Background
Venous thrombosis is one of the leading causes of morbidity and mortality in the United States and is one of the most frequent causes of presentation to an emergency department. Deep vein thrombosis (DVT) can cause thromboembolism, chronic venous insufficiency, and pulmonary embolism (PE), which can be fatal. Pulmonary Emboli, which are among the most preventable causes of death, are reported to develop initially in the lower extremities in about two thirds of patients. The development of PE is assumed to be as frequent as 10 to 50% if untreated, resulting from DVT. Prompt diagnosis and the initiation of anticoagulation or, in some cases, the placement of a Greenfield filter is extremely successful.
Compression ultrasonography as a method for diagnosing lower extremity DVT is proven to be equally sensitive and specific compared to other methods that use radiation or contrast agents. Conventional lower extremity Doppler studies, which evaluate the blood vessels in the entire limb, are done by ultrasound technicians and reported by radiologists. Still, these processes can take as long as two hours and slow diagnosis and treatment.
Patients with risk factors for DVT or PE should receive a diagnostic workup, which frequently involves using bedside compression ultrasound. Although contrast venography is the gold standard for DVT diagnosis, point of care ultrasound (POCUS) is being used in more EDs for lower extremity DVT assessment. Two main POCUS techniques are employed: the 2-point method, based on the compressibility of the common femoral vein (CFV) and popliteal vein (PV), and the 3-point method including the superficial femoral vein (SFV).
Current EDs preferentially employ a variation to the 2-point compression technique that targets high-risk regions for DVT, takes less than five minutes, and has comparable diagnostic sensitivity and specificity. A negative DVT compression ultrasound can help avoid the use of anticoagulant agents in patients suspected of having DVT. The 2-point compression method has been used in many studies and is widely accepted when used with pretest probability assessments.
Indications
Leg Pain: Cramp or burning pain in one leg which may be constant or develop suddenly; this would be due to obstruction of blood flow in deep veins.
Tenderness: Leg tenderness and discomfort on pressure, especially on the calf, may indicate venous thrombus formation.
Swelling: One of the main symptoms of DVT is the swelling or edema of one leg that may occur due to the clot blocking blood flow.
Erythema: Swelling of the leg may be accompanied by redness or warmth due to inflammation that is associated with a blood clot.
Positive Homans’ Sign: The presence of tenderness on compression of the calf or dorsiflexion of the foot during physical examination may indicate DVT though it is non-specific.
Evidence Supporting POCUS for Lower Extremity DVT
Sensitivity and Specificity
Various investigations by the experts have over the years shown that POCUS by physicians in the emergency department is very effective in diagnosing DVT. In a 1997 study, Jolly et al. showed 100% sensitivity for the duplex ultrasound in trained emergency physicians but this involved complete duplex exams and not the 2- or 3-point technique. Blaivas et al. (2000) applied a 2-point compression ultrasound which correlated with 98% of vascular lab studies. Other authors have published sensitivities of 100% and high specificities, for example, Magazzini et al. results and Jang et al. ’s results on POCUS conducted by emergency physicians and residents.
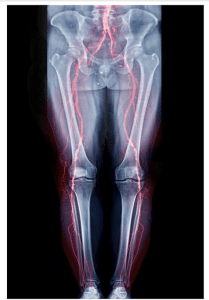
Lower Extremity DVT
In the HOCUS-POCUS study it concluded that using 3-point POCUS assesses by hospitalists, it achieved a sensitivity level of 100% and specificity of 95.8% after brief training. However, Caronia et al reviewed the data and pointed out that the 2-point technique employed by internal medicine residents failed to detect the isolated femoral clots.
In a meta-analysis performed by Lee et al., the authors determined that both 2-point and 3-point POCUS were equally effective, in terms of sensitivity and specificity for DVT diagnosis. In conclusion, POCUS has been shown to be highly accurate in diagnosing proximal DVT based on the existing evidence while acknowledging that accuracy can be reduced by variability in clinical context and clinician experience.
Contraindications
Outcomes
Equipment
Portable Ultrasound Machine: A portable, mostly in the form of a small unit that is easily carried and is laid on a bedside table. It also offers real-time imaging, making it useful in different specialties, including the emergency department, ICU or outpatient services.
High-Frequency Linear Probe (7-15 MHz): This probe is most suitable for delineation of superficial structures such as veins in the lower limbs. The high frequency is used to good effect here because it gives better definition of the venous system and clot identification in vessels such as the common femoral and popliteal veins are easier.
Ultrasound Gel: Used on the skin to improve the contact between the transducer of the equipment and the body’s surface to enhance the quality of the image as well as reception of the sound waves emitted by the equipment.
Screen or Display: It is attached to the ultrasound machine where it shows the real time picture of the images transmitted by the probe. Some of the modern POCUS devices may have features such as high-resolution touch screens to enhance usability.
Doppler Function: Some machines are Doppler optional to measure blood flow inside the veins which will help to determine the absence or presence of flow that may be suggestive of DVT.
Patient positioning
The patient needs to be laid on their back with the leg to be examined pulled up to the level of the inguinal ligament for a bedside ultrasound to determine deep vein thrombosis (DVT). There are two main positions of the patient during the exam: depending on the area that is being tested; however, the position may be adjusted to the patient’s comfort and ability. Ideally, positioning the patient with the head end of the bed raised to at least 30-40 degrees (reverse Trendelenburg) aids in increasing venous distention.
Femoral vein examination: The patient should be supine, and the hip flexed and externally rotated.
Popliteal vein examination: One must expose the back of the knee that is known as popliteal fossa. Either the patient can hang the leg over the side of the bed or, the patient can flex the knee and externally rotate the hip. Instead, they shall move sideways toward their side or extend flat onto the face (supine or prone) if required.

Patient positioning Point-of Care Ultrasound of Lower Extremity DVT
Femoral vein
Step 1-Position the Patient: Patient should be lying in a supine position with the hip flexed. The examination will be proceeded by evaluating the common femoral vein, which is situated just inferior to the inguinal ligament.
Step 2-Locate the Common Femoral Vein: Start with the inspection of the common femoral vein which is located right below the inguinal ligament. The femoral vessels are situated halfway between the pubic symphysis and the anterior superior iliac spine. The femoral artery that is usually felt to be pulsating can be used to determine the point of commencement.
Step 3-Prepare the Ultrasound Machine: Make sure that the application of the ultrasound gel to the transducer, and/or the patient’s leg is sufficient for good contact and image quality.
Step 4-Position the Transducer: Position the transducer in a transverse position inferior to the inguinal ligament with the probe marker pointing to the patient’s right side.
Step 5-Visualize the Vein Junction: Sweep the transducer in the cephalad or caudad direction to identify the junction of the common femoral vein and the greater saphenous vein. The common femoral artery will be located lateral to the common femoral vein.
Step 6-Apply Compression: Ensure the amount of pressure exerted by the transducer on the vein is firm and constant while compressing the vein. Lack of compression of the vein means that there is no DVT at this site in this case. Also, make sure that you exert enough pressure that will cause a slight deformation to the artery though.
Step 7-Confirm Compression: If the vein does not fully compress, there is a likelihood that a DVT is present in the leg. The ability to compress the vein fully excludes DVT, while if one can only partially compress the vein, then it is evident that a clot has formed. For DVT to be ruled in or out using ultrasound, compressibility is the most important criterion to consider.
Step 8-Examine the Veins: It is essential to double check whether there exists any compression in the femoral veins as well as the popliteal vein. Rotate the transducer as required to obtain adequate vein compression. It may be important to pay attention to the greater saphenous vein as some clot form at this section of the vein superficial and migrate to the common femoral vein. Evaluate this vein from 2cm proximal to 2 cm distal to this region.
Step 9-Proceed to the Popliteal Vein: If you have confirmed the absence of both deep and the superficial femoral vein, then proceed to check the popliteal vein.

Point-of Care Ultrasound of Lower Extremity DVT
Popliteal vein
Step 1-Position the Patient: Align the patient on the back when assessing the popliteal vessels.
Step 2-Prepare the Transducer: The ultrasound gel should be used on the transducer’s surface, the leg of the patient, or both to minimize air cavities.
Step 3-Position the Transducer: Position the transducer in the transverse plane of the popliteal fossa with the indicator facing the right side of the patient.
Step 4-Visualize the Vessels: To do this, the transducer is moved either cephalad (toward the head) or caudal (toward the feet) to locate the superficial popliteal artery and vein. The popliteal vein is commonly located posterior the popliteal artery, as its name implies, in the popliteal fossa. Because the posterior lobe of the probe shaft directs the ultrasonic beam towards the machine, the vein may look closer to the transducer compared to the artery.
Step 5-Adjust Probe Pressure: Alleviate the probe pressure if possible for better view of the veins as they are most compressible compared to the artery.
Step 6-Examine the Popliteal Vein: Make sure the examination area involves the distal 2 cm of the popliteal vein as well as proximal sections involving trifurcation of popliteal vein into the anterior tibial, the posterior tibial and the peroneal veins.
Step 7-Note Anatomical Variations: Know that the popliteal vein may bifurcate into the anterior and posterior tibial veins with the peroneal vein emerging from the posterior tibial vein.
Doppler Ultrasonography
Interestingly, Doppler ultrasonography is not a formal component of the focused lower-extremity compression examination for DVT; nonetheless, it is useful for visualization of the regional anatomy and assessment of ambiguous findings. However, Doppler ultrasound results cannot be relied on as a definitive sign of a clot.
Doppler ultrasound tests the velocity, direction, and turbulence of blood flow. Blood flow in both venous and arterial vessels possess distinctive features. In normal venous structures, there should be continuous venous flow that peaks on the compression of the calf, and venous flow should be affected by the respiratory movements, and this generally increases at the time of expiration. Compression of the calves helps to check obstruction distal to the probe while any respiratory changes can point to proximal obstruction in the iliac veins or the inferior vena cava.
Results
In a focused compression ultrasound exam for DVT, a fully compressible vein rules out the diagnosis of DVT and an incompletely compressible vein suggests the presence of DVT. It is vital to denote the location of the clot and more specifically, the area nearest to the clot to assess its advancement or withdrawal after treatment.
This means that while visualization of a clot and Doppler flow can give an indication that DVT may exist and require further follow up scans if clinically warranted, these alone are not sufficient for diagnosis of DVT.
Complications
There are no major risks or complications with the utilization of bedside ultrasound for diagnosing DVT. In this concern, there is no adequate literature that tries to advance any theory that clot propagation is instigated by manipulation of legs or compression of the vessels when performing the procedure.

Venous thrombosis is one of the leading causes of morbidity and mortality in the United States and is one of the most frequent causes of presentation to an emergency department. Deep vein thrombosis (DVT) can cause thromboembolism, chronic venous insufficiency, and pulmonary embolism (PE), which can be fatal. Pulmonary Emboli, which are among the most preventable causes of death, are reported to develop initially in the lower extremities in about two thirds of patients. The development of PE is assumed to be as frequent as 10 to 50% if untreated, resulting from DVT. Prompt diagnosis and the initiation of anticoagulation or, in some cases, the placement of a Greenfield filter is extremely successful.
Compression ultrasonography as a method for diagnosing lower extremity DVT is proven to be equally sensitive and specific compared to other methods that use radiation or contrast agents. Conventional lower extremity Doppler studies, which evaluate the blood vessels in the entire limb, are done by ultrasound technicians and reported by radiologists. Still, these processes can take as long as two hours and slow diagnosis and treatment.
Patients with risk factors for DVT or PE should receive a diagnostic workup, which frequently involves using bedside compression ultrasound. Although contrast venography is the gold standard for DVT diagnosis, point of care ultrasound (POCUS) is being used in more EDs for lower extremity DVT assessment. Two main POCUS techniques are employed: the 2-point method, based on the compressibility of the common femoral vein (CFV) and popliteal vein (PV), and the 3-point method including the superficial femoral vein (SFV).
Current EDs preferentially employ a variation to the 2-point compression technique that targets high-risk regions for DVT, takes less than five minutes, and has comparable diagnostic sensitivity and specificity. A negative DVT compression ultrasound can help avoid the use of anticoagulant agents in patients suspected of having DVT. The 2-point compression method has been used in many studies and is widely accepted when used with pretest probability assessments.
Leg Pain: Cramp or burning pain in one leg which may be constant or develop suddenly; this would be due to obstruction of blood flow in deep veins.
Tenderness: Leg tenderness and discomfort on pressure, especially on the calf, may indicate venous thrombus formation.
Swelling: One of the main symptoms of DVT is the swelling or edema of one leg that may occur due to the clot blocking blood flow.
Erythema: Swelling of the leg may be accompanied by redness or warmth due to inflammation that is associated with a blood clot.
Positive Homans’ Sign: The presence of tenderness on compression of the calf or dorsiflexion of the foot during physical examination may indicate DVT though it is non-specific.
Evidence Supporting POCUS for Lower Extremity DVT
Sensitivity and Specificity
Various investigations by the experts have over the years shown that POCUS by physicians in the emergency department is very effective in diagnosing DVT. In a 1997 study, Jolly et al. showed 100% sensitivity for the duplex ultrasound in trained emergency physicians but this involved complete duplex exams and not the 2- or 3-point technique. Blaivas et al. (2000) applied a 2-point compression ultrasound which correlated with 98% of vascular lab studies. Other authors have published sensitivities of 100% and high specificities, for example, Magazzini et al. results and Jang et al. ’s results on POCUS conducted by emergency physicians and residents.
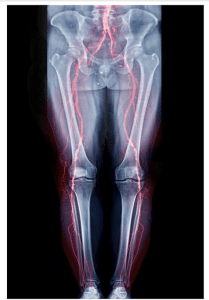
Lower Extremity DVT
In the HOCUS-POCUS study it concluded that using 3-point POCUS assesses by hospitalists, it achieved a sensitivity level of 100% and specificity of 95.8% after brief training. However, Caronia et al reviewed the data and pointed out that the 2-point technique employed by internal medicine residents failed to detect the isolated femoral clots.
In a meta-analysis performed by Lee et al., the authors determined that both 2-point and 3-point POCUS were equally effective, in terms of sensitivity and specificity for DVT diagnosis. In conclusion, POCUS has been shown to be highly accurate in diagnosing proximal DVT based on the existing evidence while acknowledging that accuracy can be reduced by variability in clinical context and clinician experience.
Portable Ultrasound Machine: A portable, mostly in the form of a small unit that is easily carried and is laid on a bedside table. It also offers real-time imaging, making it useful in different specialties, including the emergency department, ICU or outpatient services.
High-Frequency Linear Probe (7-15 MHz): This probe is most suitable for delineation of superficial structures such as veins in the lower limbs. The high frequency is used to good effect here because it gives better definition of the venous system and clot identification in vessels such as the common femoral and popliteal veins are easier.
Ultrasound Gel: Used on the skin to improve the contact between the transducer of the equipment and the body’s surface to enhance the quality of the image as well as reception of the sound waves emitted by the equipment.
Screen or Display: It is attached to the ultrasound machine where it shows the real time picture of the images transmitted by the probe. Some of the modern POCUS devices may have features such as high-resolution touch screens to enhance usability.
Doppler Function: Some machines are Doppler optional to measure blood flow inside the veins which will help to determine the absence or presence of flow that may be suggestive of DVT.
The patient needs to be laid on their back with the leg to be examined pulled up to the level of the inguinal ligament for a bedside ultrasound to determine deep vein thrombosis (DVT). There are two main positions of the patient during the exam: depending on the area that is being tested; however, the position may be adjusted to the patient’s comfort and ability. Ideally, positioning the patient with the head end of the bed raised to at least 30-40 degrees (reverse Trendelenburg) aids in increasing venous distention.
Femoral vein examination: The patient should be supine, and the hip flexed and externally rotated.
Popliteal vein examination: One must expose the back of the knee that is known as popliteal fossa. Either the patient can hang the leg over the side of the bed or, the patient can flex the knee and externally rotate the hip. Instead, they shall move sideways toward their side or extend flat onto the face (supine or prone) if required.

Patient positioning Point-of Care Ultrasound of Lower Extremity DVT
Step 1-Position the Patient: Patient should be lying in a supine position with the hip flexed. The examination will be proceeded by evaluating the common femoral vein, which is situated just inferior to the inguinal ligament.
Step 2-Locate the Common Femoral Vein: Start with the inspection of the common femoral vein which is located right below the inguinal ligament. The femoral vessels are situated halfway between the pubic symphysis and the anterior superior iliac spine. The femoral artery that is usually felt to be pulsating can be used to determine the point of commencement.
Step 3-Prepare the Ultrasound Machine: Make sure that the application of the ultrasound gel to the transducer, and/or the patient’s leg is sufficient for good contact and image quality.
Step 4-Position the Transducer: Position the transducer in a transverse position inferior to the inguinal ligament with the probe marker pointing to the patient’s right side.
Step 5-Visualize the Vein Junction: Sweep the transducer in the cephalad or caudad direction to identify the junction of the common femoral vein and the greater saphenous vein. The common femoral artery will be located lateral to the common femoral vein.
Step 6-Apply Compression: Ensure the amount of pressure exerted by the transducer on the vein is firm and constant while compressing the vein. Lack of compression of the vein means that there is no DVT at this site in this case. Also, make sure that you exert enough pressure that will cause a slight deformation to the artery though.
Step 7-Confirm Compression: If the vein does not fully compress, there is a likelihood that a DVT is present in the leg. The ability to compress the vein fully excludes DVT, while if one can only partially compress the vein, then it is evident that a clot has formed. For DVT to be ruled in or out using ultrasound, compressibility is the most important criterion to consider.
Step 8-Examine the Veins: It is essential to double check whether there exists any compression in the femoral veins as well as the popliteal vein. Rotate the transducer as required to obtain adequate vein compression. It may be important to pay attention to the greater saphenous vein as some clot form at this section of the vein superficial and migrate to the common femoral vein. Evaluate this vein from 2cm proximal to 2 cm distal to this region.
Step 9-Proceed to the Popliteal Vein: If you have confirmed the absence of both deep and the superficial femoral vein, then proceed to check the popliteal vein.

Point-of Care Ultrasound of Lower Extremity DVT
Step 1-Position the Patient: Align the patient on the back when assessing the popliteal vessels.
Step 2-Prepare the Transducer: The ultrasound gel should be used on the transducer’s surface, the leg of the patient, or both to minimize air cavities.
Step 3-Position the Transducer: Position the transducer in the transverse plane of the popliteal fossa with the indicator facing the right side of the patient.
Step 4-Visualize the Vessels: To do this, the transducer is moved either cephalad (toward the head) or caudal (toward the feet) to locate the superficial popliteal artery and vein. The popliteal vein is commonly located posterior the popliteal artery, as its name implies, in the popliteal fossa. Because the posterior lobe of the probe shaft directs the ultrasonic beam towards the machine, the vein may look closer to the transducer compared to the artery.
Step 5-Adjust Probe Pressure: Alleviate the probe pressure if possible for better view of the veins as they are most compressible compared to the artery.
Step 6-Examine the Popliteal Vein: Make sure the examination area involves the distal 2 cm of the popliteal vein as well as proximal sections involving trifurcation of popliteal vein into the anterior tibial, the posterior tibial and the peroneal veins.
Step 7-Note Anatomical Variations: Know that the popliteal vein may bifurcate into the anterior and posterior tibial veins with the peroneal vein emerging from the posterior tibial vein.
Interestingly, Doppler ultrasonography is not a formal component of the focused lower-extremity compression examination for DVT; nonetheless, it is useful for visualization of the regional anatomy and assessment of ambiguous findings. However, Doppler ultrasound results cannot be relied on as a definitive sign of a clot.
Doppler ultrasound tests the velocity, direction, and turbulence of blood flow. Blood flow in both venous and arterial vessels possess distinctive features. In normal venous structures, there should be continuous venous flow that peaks on the compression of the calf, and venous flow should be affected by the respiratory movements, and this generally increases at the time of expiration. Compression of the calves helps to check obstruction distal to the probe while any respiratory changes can point to proximal obstruction in the iliac veins or the inferior vena cava.
In a focused compression ultrasound exam for DVT, a fully compressible vein rules out the diagnosis of DVT and an incompletely compressible vein suggests the presence of DVT. It is vital to denote the location of the clot and more specifically, the area nearest to the clot to assess its advancement or withdrawal after treatment.
This means that while visualization of a clot and Doppler flow can give an indication that DVT may exist and require further follow up scans if clinically warranted, these alone are not sufficient for diagnosis of DVT.
There are no major risks or complications with the utilization of bedside ultrasound for diagnosing DVT. In this concern, there is no adequate literature that tries to advance any theory that clot propagation is instigated by manipulation of legs or compression of the vessels when performing the procedure.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



