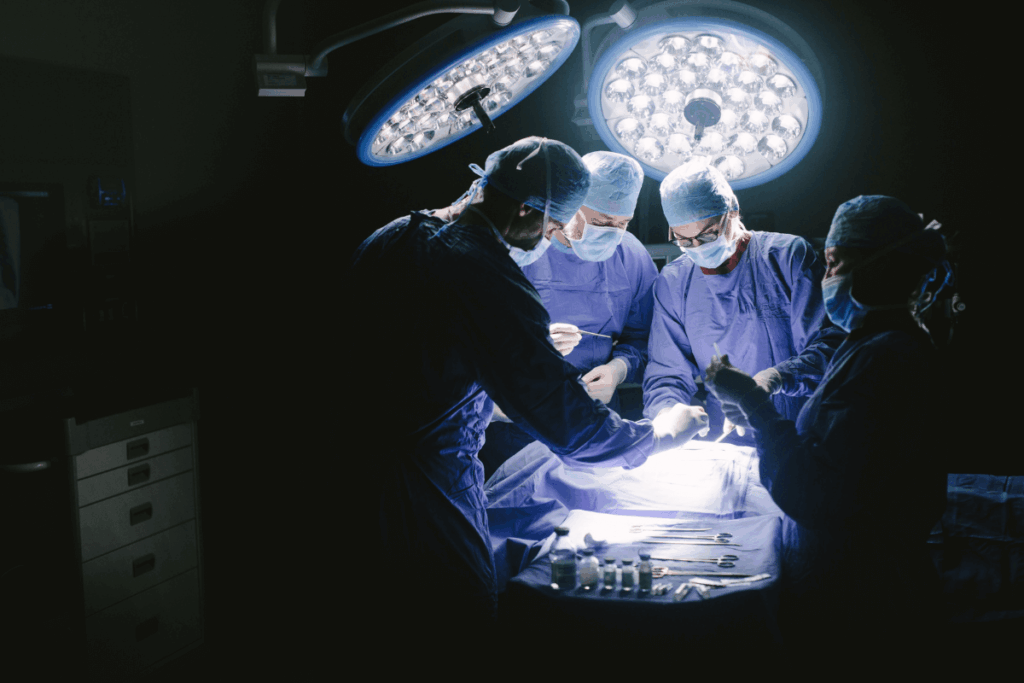
Pharmacological agents used to achieve general anaesthesia in laparoscopic surgery are usually associated with hemodynamic instability, delayed recovery, and postoperative nausea. Non-pharmacological adjuncts like music therapy have demonstrated potential in reducing perioperative stress, regulating autonomic responses, and decreasing anaesthetic needs. Studies suggest that auditory pathways might not be entirely inactivated during anaesthesia, which means that music can have an impact on stress and perception of pain by reducing sympathetic activity, lowering serum cortisol levels, and enhancing endogenous opioids and oxytocin.
The aim of this randomized controlled trial was to determine whether intraoperative music therapy reduces the total propofol requirement in adult patients undergoing laparoscopic cholecystectomy under total intravenous anaesthesia (TIVA) with bispectral index (BIS) monitoring. Secondary outcomes included additional fentanyl needs, quality of awakening, serum cortisol variation, and patient satisfaction.
A randomized controlled trial was conducted to determine the effect of intraoperative music therapy on propofol intake in the adult population undergoing laparoscopic cholecystectomy. This approach reflects the increasing interest in non-pharmacological modalities to minimize perioperative stress, anaesthetic needs, and hemodynamic fluctuations. Music therapy has been linked to reduced sympathetic activity, lower serum cortisol, and elevated endogenous opioids and oxytocin, suggesting that it may reduce pain and stress even under general anaesthesia by maintaining the activity of the auditory pathway.
Based on these considerations, the researchers investigated whether instrumental music selected by patients could decrease propofol use and influence perioperative physiological and recovery outcomes. A total of 56 ASA I-II patients aged 18-65 years scheduled for laparoscopic cholecystectomy between March 2023 and January 2024 were enrolled following institutional ethics approval and registration of the study in the Clinical Trials Registry of India (CTRI). Participants were randomized into two groups: music group (M, n = 28) and the control group (C, n = 28).
Group M listened to non-lyric and instrumental flute or piano music at a slow tempo (60-100 beats per minute) through noise-cancelling headphones at 60 dB throughout the surgery, while group C wore identical headphones without sound. Propofol was then used to induce anaesthesia using the Schneider model via a Target-Controlled Infusion (TCI) pump with an initial effect-site concentration of 3 mcg/ml, which was adjusted to keep the BIS within the range of 40 to 60. Each patient was induced with fentanyl at 2 μg/kg, with additional doses of 0.5mg/kg given if heart rate or mean arterial pressure exceeded baseline values.
Serum cortisol was measured one hour before and one hour after surgery. The quality of awakening was measured using the Riker Sedation Agitation Scale (RSAS), whereas postoperative pain and patient satisfaction were evaluated by standardized scoring tools. The groups did not differ in demographic characteristics, such as age (35.14±9.22 vs. 33.39±9.07 years), gender distribution (4/24 in both groups), weight, and the level of preoperative serum cortisol (249.93±99.292 vs. 254.29±128.546 IU/ml; P=0.838).
The primary outcome demonstrated a significant reduction in the intake of propofol in group M (6.7082±0.96412 mg/kg/hr) versus group C (7.8643±1.43 mg/kg/hr; P=0.001). Additional fentanyl use was also lower in Group M was also much lower (0.64±0.678 vs. 1.04±0.637; P=0.003). Group M showed a lower systolic, diastolic, and mean arterial pressure at 30-45 minutes of surgery (P<0.05), indicating improved hemodynamic stability, which could be attributed to reduced catecholamine release.
There was an improvement in the cortisol level of both groups, but it was significantly lower in group M (417.82±142.651 IU/ml) compared to group C (536.18±140.909 IU/ml; P=0.004), which is indicative of an attenuated cortisol response. The music group was more favourable in terms of quality of emergence, as the RSAS scores were higher (3.64±0.488 vs. 4.00±0.272; P=0.001). One-hour postoperative pain scores (2.12+0.94 vs. 2.59+1.1; P=0.07) and 24-hour patient satisfaction (P=0.361) were similar between groups.
Overall, the patient-selected instrumental music therapy is a safe and effective non-pharmacological adjunct in laparoscopic surgery. It reduces propofol and fentanyl requirements, enhances hemodynamic stability, and reduces cortisol-mediated perioperative stress without any adverse effects.
References: Goel T, Husain F, Wadhawan S, et al. Effect of music therapy on propofol consumption in patients for laparoscopic cholecystectomy under TIVA (Total Intravenous Anaesthesia). Music & Medicine. 2025;17(4):212-218.