Functional seizures are brief episodes that resemble epileptic seizures or fainting but are not caused by abnormal electrical activity in the brain. Instead, they are thought to arise from dissociation or other cognitive and emotional processes. These events are also called dissociative seizures, psychogenic nonepileptic seizures, or conversion disorder with seizures.
Importantly, functional seizures are unintentional and should not be mistaken for malingering or factitious disorders. The functional seizures are a widespread and debilitating type of functional neurologic symptom disorder. They are frequently complicated biological, psychological, and social causes.
Some patients have co-occurring psychiatric conditions or a history of negative events in life, like sickness, injury, neglect, or abuse, but these are not applicable to all patients and are not required for diagnosis. Children who are affected by functional seizures are less likely to have such associations.
Even though increasing evidence supports the idea that psychological interventions can decrease seizure frequency and improve the quality of life, as well as decrease health care expenses, most individuals with functional seizures fail to receive proper care.
Examples of barriers are stigma, lack of coordination between neurologists and mental health clinicians, poor access to psychotherapy, low reimbursement of counseling services, and the unawareness of clinicians and the general population.
To address these gaps, the American Academy of Neurology (AAN) developed evidence-based practice guidelines for the management of functional seizures. The guideline was developed by a multidisciplinary panel based on the 2017 Guideline Development Process of the AAN. Most of the panel members, including the principal author, were conflict-free (at least 51%). The panel examined Medline, Embase, PsychINFO and CINAHL evidence and discovered 12 relevant studies. AAN criteria were used to rate each of the studies independently.
Some of the psychological interventions that were reviewed by the guideline include functional seizure-specific cognitive behavioral therapy (CBT), neurobehavioral therapy, Retraining and Control Therapy (ReACT), behavioral therapy, psychoeducation, motivational interviewing, and group therapies. Most interventions took 3-12 sessions, with follow-up data up to 1 year.
Overall, psychological interventions are potentially likely to raise the probability of seizure freedom. Out of 7 Class III studies, the pooled risk ratio was 1.87 (95% confidence interval [CI]: 1.36 to 2.56), indicating seizure freedom. This also has a potential frequency of reduction of the seizure frequency of these treatments, a pooled standardized mean difference of -0.81.
Psychological interventions have the potential to enhance health-related quality of life, and the pooled standardized mean difference is 0.37. But there are not enough data to ascertain regular influences on the severity of seizure, depression, or anxiety.
Positive outcomes were still observed when the emphasis was laid on functional seizure-specific CBT. CBT potentially enhances the level of seizure freedom with a pooled risk ratio of 1.76 (95% CI: 1.10 to 2.80) and potentially may enhance psychosocial functioning.
Limited evidence exists on the effects on the frequency, quality of life, anxiety, and depression. It reviewed three studies, two of which were on drugs, such as sertraline and diazepam. The evidence did not provide enough evidence to show whether sertraline increases the freedom from seizures, the frequency of seizures, the quality of life, the psychosocial functioning, anxiety, or depression. Diazepam also did not have enough evidence of benefit and has risks of dependence, cognitive impairment, and iatrogenic harm.
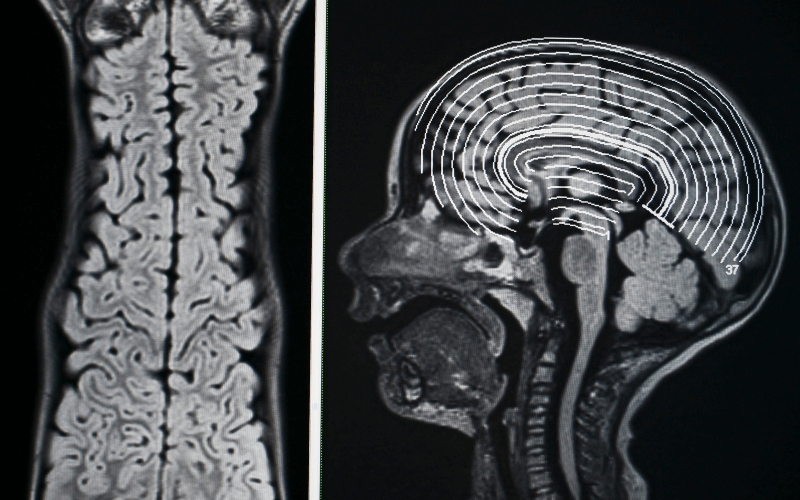
The guideline also emphasizes early and correct diagnosis, where the diagnosis is usually delayed by 7-8 years. The video-EEG monitoring is the gold standard, but history, witness descriptions, physical examination, and smartphone videos could be helpful in the diagnosis. Patients should be assessed by clinicians in terms of psychiatric comorbidity and co-occurring epilepsy, which may be present in up to 20% of adults and 30 to 40% of children with functional seizures.
Respectful communication, shared decision-making, continuity of care, and collaboration between neurologists and mental health professionals should be given priority in treatment. Whenever possible, psychological therapies need to be provided, whereas the antiseizure drugs and benzodiazepines are to be avoided unless otherwise. The guideline concludes by calling for more research to strengthen the evidence base and improve care for people living with functional seizures.
Reference: Tolchin B, Goldstein LH, Reuber M, et al. Management of Functional Seizures Practice Guideline Executive Summary Report of the AAN Guidelines Subcommittee. Neurology. 2026;106:e214466. doi:10.1212/WNL.0000000000214466












