Understanding how inflammation resolves in humans remains a major challenge, particularly because failures in resolution can lead to chronic inflammatory diseases. Although numerous inflammatory mediators have been identified, relatively few pathways governing the resolution phase of inflammation have been well characterized. One largely unexplored system involves cytochrome P450–derived epoxy-oxylipins, lipid mediators formed from polyunsaturated fatty acids and metabolized by epoxide hydrolase enzymes. While these mediators have demonstrated anti-inflammatory and analgesic effects in animal models, their roles in human inflammation have remained unclear.
In a study published in Nature Communications (2026), researchers investigated the effects of epoxy-oxylipins on immune cell behavior during acute resolving inflammation in humans, with a particular focus on monocyte differentiation and inflammatory resolution. This study employed a previously published human model of acute inflammation in which healthy male volunteers received an intradermal injection of UV-killed Escherichia coli. The study included 24 healthy male volunteers aged 18–50 years in the prophylactic arm and 25 healthy male volunteers in the therapeutic arm.
Participants received 15 mg of GSK2256294, a selective soluble epoxide hydrolase (sEH) inhibitor, administered either 2 hours or 4 hours before the induction of inflammation, depending on the study arm. Blood samples, skin biopsies, and inflammatory exudates were taken at various time points to measure the levels of enzyme expression, lipid mediators, clinical manifestations of inflammation, and immune cell populations. The level of epoxy-oxylipin and monocyte subsets was assessed with advanced lipidomic analysis and flow cytometry.
Epoxy-oxylipins were detectable in both circulation and inflamed skin at baseline and during inflammation. Their synthesis and metabolism were dynamically regulated by enzymes such as CYP2C, CYP2J2, and sEH. Blockage of sEH using GSK2256294 resulted in a significant increase in the level of 12,13-EpOME and 14,15-EET, which is an indicator of successful enzyme inhibition. While sEH inhibition did not alter tissue heat, redness, swelling, or blister volume, it significantly accelerated the resolution of pain.
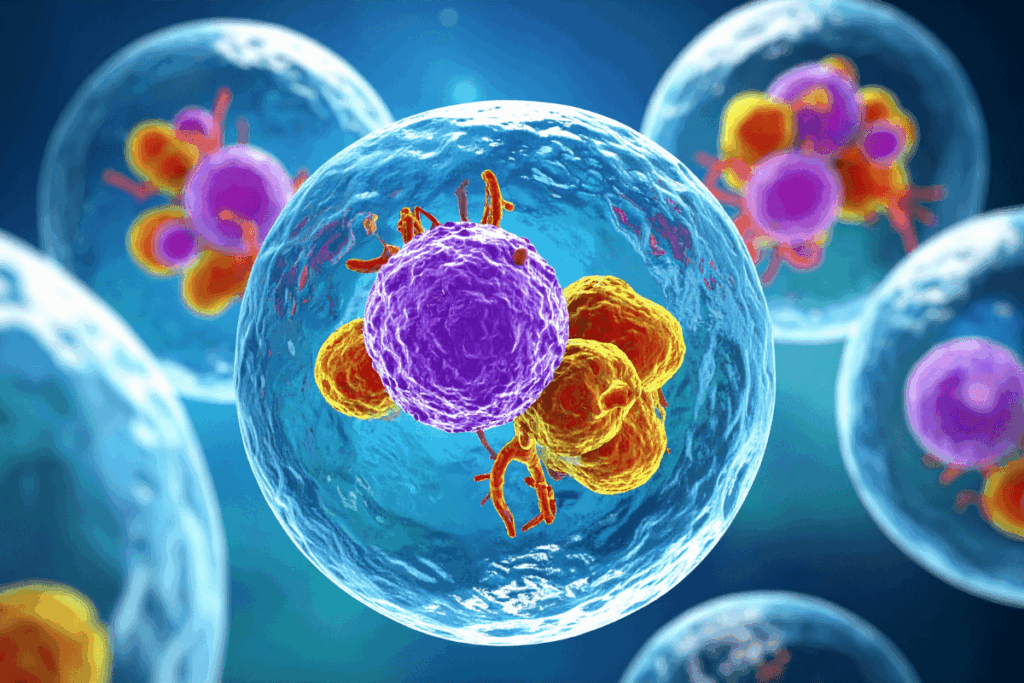
Another impressive immunological discovery was the monocyte effect. Inflammation generally causes an increase in intermediate monocytes in the blood and tissue.
Nevertheless, sEH inhibition greatly decreased the count of circulating intermediate monocytes and restricted their build-up at the inflammatory location. Mechanistic experiments indicated that 12,13-EpOME inhibited the transition of classical monocytes to intermediate monocytes by inhibiting the phosphorylation of p38 MAPK. These findings were corroborated both in vitro and in vivo using the p38 MAPK inhibitor losmapimod. Reduced tissue levels of intermediate monocytes were accompanied by fewer CD4⁺ T cells and decreased T-cell viability.
This study represents the first comprehensive characterization of the production, metabolism, and role of epoxy-oxylipin in human acute inflammation. The results indicate that sEH inhibition does not broadly suppress the immune responses but instead selectively modulates immune cell differentiation. Epoxy-oxylipins also appear to promote inflammatory immune resolution by restricting the expansion of intermediate monocytes through a p38 MAPK-dependent mechanism, without impairing essential inflammatory responses.
The dual role of the intermediate monocytes, supporting CD4⁺ T-cell survival while enhancing CD8⁺ T-cell cytotoxicity, highlights their complex contributions to inflammation and tissue outcomes. Given that sEH inhibitors are safe and well-tolerated in humans, these study findings represent a promising therapeutic strategy for selectively regulating pathogenic monocyte responses in chronic inflammatory conditions while preserving normal immune function.
Reference: Bracken OV, Jalali P, Glanville JRW, et al. Epoxy-oxylipins direct monocyte fate in inflammatory resolution in humans. Nat Commun. 2026;17:431. doi:10.1038/s41467-025-67961-5