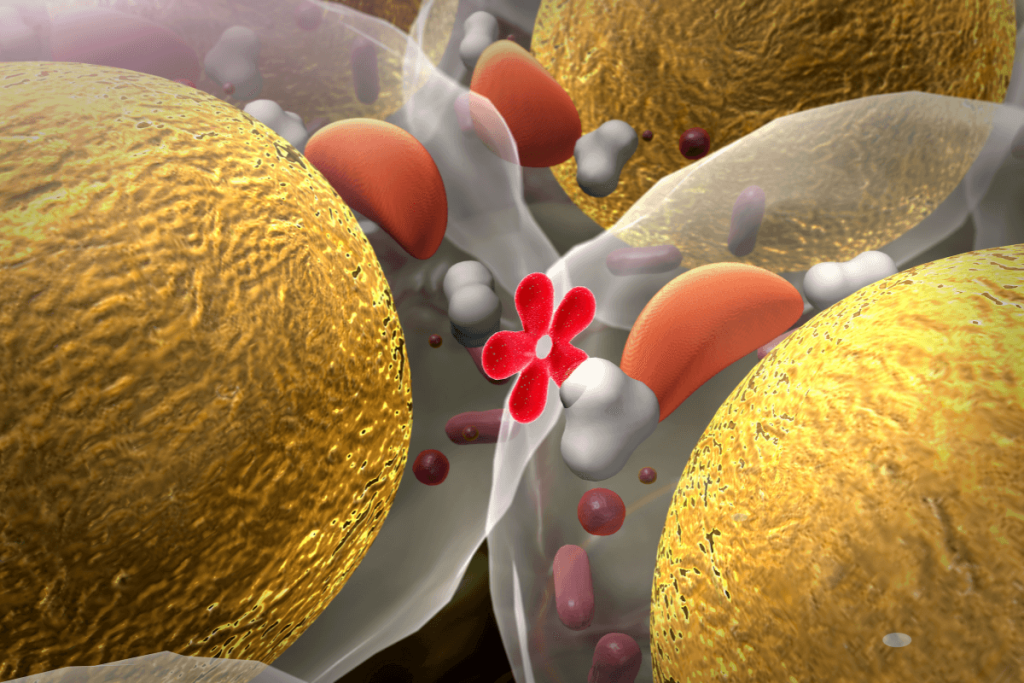
Type 2 diabetes is caused by β-cell dysfunction and impaired insulin secretion. The underlying molecular and cellular mechanisms are not completely understood. Recent advances in single-nucleus and single-cell RNA sequencing (snRNA-seq and scRNA-seq) have shed light on the complex heterogeneity of pancreatic islet cells. These technologies enable the identification of distinct subpopulations of β and α cells, the potential of transition to cell states, and their gene expression profiles. It is crucial to understand these dynamics to uncover the cellular pathways involved in T2D progression and to identify novel therapeutic targets.
This study aimed to define α-cell heterogeneity in adult human islets, transcriptional pathways between β and α cells, and targeted genes implicated in α-cell plasticity and β-cell dedifferentiation in T2D. The primary focus was to understand the role of the gene SMOC1, which has been newly linked to β-cell dysfunction in diabetes.
The researchers combined snRNA-seq and scRNA-seq datasets from the human islets of T2D and non-diabetic donors. They used stringent computational filters to exclude ambient RNA contamination and cell doublets. Clustering analysis revealed various α-cell subtypes based on gene expression profiles. Pseudotime and RNA velocity trajectory analyses were used to recreate differentiation pathways between α and β cells. Comparative gene expression profiling helped identify genes linked to cell state transition and diabetes-related dysfunction in T2D and non-diabetic islets. Functional investigations evaluated the effects of SMOC1 on insulin secretion, gene expression, and β-cell calcium influx.
Five distinct α-cell subclusters are α1, α2, α3, α4, and a bihormonal AB cluster expressing both glucagon (GCG) and insulin (INS) were five distinct α cell subclusters. The α1-α4clusters showed the typical α cell gene signatures and translation pathways with α2 cells, which were enriched for cell cycle-related genes of proliferative activity. The AB cluster-expressed genes were linked to the pancreatic progenitors and β cells pathway, which supports a progenitor-like or translational identity instead of an artifactual doublet. These results matched those of an earlier study, which also showed the same α cell state in cross-species and human islet analyses.
Trajectory analysis revealed that AB cells have a root position in the bifurcated differentiation pathway leading to mature α and β cells in non-diabetic islets. T2D islets showed unidirectional trajectories to α cells from β cells. This is consistent with β-cell dedifferentiation or conversion to α-like states in response to diabetic stress.
There was a 10-gene set identified from the analysis of trajectories from AB to α cells, which were ZNF331, PLCE1, PAPPA2, TM4SF4, NR4A1, BTG2, SLC30A8, PCSK2, SMOC1, and ALDH1A1. Many of these genes were known or suspected to have roles in α cell specification, β cell function, or diabetes pathology. PLCE1 potentiates GSIS, reduced in β cells but elevated in α cells in T2D. This suggests that there is an involvement in β-cell dysfunction. PAPPA2 is upregulated in T2D α cells and can inhibit insulin-like growth factor binding proteins and maintain α cell identity, limiting α to β reprogramming.
SMOC1 is an α-cell-specific gene in healthy islets that is aberrantly expressed in β cells from T2D donors. Functional assays showed that SMOC1 impairs β-cell calcium influx, maturation of insulin granules, and GSIS. They are essential for effective insulin secretion. SMOC1 reduced cAMP production in response to GLP1 receptor agonists and diminished the efficacy of incretin therapies. This effect was mediated by reduced GLP1 receptor expression or interaction of SMOC1 with signaling pathways like BMP-2.
This study enhances our understanding of the diversity of pancreatic islet cells by identifying five α-cell subtypes and reveals a dynamic transition in β-cell identities. In T2D, β cells lose their identity and transform into α-like cells, contributing to β cell failure. A common set of genes is involved in this change. SMOC1 was a novel diabetes-associated gene. Elevated SMOC1 in β cells impairs insulin secretion by altering calcium influx and cAMP signaling. It can reduce the efficacy of GLP1 receptor therapies. Targeting SMOC1 or its pathways can help preserve β-cell function, but careful techniques are required due to the complex systemic effects. Future studies will focus on the mechanisms of SMOC1 and other genes that are involved in α and β cell plasticity to improve diabetic treatment.
Reference: Kang RB, Varela M, Oh E, et al. Human pancreatic α-cell heterogeneity and trajectory inference analyses reveal SMOC1 as a β-cell dedifferentiation gene. Nat Commun. 2025;16:8434. doi:10.1038/s41467-025-62670-5











