However, cases have been reported all over the world. It seems to be more frequent in Asian patients. These patients are more likely to have eosinophilic infiltration of the colon compared to White patients. Studies show that the symptoms can vary between different races. For instance, Asian patients with eosinophilic esophagitis tend to experience less difficulty swallowing and heartburn. But they have more vomiting and abdominal pain. Several reports from places like Seoul, Korea, China, and India have described new EGE cases over time. This indicates it occurs globally. The estimated incidence is around 1 case per 100,000 people. And the prevalence is 28 cases per 100,000 in the United States. While EGE is mainly linked to White individuals, some Asians can get it too, with a slight tendency towards affecting more males. It can happen at any age, but usually becomes clinically apparent in the 3rd or 5th decade of life.
The cause for eosinophilic gastroenteritis remains unclear. Eosinophils in the small intestine or stomach characterize it. It’s either primary or secondary. Primary types include familial, nonatopic, atopic. Also called idiopathic or allergic. Which layer of the GI tract is affected determines symptoms. Secondary types include hypereosinophilic disorders, vasculitis, IBD, celiac disease. Research shows eosinophils, eotaxin, T helper 2 cytokines play key roles. Eosinophils express MHC class II molecules. They release factors causing inflammation. Some patients have high total IgE levels, suggesting atopy. Others have non-IgE mechanism, with thymic stromal lymphopoietin (TSLP) upregulation.
As we look at eosinophilic gastroenteritis, a tricky condition puzzles doctors. What exactly triggers this buildup of eosinophils in the gut? Patients often show high levels of IgE and eosinophils in tissues and blood. One idea is an imbalance in the T-cell system. This leads to too much of certain interleukins like IL-13, IL-4, and IL-5. These interleukins boost IgE production and eosinophil levels. Interestingly, studies found key cytokines (IL-3, GM-CSF, IL-5) inside eosinophil granules. This hints that eosinophil invasion in intestines may release these, worsening inflammation. Grasping these underlying pathways could guide better eosinophilic gastroenteritis treatment.
Eosinophilic gastroenteritis (EGE) remains a poorly-researched condition. Few studies exist on how common it is and how it progresses. EGE causes symptoms that come and go. They can be mild or severe. Mild cases may only need monitoring. More severe flare-ups require oral steroids to control. Studies show that finding food triggers can lead to EGE going away in childhood. This is especially true if it starts in infancy. A study by De Chambrun et al. found EGE can follow three patterns over time. Some cases have only a single outbreak lasting less than three months. Others have flare-ups off-and-on. Still others have constant, ongoing symptoms. While EGE can cause serious issues like intestinal blockages or tears, fatal outcomes are very rare. It does not increase cancer risk. Bloody diarrhea mimicking inflammatory bowel disease and intestinal perforations needing surgery are possible complications. In some cases, EGE spreads outside the intestines. This can cause jaundice, gallbladder/pancreas inflammation with bile duct blockage, and liver inflammation from eosinophils.
Eosinophilic gastroenteritis, also known as EGE, is an illness that brings varying symptoms. This depends on how much the intestinal walls are affected. EGE commonly targets the small intestine. To diagnose EGE, doctors check for high eosinophil levels. They also look at tissue samples under a microscope. EGE must be distinguished from other conditions too. Lab results may show increased eosinophils in blood tests. Also, serum albumin levels are often low with EGE. Imaging scans can reveal thickened intestine walls. An endoscopy procedure can confirm EGE diagnosis. During this, biopsies are taken to check for high eosinophil counts. Treatment involves oral corticosteroid medication for flare-ups. However, experts still don’t fully understand EGE’s long-term progression.
Most people have different Eosinophilic gastroenteritis symptoms. Kids often have conditions like hay fever and asthma. Grownups may have trouble swallowing or belly pain. Growth can be slow for children. Muscle layer problems may block the intestines. More often, the stomach is affected than the small intestine. People feel sick, throw up, and have belly aches. Those with mucosal disease usually have allergy histories. Rarely, the serosal layer is inflamed, causing fluid buildup in the abdomen.
Doctors use these key methods to handle eosinophilic gastroenteritis. They ask many questions about health history. They examine the body carefully. They check for too many eosinophils (a type of white blood cell) in the gastrointestinal tract. They assess symptoms related to this condition. Ruling out other causes of high eosinophil levels helps diagnose this disorder. Simple treatments often help many patients. One option is removing certain foods from the diet. Another is taking steroid medicines like glucocorticosteroids. Follow-up visits every six months are smart. New treatments targeting a protein called IL-5 look promising. They may lower eosinophil counts well. Omalizumab and clarithromycin show potential benefits too, though effects vary. Surgery should only happen for chronic obstruction cases. Even after surgery, symptoms can return sometimes. So doctors avoid operating unless absolutely needed. Gastroenterologists and allergy experts provide specialized care. They evaluate further and manage treatment, especially for ongoing symptoms and high eosinophil levels overall.
Gastroenterology
Lifestyle modifications
Patients with eosinophilic gastroenteritis should get info on seeking medical help when needed. They should avoid foods that make symptoms worse. At first, an elimination diet without milk, eggs, wheat, gluten, soy, and beef may help. Food hypersensitivity tests like RAST or skin tests may be considered if reactions seem likely. Restrictive or elemental diets have shown promise for managing symptoms. Still, strong clinical data is lacking. Based on available studies, trying to eliminate six common allergenic foods – milk, soy, wheat, eggs, peanuts/tree nuts, and fish/shellfish – may be attempted. The American Partnership for Eosinophilic Disorders (APFED) provides support and educational resources. Monitoring eosinophil counts after dietary changes can assess therapeutic response. But pinpointing specific trigger foods remains hard.
Use of corticosteroids
Eosinophilic gastroenteritis causes obstructive symptoms. Treating this requires medication. Corticosteroids work best, improving symptoms in most patients Prednisone treats effectively. Other corticosteroids prescribed include fluticasone, prednisolone, budesonide.
Fluticasone inhaled
Fluticasone helps asthma by reducing inflammation, eosinophil recruitment when inhaled.
Budesonide oral suspension
Budesonide oral suspension and prednisolone reduce inflammation, capillary permeability too.
Prednisolone
Budesonide oral suspension and prednisolone reduce inflammation, capillary permeability too.
Gastroenterology
Many patients with eosinophilic gastroenteritis affecting the mucosal layer find relief from anti-inflammatory drugs and diet therapy. Oral glucocorticoids and oral cromolyn work by stopping mast cell degranulation caused by allergen exposure. They help people with food intolerance or allergy.
Cromolyn
Cromolyn specifically prevents mast cells from releasing histamine and other inflammatory substances. It also reduces neutrophil inflow and the production of damaging oxygen radicals by NADPH oxidase. Diet elimination therapy, when combined with these medications, can offer relief.
Gastroenterology
Eosinophilic gastroenteritis has treatment options. Antihistamines and mast cell stabilizers help by stopping histamine’s inflammation effects. Also suggested are alternative Chinese medicines and drugs like mycophenolate mofetil and montelukast, though effectiveness is low.
Montelukast
Montelukast is selective agonist of leukotriene D4 at cysteinyl leukotriene receptor (CysLT1), but limited action.
Gastroenterology
Clarithromycin
Bacteria need ribosomes to make proteins and grow. The antibiotic clarithromycin binds to one part of bacterial ribosomes. It stops the ribosomes from working right. This keeps new proteins from being made. Without new proteins, the bacteria can’t grow.
Monitoring for long-term
Eosinophilic gastroenteritis (EGE) has diverse symptoms, so there aren’t strict rules for long-term check-ups. Some patients have flare-ups now and then, while others experience just one episode or ongoing illness. Yearly visits might be wise. The American Partnership For Eosinophilic Disorders (APFED) created an online patient registry to gather data on how the disease progresses. With EGE, endoscopy and imaging tests can seem normal, yet still prove useful for follow-up exams when needed.
Gastroenterology
Phase of diagnosis:
Handling Acute Symptoms:
Maintenance Therapy:
Nutritional Assistance:
Cooperation with Experts:
Patient Instruction:
Frequent Monitoring
Eosinophilic gastroenteritis (EGE) is an uncommon inflammatory bowel disease. It affects both kids and grownups. The hallmark is over twenty eosinophils per high-power field (HPF). These eosinophils infiltrate stomach, duodenum, esophagus, and sometimes colon. Symptoms like weight loss, nausea, throwing up, diarrhea, and belly pain occur. Often, there’s no clear reason for the high eosinophils. EGE typically involves the mucosal lining, muscle layer, or outer serosa of the GI tract. Clinical features depend on where the eosinophils accumulate. Many patients have food allergies or atopic conditions like asthma. Though first described by Kaijser in 1937, later case studies expanded our knowledge. Still, treatments often fail, and the long-term outlook remains uncertain.
Eosinophilic gastroenteritis is a condition that’s tricky to understand how common it is. This is because it’s often not diagnosed correctly. However, cases have been reported all over the world. It seems to be more frequent in Asian patients. These patients are more likely to have eosinophilic infiltration of the colon compared to White patients. Studies show that the symptoms can vary between different races. For instance, Asian patients with eosinophilic esophagitis tend to experience less difficulty swallowing and heartburn. But they have more vomiting and abdominal pain. Several reports from places like Seoul, Korea, China, and India have described new EGE cases over time. This indicates it occurs globally. The estimated incidence is around 1 case per 100,000 people. And the prevalence is 28 cases per 100,000 in the United States. While EGE is mainly linked to White individuals, some Asians can get it too, with a slight tendency towards affecting more males. It can happen at any age, but usually becomes clinically apparent in the 3rd or 5th decade of life.
The cause for eosinophilic gastroenteritis remains unclear. Eosinophils in the small intestine or stomach characterize it. It’s either primary or secondary. Primary types include familial, nonatopic, atopic. Also called idiopathic or allergic. Which layer of the GI tract is affected determines symptoms. Secondary types include hypereosinophilic disorders, vasculitis, IBD, celiac disease. Research shows eosinophils, eotaxin, T helper 2 cytokines play key roles. Eosinophils express MHC class II molecules. They release factors causing inflammation. Some patients have high total IgE levels, suggesting atopy. Others have non-IgE mechanism, with thymic stromal lymphopoietin (TSLP) upregulation.
As we look at eosinophilic gastroenteritis, a tricky condition puzzles doctors. What exactly triggers this buildup of eosinophils in the gut? Patients often show high levels of IgE and eosinophils in tissues and blood. One idea is an imbalance in the T-cell system. This leads to too much of certain interleukins like IL-13, IL-4, and IL-5. These interleukins boost IgE production and eosinophil levels. Interestingly, studies found key cytokines (IL-3, GM-CSF, IL-5) inside eosinophil granules. This hints that eosinophil invasion in intestines may release these, worsening inflammation. Grasping these underlying pathways could guide better eosinophilic gastroenteritis treatment.
Eosinophilic gastroenteritis (EGE) remains a poorly-researched condition. Few studies exist on how common it is and how it progresses. EGE causes symptoms that come and go. They can be mild or severe. Mild cases may only need monitoring. More severe flare-ups require oral steroids to control. Studies show that finding food triggers can lead to EGE going away in childhood. This is especially true if it starts in infancy. A study by De Chambrun et al. found EGE can follow three patterns over time. Some cases have only a single outbreak lasting less than three months. Others have flare-ups off-and-on. Still others have constant, ongoing symptoms. While EGE can cause serious issues like intestinal blockages or tears, fatal outcomes are very rare. It does not increase cancer risk. Bloody diarrhea mimicking inflammatory bowel disease and intestinal perforations needing surgery are possible complications. In some cases, EGE spreads outside the intestines. This can cause jaundice, gallbladder/pancreas inflammation with bile duct blockage, and liver inflammation from eosinophils.
Eosinophilic gastroenteritis, also known as EGE, is an illness that brings varying symptoms. This depends on how much the intestinal walls are affected. EGE commonly targets the small intestine. To diagnose EGE, doctors check for high eosinophil levels. They also look at tissue samples under a microscope. EGE must be distinguished from other conditions too. Lab results may show increased eosinophils in blood tests. Also, serum albumin levels are often low with EGE. Imaging scans can reveal thickened intestine walls. An endoscopy procedure can confirm EGE diagnosis. During this, biopsies are taken to check for high eosinophil counts. Treatment involves oral corticosteroid medication for flare-ups. However, experts still don’t fully understand EGE’s long-term progression.
Most people have different Eosinophilic gastroenteritis symptoms. Kids often have conditions like hay fever and asthma. Grownups may have trouble swallowing or belly pain. Growth can be slow for children. Muscle layer problems may block the intestines. More often, the stomach is affected than the small intestine. People feel sick, throw up, and have belly aches. Those with mucosal disease usually have allergy histories. Rarely, the serosal layer is inflamed, causing fluid buildup in the abdomen.
Doctors use these key methods to handle eosinophilic gastroenteritis. They ask many questions about health history. They examine the body carefully. They check for too many eosinophils (a type of white blood cell) in the gastrointestinal tract. They assess symptoms related to this condition. Ruling out other causes of high eosinophil levels helps diagnose this disorder. Simple treatments often help many patients. One option is removing certain foods from the diet. Another is taking steroid medicines like glucocorticosteroids. Follow-up visits every six months are smart. New treatments targeting a protein called IL-5 look promising. They may lower eosinophil counts well. Omalizumab and clarithromycin show potential benefits too, though effects vary. Surgery should only happen for chronic obstruction cases. Even after surgery, symptoms can return sometimes. So doctors avoid operating unless absolutely needed. Gastroenterologists and allergy experts provide specialized care. They evaluate further and manage treatment, especially for ongoing symptoms and high eosinophil levels overall.
Gastroenterology
Lifestyle modifications
Patients with eosinophilic gastroenteritis should get info on seeking medical help when needed. They should avoid foods that make symptoms worse. At first, an elimination diet without milk, eggs, wheat, gluten, soy, and beef may help. Food hypersensitivity tests like RAST or skin tests may be considered if reactions seem likely. Restrictive or elemental diets have shown promise for managing symptoms. Still, strong clinical data is lacking. Based on available studies, trying to eliminate six common allergenic foods – milk, soy, wheat, eggs, peanuts/tree nuts, and fish/shellfish – may be attempted. The American Partnership for Eosinophilic Disorders (APFED) provides support and educational resources. Monitoring eosinophil counts after dietary changes can assess therapeutic response. But pinpointing specific trigger foods remains hard.
Use of corticosteroids
Eosinophilic gastroenteritis causes obstructive symptoms. Treating this requires medication. Corticosteroids work best, improving symptoms in most patients Prednisone treats effectively. Other corticosteroids prescribed include fluticasone, prednisolone, budesonide.
Fluticasone inhaled
Fluticasone helps asthma by reducing inflammation, eosinophil recruitment when inhaled.
Budesonide oral suspension
Budesonide oral suspension and prednisolone reduce inflammation, capillary permeability too.
Prednisolone
Budesonide oral suspension and prednisolone reduce inflammation, capillary permeability too.
Gastroenterology
Many patients with eosinophilic gastroenteritis affecting the mucosal layer find relief from anti-inflammatory drugs and diet therapy. Oral glucocorticoids and oral cromolyn work by stopping mast cell degranulation caused by allergen exposure. They help people with food intolerance or allergy.
Cromolyn
Cromolyn specifically prevents mast cells from releasing histamine and other inflammatory substances. It also reduces neutrophil inflow and the production of damaging oxygen radicals by NADPH oxidase. Diet elimination therapy, when combined with these medications, can offer relief.
Gastroenterology
Eosinophilic gastroenteritis has treatment options. Antihistamines and mast cell stabilizers help by stopping histamine’s inflammation effects. Also suggested are alternative Chinese medicines and drugs like mycophenolate mofetil and montelukast, though effectiveness is low.
Montelukast
Montelukast is selective agonist of leukotriene D4 at cysteinyl leukotriene receptor (CysLT1), but limited action.
Gastroenterology
Clarithromycin
Bacteria need ribosomes to make proteins and grow. The antibiotic clarithromycin binds to one part of bacterial ribosomes. It stops the ribosomes from working right. This keeps new proteins from being made. Without new proteins, the bacteria can’t grow.
Monitoring for long-term
Eosinophilic gastroenteritis (EGE) has diverse symptoms, so there aren’t strict rules for long-term check-ups. Some patients have flare-ups now and then, while others experience just one episode or ongoing illness. Yearly visits might be wise. The American Partnership For Eosinophilic Disorders (APFED) created an online patient registry to gather data on how the disease progresses. With EGE, endoscopy and imaging tests can seem normal, yet still prove useful for follow-up exams when needed.
Gastroenterology
Phase of diagnosis:
Handling Acute Symptoms:
Maintenance Therapy:
Nutritional Assistance:
Cooperation with Experts:
Patient Instruction:
Frequent Monitoring
Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.
On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.
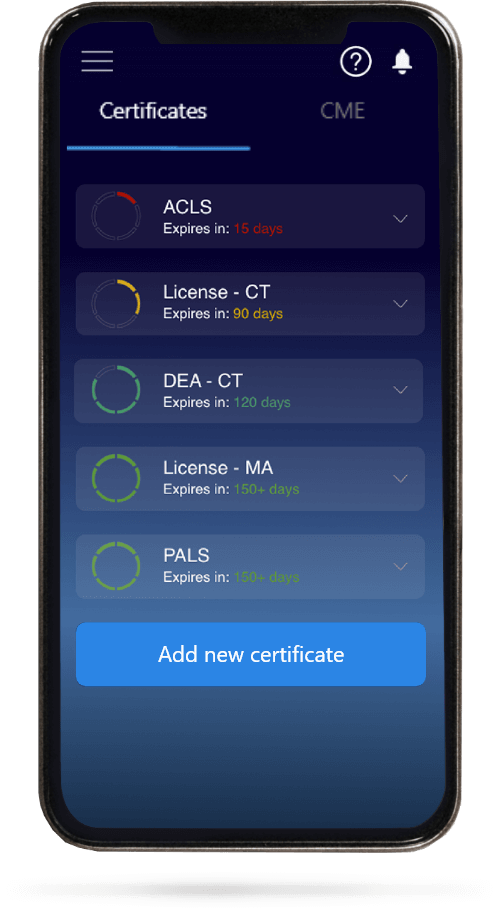
When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.