Head and neck cancer (HNC) is one of the most common cancers globally and is frequently treated with radiotherapy (RT), which improves tumor control and survival. Though advances like intensity-modulated radiotherapy (IMRT), which better spares normal tissues, RT is linked with long-term adverse effects that can significantly impair quality of life. Olfactory dysfunction is an underrecognized but clinically significant complication that affects nutrition, weight maintenance, and psychological well-being. The olfactory system is anatomically vulnerable to radiation because the olfactory receptors, epithelium, and olfactory bulb are located in the superior nasal cavity and anterior cranial fossa regions commonly exposed during RT for HNC. Previous research studies have suggested an association between RT and olfactory impairment. However, a clear radiation dose threshold linked to olfactory dysfunction is not well defined, limiting optimization of RT planning for olfactory preservation.
The aim of this prospective, nonrandomized clinical trial was to assess the dose-dependent relationship between radiation exposure to the olfactory region and subsequent olfactory dysfunction in patients with HNC treated with IMRT. The study also sought to detect a critical radiation dose threshold linked with increased risk of olfactory impairment and to characterize changes in the olfactory function over time after RT.
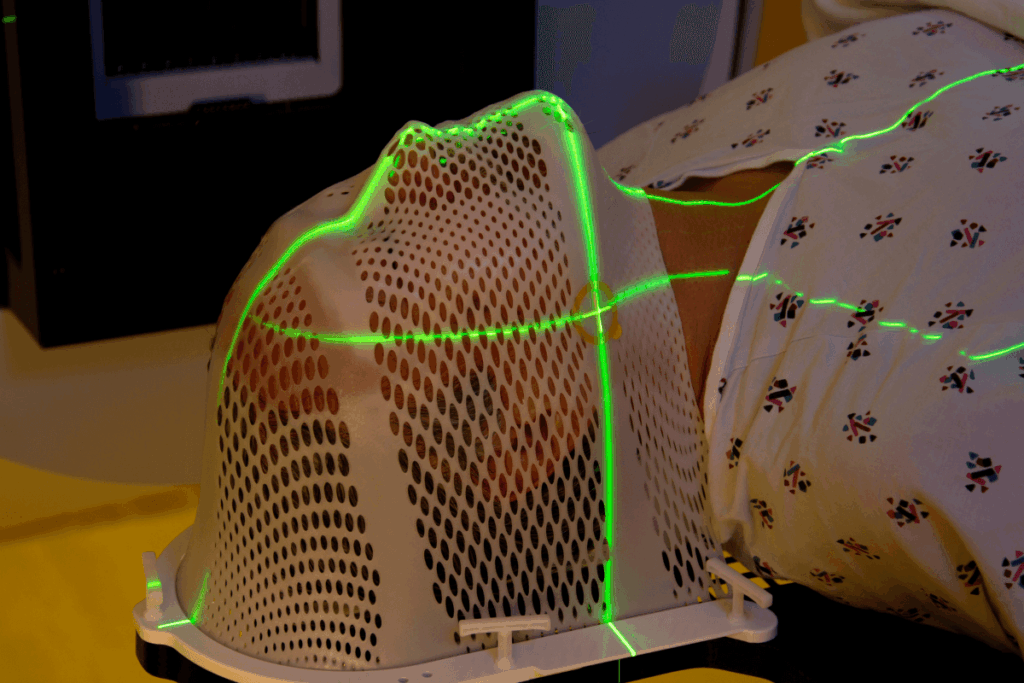
From January 2021 to December 223, patients with histologically confirmed HNC undergoing curative IMRT at a tertiary medical center were prospectively enrolled. Ethical approval and written informed consent were obtained. To ensure an accurate assessment of radiation-related olfactory changes, only patients with normal baseline olfaction, defined as a Taiwan smell identification test (TWSIT) score of ≥40, were included. Patients with prior head and neck RT, significant nasal or sinus disease, head trauma, or baseline olfactory dysfunction were excluded.
Olfactory function was assessed using the validated TWSIT at six time points: before RT, at the end of RT, and at 1, 3, 6, and 12 months after RT. Nasal endoscopy was performed before each assessment to exclude confounding nasal conditions. The olfactory fossae were precisely contoured during IMRT planning, and the mean and maximum radiation doses to the olfactory region were calculated. Statistical analyses included linear regression to assess dose-response relationships, receiver operating characteristic (ROC) curve analysis to detect optimal dose thresholds for predicting olfactory dysfunction, and logistic regression modelling to assess dose-dependent risk while adjusting for potential confounders. A two-sided P value <0.05 was considered statistically significant.
Of the 99 enrolled patients, 63 met the inclusion criteria and were included in the final analysis (median age = 55 years, male = 82.5%). Most patients had advanced-stage disease and received concurrent chemoradiotherapy. The medial total RT dose was 68 Gy, and the mean dose to the olfactory region was 23 Gy (range 6-62 Gy). Longitudinal analysis showed a general decline in olfactory scores after RT, with partial recovery observed in some patients during follow-up. Patients receiving lower radiation doses to the olfactory region maintained relatively stable olfactory function.
Linear regression analysis revealed a moderate dose-response relationship, with a regression slope of 0.128, which indicates that each 1-Gy increase in radiation dose to the olfactory region was associated with a mean decrease of 0.128 points in TWSIT score. ROC curve analysis identified 22 Gy as the optimal cutoff dose for estimating olfactory dysfunction (area under the curve [AUC]: 0.74, 95% confidence interval [CI]: 0.52 to 0.96, sensitivity: 64%, specificity 92%, P = 0.03). Patients receiving less than 22 Gy had a greater than 90% likelihood of preserving normal olfactory function, whereas about 64% of those exposed to higher doses developed olfactory dysfunction. Logistic regression modelling demonstrated a dose-dependent increase in dysfunction probability with an inflection point at about 22 Gy. Multivariable analysis confirmed that a mean olfactory region dose exceeding 22 Gy was an independent risk factor for olfactory dysfunction (odds ratio: 20.65, 95% CI: 2.60 to 164.35). Olfactory scores declined early after RT and showed minimal recovery over 12 months in patients exposed to doses above this threshold.
This clinical trial indicates that the olfactory dysfunction after RT for HNC is dose-dependent, specifically with a critical threshold at approximately 22 Gy. Radiation doses above this level significantly increase the risk of persistent olfactory impairment for up to one year post-treatment. These findings highlight the importance of careful RT planning to decrease exposure to the olfactory region and suggest that preservation of olfactory function should be considered a key objective in optimizing radiation dose delivery to improve long-term quality of life in patients with HNC.
Reference: Chang G, Tsai Y, Lin M, et al. Radiotherapy and Smell Function in Head and Neck Cancer: A Nonrandomized Clinical Trial. JAMA Netw Open. 2025;8(12):e2548547. doi:10.1001/jamanetworkopen.2025.48547