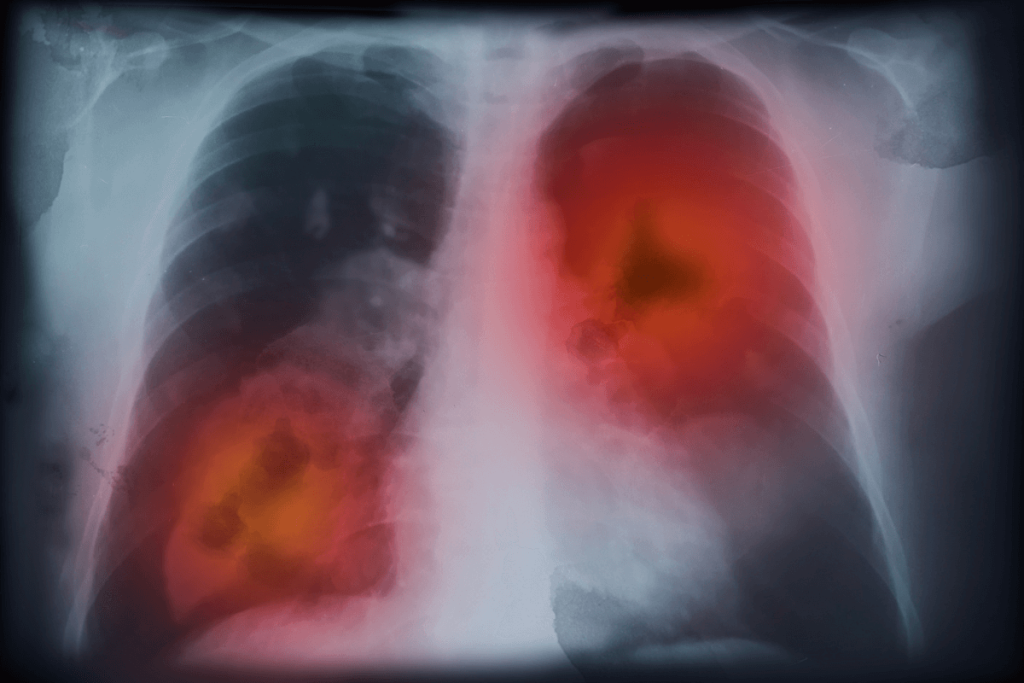
The unusual chemosensory epithelial lineages known as neuroendocrine (NE) cells were identified by the expression of the transcription factors such as POU Class 2 Homeobox 3 (POU2F3) and Achaete-Scute Family BHLH Transcription Factor 1 (ASCL1). Tuft-like fractions are commonly observed in NE tumors, and their properties are related to poor patient outcomes. Using multiple genetically modified animal models, researchers observed that neuroendocrine-tuft-like tumors, which closely resemble human small cell lung cancer (SCLC), arise from the basal cells as the cell of origin.
A lack of representative models has contributed to an incomplete understanding of tuft-like malignancies. Tuft-lineage transcription is associated with the poorest prognosis and originates from brush cells. At least one additional SCLC subtype marker was co-expressed in 80% of the 70 POU2F3-positive samples studied.
Researchers used single-cell RNA sequencing (scRNA seq) to analyse keratin 5 (KRT5) and calcitonin gene-related peptide (CGRP)-initiated RPM tumors to evaluate transcriptional heterogeneity at the single-cell level. Transformed organoids show increased expression of genes linked to LoxP-Stop-LoxP (LSL) recombination and proliferation markers determined by scRNA-seq. In cancer development, ASCL1 and POU2F3 usually do not coexist, and ASCL1 is necessary for NE phenotypes in different types of malignancies.
The in-vivo SCLC model with strong POU2F3 populations is established by blocking NE fate by ASCL1 deletion, which allows YAP1+ and subtype-low tumors to form. Organoids were grown for clonal proliferation before transplantation after being infected with three CellTags. Clones of pattern 1 alternated between basal and Ascl1+ NE states, while pattern six clones were less common and represented a neuronally biased NE population with low adhesion marker expression.
ASCL1 / NEUROD1 / POU2F3 (A/N/P) mixed tumors contained small fractions of basal markers, while Lin-tumors showed strong enrichment for basal cell signature. A significant portion of the YAP1+ human SCLC subtype preferred for basal-like tumor cells, as observed in both YAP1 and mixed tumors. A strong correlation was found between subtype-specific signals from the Caris dataset and their corresponding murine outcomes.
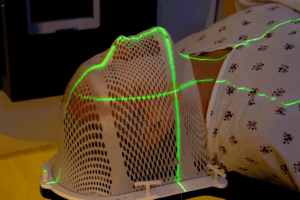
Mice were maintained at a temperature of 18 to 24 °C with a humidity of 40 to 60% under a 12-hour light-dark cycle. The results explain that no significant differences in the tumor phenotype or latency were observed between Rb1/Trp53/Pten (RPP) animals administered tumor-inducing agents intratracheally versus intranasally. Individual lung lobes and trachea were obtained for fixation after the lungs were excised and inflated with 1×phosphate-buffered saline (PBS) in autochthonous mice models. Tissues from the lung and tumor were preserved in 10% neutral buffered formalin solution for at least one day.
Transcriptomics analysis of 944 human SCLCs revealed a tuft-ionocyte-like condition that demonstrates conserved features across cancer states and basal cell injury mechanisms. The human SCLC subtype in basal-derived mice models highlighted the role of basal cells and their ability to differentiate in the formation of SCLC. These findings highlighted that SCLC and other neuroendocrine-tuft malignancies originated from the basal cell and provided a new approach towards lineage plasticity.
Reference: Ireland AS, Xie DA, Hawgood SB, et al. Basal cell of origin resolves neuroendocrine-tuft lineage plasticity in cancer. Nature. 2025. doi:10.1038/s41586-025-09503-z