Introduction
The use of opioids in the management of chronic pain has become a double-edged weapon in modern medicine. Opioid provides significant relief for patients who have diseases like cancer, neuropathy, or post-surgical pain. The increasing rate of opioid misuse, overdose, or dependence has made the prescription of opioids a risky decision. Clinicians are under pressure to find effective pain relief with proper opioid management.
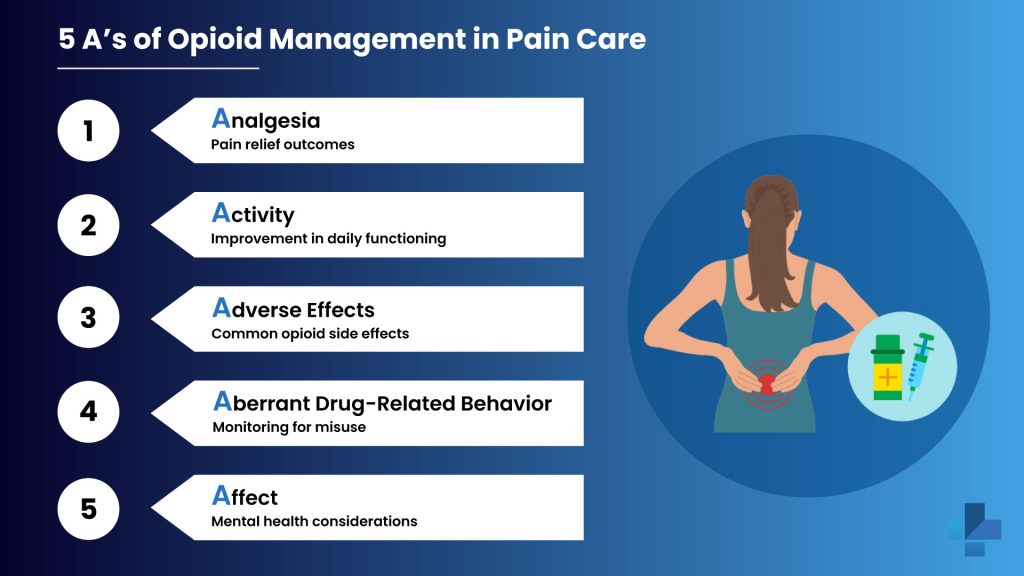
The 5 A’s framework is invaluable. It gives a structured, evidence-based method to monitor and manage opioid treatment. Healthcare providers can decrease the risks and maximize the results by assessing Analgesia, Activity, Adverse effects, Aberrant behavior, and Affect.
Learn more and remain up to date on safe prescribing practices by taking advantage of the free CME-accredited courses at medtigo Certificate Courses.
Why Structured Opioid Monitoring Is Essential?
For pain management, there is an urgent need for disciplined methods because of the opioid crisis. About half a million individuals from 1999 to 2020 in the United States died from fatal overdoses due to the overuse of opioids. Lack of systematic monitoring and early detection of opioid misuse cases was a factor in several cases that resulted in tragedy.
A structured framework like the 5 A’s can help clinicians go beyond just asking questions like “Is your pain better”? It gives a holistic view of the experience of patients in identifying the red flags early. Using this methodology for ongoing assessment can make sure that the advantages of opioids exceed the disadvantages and allow for prompt adjustment in treatment.
Real-world application of the 5 A’s has benefited practices to reduce overdose incidents, detect early signs of addiction, and provide better support to patients who need and get the benefit from opioid treatment.
Deep Dive into the 5 A’s of Opioid Management
A. Analgesia
The effectiveness of opioid treatment is to decrease pain. Effective pain control is not about the elimination of pain; it is about substantial reduction.
Tools like the Brief Pain Inventory (BPI) and the Numeric Rating Scale (NRS) help to quantify the changes in pain over time. For example, a patient who is recovering from spinal surgery reports a drop from /10 to 4/10 on the pain scale and can walk short distances without assistance, which indicates a clinically significant analgesia.
Lack of improvement may indicate tolerance or opioid inefficacy, which needs a reconsideration of the treatment plan.
B. Activity
Pain management needs to improve daily functioning. This involves elevated mobility, return to work, improved sleep, and high social engagement. For example, a 55-year-old individual with degenerative disc disease, after the initiation of an opioid, can clean, cook, and even drive for short distances. These were the activities she had not performed in months. This functional gain is a significant indicator that treatment is beneficial for her quality of life.
Clinical professionals can assess the improvements by using Patient-Specific Functional Scales or by simple goal tracking.
C. Adverse Effects
Opioid side effects are common. The most common side effects are constipation, nausea, dizziness, and sedation. These can severely affect overall health if ignored.
A patient with long-term oxycodone may have severe constipation and appetite loss. Complications can be prevented with anticipatory advice, such as prescribing laxatives with opioids. Regular checkups can allow clinicians to adjust the dosage or change the medications to reduce side effects.
Recording these adverse effects ensures open communication and helps with supportive care.
D. Aberrant Drug-Related Behavior
Aberrant behaviors which indicate abuse, like frequent early refill requests, lost prescriptions, increasing dosages without approval, or doctor shopping. For example, a patient who continuously gets out of medications with a week’s early visit and requests emergency refills must be evaluated through assessment. Tools like PDMP (Prescription Drug Monitoring Programs), urine drug screening, and pill counts are important to identify any risky behaviors.
Early detection of these patterns can help clinicians to take proper actions, which may change the pain management treatment or redirect them to an addiction treatment plan.
E. Affect
Mental health and chronic pain are closely linked. Untreated depression, anxiety, PTSD, and emotional distress can increase pain and affect treatment results.
For example, a patient who has chronic migraine reported increasing pain and opioid dependence. After additional testing, she was diagnosed with major depressive disorder. Managing her depression with psychotherapy and SSRIs significantly enhanced her pain control and reduced opioid usage.
A comprehensive method to pain management must involve open-ended communication about emotional well-being and mental health screening.
Incorporating the 5 A’s Into Routine Care
Practices can involve the 5 A’s in routine clinical workflows. This can develop EMR-integrated templates, smart phrases, or structured note formats that prompt healthcare providers to review each A at every visit.
For example, an EMR may include dropdown menus for pain score (Analgesia), activity level (Activity), side effects checklist (Adverse Effects), PDMP status (Aberrant behavior), and mood screening (Affect).
A team-based method includes nurses, pharmacists, behavioral health providers, and case managers to ensure comprehensive treatment. This shared responsibility decreases the provider burden and increases patient outcomes.
Education & CME for Safer Opioid Prescribing
medtigo’s pain management courses offer:
- 3 CME credits
- 100% free access
- Flexible online learning
- Real-life case studies
These courses can improve healthcare providers’ judgment, detect red flags early, and deliver safe and patient-centered opioid care.
Start learning today → medtigo Certificate Courses
Conclusion
The 5 A’s of opioid monitoring: Analgesia, Activity, Adverse effects, Aberrant behavior, and Affect can give a structured, compassionate, and clinical method to manage opioid treatment. This method increases patient safety, outcomes, and builds trust in patients and providers.
Want to remain updated on the best practices in opioid management? Explore our CME-accredited online courses for healthcare professionals.
FAQs About Opioid Management and the 5 A’s Framework
Q1. Why is it important to monitor structured opioids?
Structured monitoring of opioids by using tools like the 5 A’s makes sure to provide safe, more effective, and compassionate care for patients who have chronic pain, with increasing misuse of opioids.
Q2. How can I monitor the patients for aberrant drug-related behavior?
Providers can use methods like pill counts, PDMP checks, urine screens, and monitoring early refill requests to determine the potential misuse of opioids.
Q3. Can mental health affect opioid treatment outcomes?
Yes, mental health (anxiety and depression) can affect the pain perception and treatment response. This component encourages clinicians to consider the mental well-being in pain management.
Q4. Are there any free CME courses available on opioid management?
Yes, medtigo offers free and CME-accredited pain management courses to help healthcare providers stay updated on best practices in opioid prescribing and monitoring.