Peripheral neuropathy is a pain disorder that is common and experienced in various diseases, including diabetes and following chemotherapy. Primary sensory neurons in the dorsal root ganglia (DRG) possess long axons and have high mitochondrial demands, and mitochondrial dysfunction has been linked to peripheral neuropathy in both diabetes and chemotherapy.
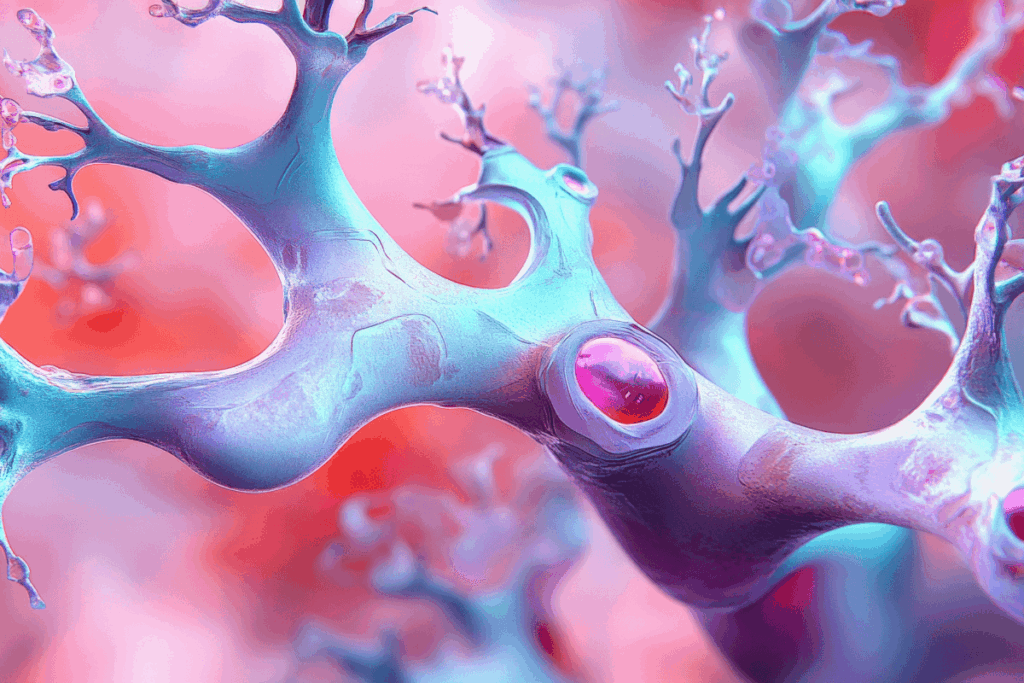
Satellite glial cells (SGCs) tightly enclose the sensory neurons’ cell bodies in the DRG, regulate neuronal activity and pain; however, the structural and metabolic support mechanisms of these processes are poorly understood. This study investigated the ability of SGCs to deliver mitochondria to sensory neurons directly and whether this mechanism could prevent or alleviate peripheral neuropathy. To examine mitochondrial transfer, the researchers used in vitro cell culture systems, ex vivo DRG tissue, and in vivo mouse models.
To monitor the movement of mitochondria, mouse SGCs were labelled with mitochondrial dyes and co-cultured with sensory neurons. Tunnelling nanotube-like structures (TNTs) were visualized using advanced imaging techniques such as live-cell imaging, scanning electron microscopy (SEM), transmission electron microscopy (TEM), and structured illumination microscopy. In genetically modified MitoTag mice, mitochondria were specifically labeled in SGCs to permit the transfer of the mitochondrial structure to the neuron to be traced in living animals. Pharmacological blockers were used to inhibit TNT formation, endocytosis, or gap junctions. The role of motor protein, MYO10, was also tested using si-RNA mediated knockdown and Myo10+ /- mice.
Human DRG samples from diabetic and non-diabetic donors were analyzed using SEM, immunostaining, in situ hybridization, and single-nucleus RNA sequencing. Finally, adoptive transfer of mouse or human SGCs into neuropathy mouse models was performed to evaluate therapeutic efficacy.
In vitro, SGCs transferred mitochondria to DRG neurons in 83.3% of cases, although TNTs were observed in only 31.3% of cells at any given time, supporting the transient nature of these structures. Mitochondrial transfer was inhibited by tetrodotoxin, indicating dependence on neuronal activity, and was markedly reduced by blocking TNT formation, endocytosis, or gap junctions.
In vivo, mitochondrial transfer increased over time, where 2.9% of neurons were positive at day 5 and 23.0% at day 10, post-induction. Transfer was inhibited by blocking TNTs or endocytosis. Mitochondrial transfer had been hampered in diabetic streptozotocin-induced mice, in whom diabetes was induced in advance. Following nerve injury, mitochondrial transfer increased on the injured side and required neuronal activity. Neurons that received transferred mitochondria had a low probability of hyperactivity.
MYO10 was highly expressed in SGCs, and its knockdown or partial loss reduced TNT formation, impaired mitochondrial transfer, and increased pain sensitivity. TNT-like structures were also observed in human DRG samples. In diabetic donors, MYO10 expression in SGCs was markedly reduced, and mitochondrial transfer to neurons was diminished.
Adoptive transfer of healthy human or mouse SGCs into neuropathy models significantly reduced neuropathic pain; however, this effect was abolished when MYO10 was suppressed. This study indicates an unidentified protective action of peripheral glial cells. To meet neuronal energy requirements and reduce hyperactivity and degeneration, SGCs actively exchange mitochondria to sensory neurons via TNTs, which are dependent on MYO10. The impairment of this process is one of the causes of peripheral neuropathy in diabetes and chemotherapy. Notably, restoring healthy SGCs or mitochondria transfer represents a promising therapeutic approach for neuropathic pain.
Reference: Xu, J., Li, Y., Novak, C. et al. Mitochondrial transfer from glia to neurons protects against peripheral neuropathy. Nature. 2026. https://doi.org/10.1038/s41586-025-09896-x












