A new study published in The Menopause Society in Orlando highlights dry eye disease (DED) as an underrecognized problem. It becomes more frequent in women undergoing menopause. Menopause is linked to symptoms like night sweats, hot flashes, and vaginal dryness. Researchers found that hormonal changes during this transition significantly affect ocular health and increase the risk of DED in midlife and post-menopausal women.
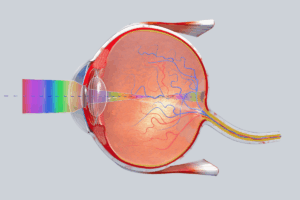
DED is a multifactorial condition in which the eyes either fail to produce sufficient tears or tears evaporate too quickly. This can lead to dryness, irritation, inflammation, redness, and a sensation of grittiness or burning. If it is not managed properly, DED can lead to corneal surface damage and recurrent eye infection, potentially impairing vision. Common risk factors include allergy, advancing age, autoimmune disease, and usage of medications like antihypertensives and antidepressants. Hormonal fluctuations, specifically in androgens and estrogen, play an important role in altering tear film composition and reducing tear gland output.
This study led by Debora Yankelevich of Hospital de Clínicas José de San Martín in Buenos Aires, Argentina. It used a cross-sectional analysis observational design. It assessed more than 3500 females with an average age of 52 years to evaluate the prevalence and severity of DED in premenopausal women. Perimenopausal and postmenopausal individuals. They used the Ocular Surface Disease Index (OSDI) questionnaire to assess dryness, eye discomfort, and vision-related symptoms. It also evaluates the links between DED and variables like autoimmune disease, contact lens use, and smoking to evaluate menopause as a potential risk factor.
Results showed that 57.38% of postmenopausal women have consistent symptoms with DED as compared to 53.22% of premenopausal women. This indicates a measurable increase in DED prevalence after menopause. This hormonal decline in menopause, specifically reduced estrogen and androgen levels, can impair lacrimal gland function and destabilize the tear film, and increase dryness. It also revealed that external influences like tobacco use and contact lens wear worsen the condition by accelerating tear evaporation. Autoimmune diseases, such as Sjögren’s syndrome and rheumatoid arthritis, were identified as additional risk factors, as they can alter the tear gland function by chronic inflammation.
According to Debora Yankelevich, the results underscore the need for clinicians to screen for DED in menopausal patients. “Clinicians should add dry eye disease to their regular assessment checklists,” she explained. Early detection is key to preventing complications and maintaining ocular health.
Dr. Stephanie Faubion, a medical director of The Menopause Society, highlighted the larger implications of the results, specifically the relationship between aging, hormonal shifts, and eye health. She stated, “We continue to learn about the effects of hormonal changes on women’s ocular health during midlife. Early identification of dry eye disease allows healthcare providers to initiate personalized treatment strategies that preserve comfort, visual clarity, and surface integrity.”
This research identifies menopause as a key risk factor for DED along with contact lens use, smoking, and autoimmune disease. Recognizing DED early allows clinicians to initiate timely treatment, improving visual comfort and preserving long-term eye health during and after menopause transition.
Reference: The Menopause Society. Risk of Dry Eye Disease Increases During Menopause Transition. Press release. Cleveland, OH; October 15, 2025. Accessed October 29, 2025. Risk of Dry Eye Disease Increases During Menopause Transition