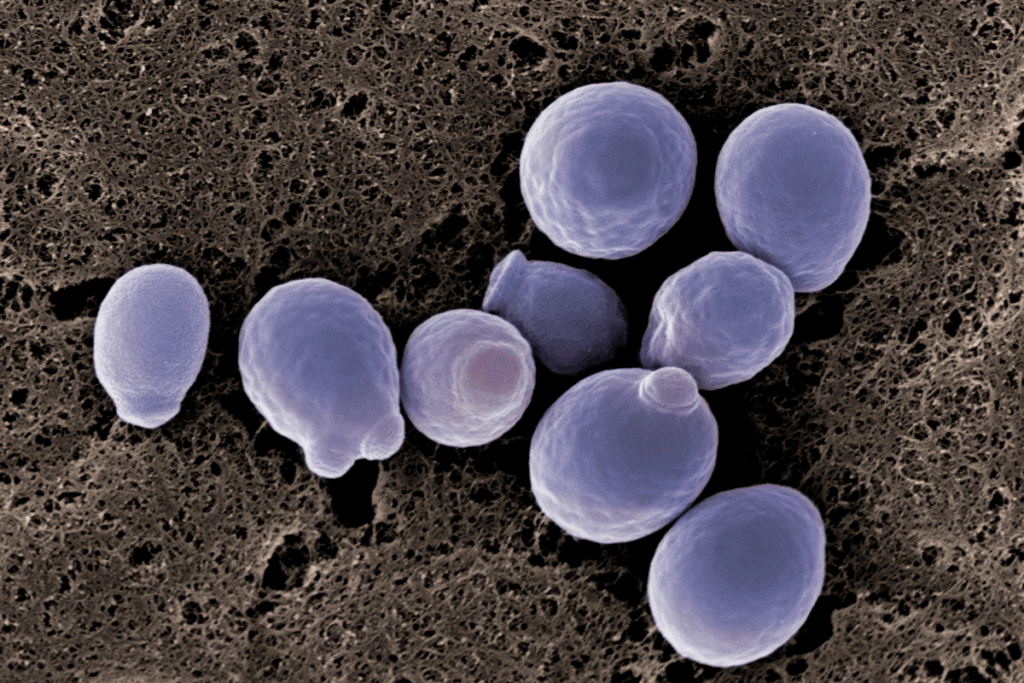
Thrush is a common infection caused by the yeast Candida albicans. It is becoming more difficult to treat because of the rapid increase in antifungal resistance, a trend with major global health implications. Although Candida infections can be treated with antifungal drugs like fluconazole, the primary treatment for most cases, an increasing number of Candida species, like C. albicans, are developing the ability to survive these medications. In the U.S., around 7% of Candida blood samples show resistance to fluconazole. In some regions, the rates can be higher. A 2024 study from Egypt found that about 26% of C. albicans blood isolates were resistant to this drug.
This represents a significant change from the early 2000s, when less than 5% of C. albicans infections were resistant. As resistance rates increase, treatment options for routine infections diminish, making even simple cases of thrush difficult to resolve and increasing the risk of severe infections, specifically in immunocompromised patients or those on prolonged antibiotic therapy. Antifungal resistance also contributes to the growing prevalence of recurrent thrush, which currently affects about 138 million women and is expected to increase to 158 million by 2030.
The adaptability of C. albicans underlies this problem. The fungus readily develops genetic mutations that decrease drug susceptibility, change molecular targets of antifungals, and form biofilms, tough, slimy layers of fungal cells that block drugs, sequester medications that penetrate, and allow dormant persister cells to survive treatment. These survival methods enable Candida to thrive even in hostile, drug-rich environments.
The rise in resistance is not occurring randomly; it is accelerated by environmental pressures and human behaviors. Misuse and overuse of antifungal drugs in both agriculture and medicine create strong selective pressures that favour resistant strains. The limited number of effective antifungal drugs, combined with the high cost and difficulty of developing new agents, means that fungi repeatedly face the same treatments and increasing opportunities to evolve defenses. Environmental factors like increasing temperature, ecological disruption, and widespread agricultural fungicide usage contribute to the increase of heat-tolerant and drug-resistant species like Candida auris, which is highly pathogenic and resistant to multiple drug classes.
Candida typically spreads through direct person-to-person contact, sexual contact, or contaminated surfaces and medical equipment. Airborne transmission has traditionally been considered rare. However, a recent study detected drug-resistant Candida, including C. albicans, in urban air in Hong Kong, raising concerns about an earlier underestimated route of exposure, specifically in crowded public settings or healthcare facilities.
Under normal circumstances, Candida lives harmlessly in the body, kept in check by a balanced microbiome. When this balance is disrupted by antibiotics, poor diet, stress, or a weakened immune system, the fungus can grow unchecked, and infections become more likely. Microbiome disruption creates an environmental condition in which resistant strains thrive and form durable biofilms.
Maintaining a healthy microbiome is therefore a key defense. Consuming a diverse, fiber-rich diet with fermented foods, limiting processed foods, taking antibiotics only when needed, and incorporating probiotics or prebiotics when appropriate can help sustain microbial balance and reduce infection risk. To prevent further resistance, collective action is essential: use antifungal medications exactly as prescribed, complete full treatment courses, limit unnecessary antifungal use in humans and agriculture, and maintain good hygiene practices to reduce transmission and preserve the effectiveness of existing antifungal drugs.
Reference: Mohammed M. Antifungal resistance is making thrush hard to treat – here’s why. The Conversation. Published December 1, 2025. Accessed December 2, 2025. Antifungal resistance is making thrush hard to treat – here’s why











