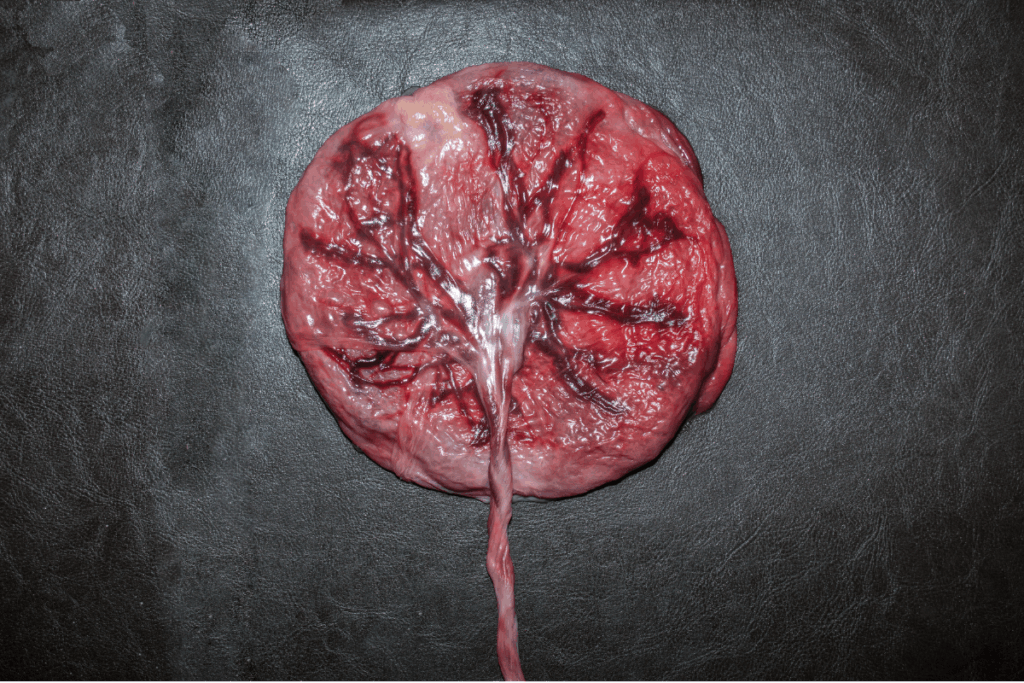
Placenta accreta spectrum (PAS) disorders are increasingly common globally, paralleling rising cesarean delivery rates. They are the leading cause of severe maternal morbidity because of hemorrhage and surgical complications. However, earlier uterine surgery and scarring are well-established clinical risk factors, and the biological mechanisms underlying abnormal placental adherence are not completely understood. PAS was attributed to excessive trophoblast invasion, but new data suggest that defects in maternal decidua and extracellular matrix (ECM), instead of intrinsic trophoblast aggressiveness, create a permissive environment for pathological placentation. Collagen is a principal structural component of the ECM and a key determinant of tissue integrity and wound repair. Collagen types I and III are critical for uterine scarring, strength, and repair, yet their spatial organization at the maternal-fetal interface has not been systematically studied in PAS.
The aim of this study was to assess whether abnormal collagen architecture and ECM remodeling contribute to defective decidual healing and subsequent placental adherence in PAS. To test this, structural imaging with functional assays in human tissues, animal models, and a novel in vitro system, which enables both mechanistic and descriptive investigation of collagen dynamics, inflammation, and trophoblast behavior.
A multimodal experimental approach was used. Human placental-decidual specimens were collected from patients with intraoperatively confirmed PAS and matched non-PAS cesarean controls. Biopsies from nonadherent and adherent regions were analyzed by using second harmonic generation (SHG) microscopy and fluorescence lifetime imaging microscopy (FLIM). A mouse model of uterine injury was used to induce scarring under hormonally distinct conditions, followed by pregnancy, to evaluate placental adherence and collagen organization at the decidual-placental interface.
An in vitro accreta-in-a-dish co-culture system was developed using decidualized human uterine fibroblasts, trophoblast-like cells, and macrophages. Electrical cell substrate impedance sensing (ECIS) was used to qualify wound healing and scar resistance. While live cell imaging and SHG microscopy assessed ECM formation and trophoblast spatial localization.
Results consistently demonstrated significant alterations in collagen architecture at sites of placental adherence across all models. In human PAS specimens, SHG imaging revealed elevated but disorganized fibrillar collagen at adherent sites with indistinct borders between placental and decidua and collagen extending abnormally in placental villi. Three-dimensional imaging highlighted complex and interdigitating collagen networks unique to PAS adherence sites. Mouse models recapitulated these findings, showing bulky, poorly organized collagen and disrupted decidual-placental borders in accreta compared with sham and control surgeries, regardless of the method used to induce scarring.
Functional in vitro studies provided mechanistic insights. Collagen coating significantly accelerated wound closure and elevated scar resistance in decidualized uterine fibroblasts, which indicates a protective role for collagen in uterine repair. Decidualized fibroblasts were shown to be the sole producers of de novo ECM. Trophoblast did not contribute to matrix deposition. Trophoblast-like cells preferentially migrated in ECM-poor wounded areas and avoided collagen-rich regions. This suggests that matrix composition and organization guide trophoblast localization. Inflammatory conditions, models by macrophage co-culture, weakened scar resistance, and impaired wound healing.
This study shows that PAS is linked to abnormal collagen architecture and ECM remodeling at uterine scars. Defective decidual healing, reduced scar resistance, and inflammation, rather than excessive trophoblast invasion, drive pathological placental adhesion. Human, animal, and in vitro models suggest that targeting collagen remodeling and inflammation may improve scar integrity and reduce PAS risk.
Reference: Ligumsky L, Jeong A, Martinez G, et al. Placenta accreta spectrum: disrupted collagen architecture at a previous scar is a defining characteristic of placental adherence. Am J Obstet Gynecol. 2026;233(6):S645-S661.e1. doi:10.1016/j.ajog.2025.08.094