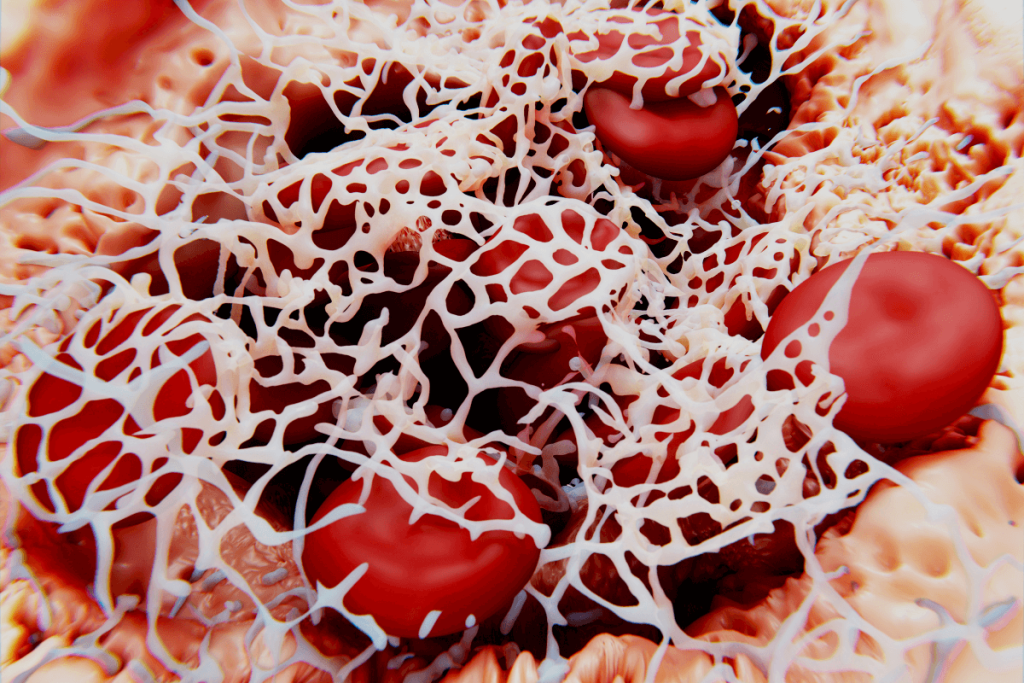
Heparin-induced thrombocytopenia (HIT) is a prothrombotic adverse drug reaction caused by the development of anti-platelet factor 4 4-heparin (PF4/H) antibodies, which trigger platelet activation, immune-mediated elimination, and thrombosis. The characteristic manifestation of HIT is thrombocytopenia accompanied by new-onset thrombosis. HIT presents a complex diagnostic issue, as there is no single test that has both high positive and negative predictive value; thus, accurate diagnosis requires a combination of immunoassays and functional assays.
The enzyme-linked immunosorbent assay (ELISA) is commonly used for initial testing, with sensitivity >95% but modest specificity (50-89%). Its advantages include rapid turnaround, low cost, and very high negative predictive value (0.998; 95% CI, 0.970–1.000), making it a practical first-line option. Due to its limited specificity, confirmation through functional testing is recommended. The serotonin release assay (SRA) remains the gold standard laboratory test, with specificity and sensitivity exceeding 95%, but it is expensive, less accessible, and slower to perform. Although rare, false-negative SRAs have been documented.
If untreated, HIT results in thrombosis in 30–50% of patients, with a venous-to-arterial ratio of 3–4:1. Complications include limb ischemia, organ ischemia, or skin necrosis. Therefore, timely diagnosis and therapeutic anticoagulation are essential.
Researchers present the case of a 47-year-old man with chronic systolic heart failure (EF <20%), pulmonary hypertension, pulmonary embolism, and atrial fibrillation who was evaluated for advanced heart failure therapy. In 2021, after developing a left ventricular (LV) thrombus, he was treated with intravenous heparin. Shortly thereafter, his platelet count dropped from 160 to 92 ×10⁹/L, raising suspicion of associated HIT. A heparin-induced platelet activation (HIPA) test was strongly positive (OD 2.533), but the confirmatory SRA was negative. Heparin was discontinued, and he was transitioned to fondaparinux, then bridged to warfarin.
One month later, he developed recurrent pulmonary embolism. Repeat testing again showed a positive HIPA (OD 1.535), but negative SRAs. Hematology recommended switching to rivaroxaban. Over the next three years, he experienced multiple admissions before ultimately being approved for left ventricular assist device (LVAD) implantation. On admission, he was started on fondaparinux, and later transitioned to enoxaparin in view of repeatedly negative SRAs. The patient underwent LVAD surgery with intraoperative heparin exposure.
Postoperatively, his platelet count decreased from 60 to 128 ×10⁹/L on day 0, reached a nadir of 77 on day 2, and returned to 141 by day 4. Subcutaneous heparin prophylaxis was initiated on day 5, but his platelet count again dropped from 121 to 53 by day 9. He also developed a new upper extremity deep vein thrombosis. Given a 4T score of 7 (~64% HIT probability), heparin was discontinued. Heparin was stopped, and warfarin was initiated. With therapeutic INR achieved by day 10, he was discharged on warfarin therapy.
This case report illustrates SRA-negative HIT, a rare but clinically significant phenomenon. Literature has reported an incidence ranging from 10% to 50%, but in one cohort of 430 patients, 27 cases had SRA-negative HIT, with a higher 30-day mortality compared to SRA-positive HIT cases ( 29.6% vs 8.6%, p=0.045).
Although ELISA remains a practical first-line tool, its limited specificity contributes to diagnostic uncertainty. Functional tests such as SRA identify the serotonin released from platelet granules, but have their own limitations. Modified assays, such as PF4-SRA, may enhance the detection of antibodies by supplementing PF4. Depending on how the data are interpreted, these assays may offer increased sensitivity, although the data are still limited.
This case highlights the diagnostic challenges of HIT in complicated cardiac patients, especially in the perioperative period. It adds to the emerging evidence of the rare SRA-negative HIT. It highlights the critical need for better diagnostic tools and further studies to determine the true incidence, particularly in cardiac surgery populations.
References: Adkins A, Harlan S, Ruckel C. A Rare Presentation of SRA-Negative Heparin Induced Thrombocytopenia in LVAD Patient. medtigo J Pharmacol. 2025;2(3):e30612311. doi:10.63096/medtigo30612311











