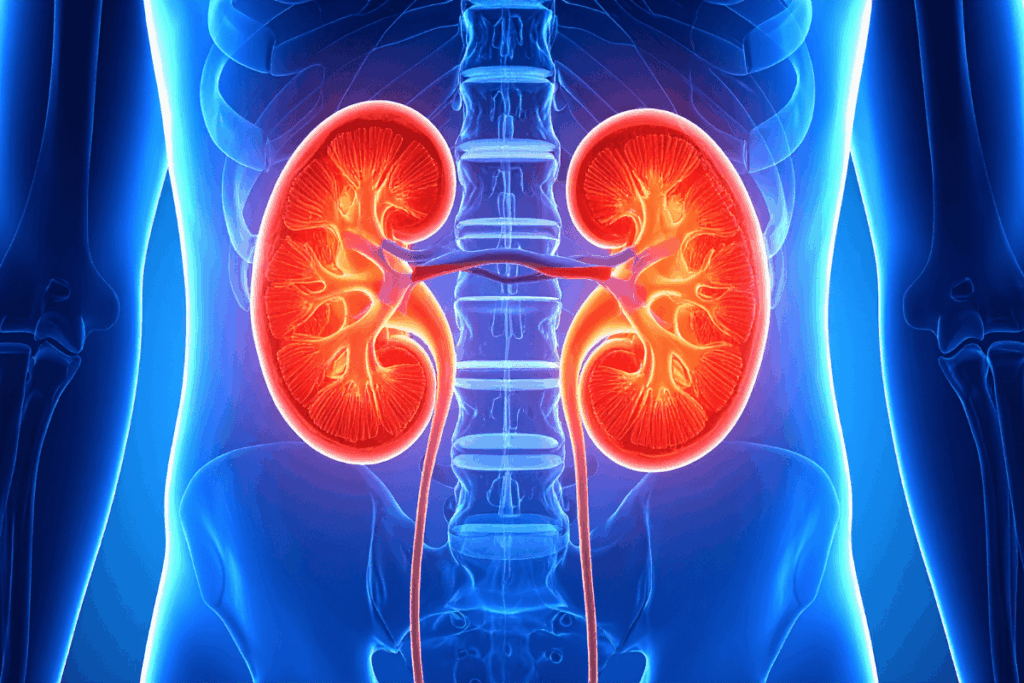
Kidneys play a major role in maintaining overall body health by filtering toxins, waste products, and excess fluids from the blood. Each day, they filter around 150 quarts of blood, supporting the proper functioning of every organ and cell. When the kidneys do not work efficiently, the effects can spread throughout the body.
One of the most common kidney disorders in adults is chronic kidney disease (CKD). CKD is a condition in which the kidneys gradually lose their ability to filter blood effectively. In the U.S., more than one in seven adults is affected by CKD. However, many individuals remain unaware of their condition. This is because CKD often causes no noticeable symptoms until it reaches an advanced stage, close to kidney failure. Although CKD cannot be cured, early diagnosis and appropriate treatment can slow or even halt its progression.
Early detection of this disease is essential, especially for individuals at higher risk. Urine and blood tests are commonly used for assessing kidney function. A standard blood test measures creatinine levels, although results may vary based on physical activity, sex, and age. Newer testing using cystatin C, either alone or in combination with creatinine, provides a more accurate assessment and improves early identification of CKD.
The leading causes of CKD include cardiovascular disease (CVD), diabetes, and high blood pressure, all of which can damage the kidneys over time. Other risk factors include cancer, long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), infections, family history of kidney disease, obesity, and genetic predisposition. As the disease progresses, symptoms may include nausea, muscle cramps, loss of appetite, swelling of the legs/hands/face, shortness of breath, fatigue, chest pain, and difficulty concentrating. Advanced CKD also enhances the risk of brain damage and CVD.
While a CKD diagnosis can be overwhelming, many treatments and lifestyle changes can help manage this condition. Modification of the dietary schedule is a key component of CKD care. Patients are often advised to reduce their intake of phosphorus, sodium, and potassium to prevent complications. Some patients may benefit from limiting the consumption of protein. A heart-healthy diet is generally recommended as it minimizes ultra-processed foods. But dietary plans should be personalized based on disease stage and individual health needs. CKD is actively managed through medical nutrition therapy (MNT).
In addition to dietary changes, lifestyle modifications such as avoiding alcohol and tobacco, managing stress, engaging in regular physical activity, and getting adequate sleep can support kidney and overall health. Medications also play a crucial role in the management of CKD by treating underlying conditions such as high blood pressure and diabetes. Newer therapies can directly slow the progression, and ongoing research aims to tailor treatment to individual patients for optimal outcomes.
In advanced stages, CKD may progress to kidney failure, requiring a kidney transplant or dialysis. Importantly, early medical care and healthy lifestyle choices remain central to CKD management. Individuals at risk should consult with their healthcare providers about appropriate prevention and screening strategies.
Reference: Bock E, Contie V, Jones Y, Lehmann C, Reynolds S. Curbing Chronic Kidney Disease. NIH News in Health. January 2026. Curbing Chronic Kidney Disease | NIH News in Health












