CYP2D6-Guided Opioid Prescribing Fails to Improve Postoperative Pain in ADOPT PGx Randomized Trial
February 23, 2026
Background
Anemia associated with chemotherapy is a complicated condition in patients undergoing treatment for cancer.
Chemotherapy drugs attack on fast-growing cells including cancer and healthy bone marrow cells.
Less red blood cells or hemoglobin count reduces oxygen-carrying capacity of blood to cause anemia.
Chemotherapy can affect kidney function to reduce the production of erythropoietin. The inflammatory response to cancer and its treatment can increase levels of cytokines.
Patients with chemotherapy-associated anemia may experience symptoms as:
Fatigue and weakness
Shortness of breath
Pale skin
Rapid heartbeat
Epidemiology
Anemia is prevalent in cancer patients with 30% to 90% cases depends on cancer type and chemotherapy treatment.
Chemotherapy-induced anemia is common in patients with hematologic malignancies and solid tumors.
Chemotherapy treatment increases anemia risk from bone marrow suppression. Cancer patients experience anemia due to inflammation and infections.
Anatomy
Pathophysiology
Chemotherapy affects stromal cells and extracellular matrix to damage the microenvironment of bone marrow.
Cytokines decrease red blood cell production to inhibit progenitor cell growth.
Chemotherapy enhances reactive oxygen species production that cause oxidative damage to RBCs.
Tumors and chemotherapy may cause chronic blood loss and affect required vitamin absorption for DNA synthesis and RBC production.
Etiology
Genetics
Prognostic Factors
Elderly patients are at higher risk for severe anemia due to various factors.
Poor nutrition and deficiencies in iron, vitamin B12, and folate damages anemia condition to affect recovery.
Blood cancers in bone marrow increase risk of severe anemia.
Advanced cancer equals higher tumor burden, inflammation, marrow suppression, severe anemia risks.
Chemotherapy with myelosuppressive agents increases risk of anemia.
Clinical History
It includes information about demography, medical history, family history, and presenting symptoms of patient.
Physical Examination
Age group
Associated comorbidity
Associated activity
Acuity of presentation
Acute symptoms as:
Chronic symptoms as:
Differential Diagnoses
Laboratory Studies
Imaging Studies
Procedures
Histologic Findings
Staging
Treatment Paradigm
Use Erythropoiesis-Stimulating Agents in patients with chemotherapy-induced anemia those with chronic kidney disease or cancer-related anemia.
Nutritional support and supplementation should be given in form of iron supplementation through various route.
Management of chemotherapy to reduce dose intensity or frequency of myelosuppressive agents.
Management of chronic diseases is conducted to optimize renal function and consider erythropoietin therapy.
Red blood cell transfusions method is used to manage symptomatic anemia.
Platelet transfusions are indicated to prevent bleeding in thrombocytopenia cases.
by Stage
by Modality
Chemotherapy
Radiation Therapy
Surgical Interventions
Hormone Therapy
Immunotherapy
Hyperthermia
Photodynamic Therapy
Stem Cell Transplant
Targeted Therapy
Palliative Care
use-of-non-pharmacological-approach-for-anemia-associated-with-chemotherapy
Ensure safe environment to prevent falls and accidents in patients with weakness or dizziness.
Balanced diet includes iron, B12, and folate supplementation to maintain adequate nutrition level.
Use HEPA filters to reduce airborne particles and lower infection risk efficiently.
Maintain ventilation in patient rooms for air quality control. Prepare food properly to prevent foodborne infections.
Proper awareness about anemia associated chemotherapy should be provided and its related causes with management strategies.
Appointments with an oncologist and preventing recurrence of disorder is an ongoing life-long effort.
Use of Erythropoiesis-Stimulating Agent
Epoetin:
It is hormonal drug that stimulates red blood cell production.
Use of iron supplementation
Ferric carboxymaltose:
It is iron hydroxide in a complex with carboxymaltose that releases iron to transport oxygen.
use-of-intervention-with-a-procedure-in-treating-anemia-associated-with-chemotherapy
Blood transfusions method indicated to increase hemoglobin levels and severe symptoms of anemia.
Bone marrow biopsy was performed to evaluate bone marrow function and eliminate bone marrow infiltration.
use-of-phases-in-anemia-associated-with-chemotherapy
In the initial assessment phase, evaluation of patient history, physical examination, and laboratory test to confirm diagnosis.
Pharmacologic therapy is effective in the treatment phase as it includes use of Erythropoiesis-Stimulating Agents and iron supplementation.
In supportive care and management phase, patients should receive required attention such as lifestyle modification and intervention therapies.
The regular follow-up visits with the oncologist are scheduled to check the improvement of patients along with treatment response.
Medication
Initial dose:2.25mcg/kg intravenous/ subcutaneous once every week
Procrit, Epogen, Retacrit
Treatment of anemic patients with non-myeloid malignancies where anemia is caused by concomitant myelosuppressive chemotherapy, and there is a minimum of 2 months of planned treatment after beginning
Initially, 150 units/kg intravenous/subcutaneous three times per week; alternatively, 40,000 units subcutaneously once per week until the chemotherapy course is finished
Reduce the dose by 25%
Hgb levels rise by more than 1 g/dL in any two-week period
Hgb meets the required level to avoid RBC transfusion
Withhold dose if hemoglobin exceeds the level required to avoid RBC transfusion; restart at a 25% lower dose if hemoglobin approaches the level where RBC transfusions may be required
Dose increase
If Hgb increases by less than 1 g/dL after 4 weeks of therapy but continues at below 10 g/dL, it may increase the dose to 60,000 units weekly or 300 units/kg 3 times a week
If no response is obtained after 8 weeks, or if RBC transfusions are required, the dose should be discontinued
Reducing Allogeneic Red Blood Cell Transfusions in Patients Undergoing Noncardiac, Nonvascular Surgery
Procrit, Epogen, Retacrit
Indicated to decrease the need for allogeneic RBC transfusions in patients with perioperative hemoglobin greater than 10 g/dL but less than 13 g/dL who are at high risk of perioperative blood loss from noncardiac, nonvascular surgery.
For 15 days, take 300 units/kg subcutaneously once a day
Alternatively, 600 units/kg Subcutaneous in 4 doses given 21, 14, and 7 days before surgery, as well as on the day of surgery
Concurrent deep vein thrombosis (DVT) prevention is recommended
Procrit, Epogen, Retacrit
Treatment of anaemic patients with non-myeloid malignancies where anemia is caused by concomitant myelosuppressive chemotherapy, and there is a minimum of 2 months of planned treatment after beginning
Below five years: Safety and efficacy were not established
5-18 years: 600 units/kg Intravenous once weekly; should not exceed 40,000 units
Reduce the dose by 25%.
Hgb levels rise by more than 1 g/dL in any two-week period
Hgb meets the required level to avoid RBC transfusion
Withhold dose if hemoglobin exceeds the level required to avoid RBC transfusion; restart at a 25% lower dose if haemoglobin approaches the level where RBC transfusions may be required
Dose increase
If Hgb increases by less than 1 g/dL after four weeks of therapy but continues at below 10 g/dL, it may increase the dose to 60,000 units weekly or 300 units/kg 3 times per week
If no response is obtained after 8 weeks, or if RBC transfusions are required, the dose should be discontinued
Future Trends
Anemia associated with chemotherapy is a complicated condition in patients undergoing treatment for cancer.
Chemotherapy drugs attack on fast-growing cells including cancer and healthy bone marrow cells.
Less red blood cells or hemoglobin count reduces oxygen-carrying capacity of blood to cause anemia.
Chemotherapy can affect kidney function to reduce the production of erythropoietin. The inflammatory response to cancer and its treatment can increase levels of cytokines.
Patients with chemotherapy-associated anemia may experience symptoms as:
Fatigue and weakness
Shortness of breath
Pale skin
Rapid heartbeat
Anemia is prevalent in cancer patients with 30% to 90% cases depends on cancer type and chemotherapy treatment.
Chemotherapy-induced anemia is common in patients with hematologic malignancies and solid tumors.
Chemotherapy treatment increases anemia risk from bone marrow suppression. Cancer patients experience anemia due to inflammation and infections.
Chemotherapy affects stromal cells and extracellular matrix to damage the microenvironment of bone marrow.
Cytokines decrease red blood cell production to inhibit progenitor cell growth.
Chemotherapy enhances reactive oxygen species production that cause oxidative damage to RBCs.
Tumors and chemotherapy may cause chronic blood loss and affect required vitamin absorption for DNA synthesis and RBC production.
Elderly patients are at higher risk for severe anemia due to various factors.
Poor nutrition and deficiencies in iron, vitamin B12, and folate damages anemia condition to affect recovery.
Blood cancers in bone marrow increase risk of severe anemia.
Advanced cancer equals higher tumor burden, inflammation, marrow suppression, severe anemia risks.
Chemotherapy with myelosuppressive agents increases risk of anemia.
It includes information about demography, medical history, family history, and presenting symptoms of patient.
Acute symptoms as:
Chronic symptoms as:
Use Erythropoiesis-Stimulating Agents in patients with chemotherapy-induced anemia those with chronic kidney disease or cancer-related anemia.
Nutritional support and supplementation should be given in form of iron supplementation through various route.
Management of chemotherapy to reduce dose intensity or frequency of myelosuppressive agents.
Management of chronic diseases is conducted to optimize renal function and consider erythropoietin therapy.
Red blood cell transfusions method is used to manage symptomatic anemia.
Platelet transfusions are indicated to prevent bleeding in thrombocytopenia cases.
Oncology, Radiation
Ensure safe environment to prevent falls and accidents in patients with weakness or dizziness.
Balanced diet includes iron, B12, and folate supplementation to maintain adequate nutrition level.
Use HEPA filters to reduce airborne particles and lower infection risk efficiently.
Maintain ventilation in patient rooms for air quality control. Prepare food properly to prevent foodborne infections.
Proper awareness about anemia associated chemotherapy should be provided and its related causes with management strategies.
Appointments with an oncologist and preventing recurrence of disorder is an ongoing life-long effort.
Oncology, Radiation
Epoetin:
It is hormonal drug that stimulates red blood cell production.
Oncology, Radiation
Ferric carboxymaltose:
It is iron hydroxide in a complex with carboxymaltose that releases iron to transport oxygen.
Oncology, Radiation
Blood transfusions method indicated to increase hemoglobin levels and severe symptoms of anemia.
Bone marrow biopsy was performed to evaluate bone marrow function and eliminate bone marrow infiltration.
Oncology, Radiation
In the initial assessment phase, evaluation of patient history, physical examination, and laboratory test to confirm diagnosis.
Pharmacologic therapy is effective in the treatment phase as it includes use of Erythropoiesis-Stimulating Agents and iron supplementation.
In supportive care and management phase, patients should receive required attention such as lifestyle modification and intervention therapies.
The regular follow-up visits with the oncologist are scheduled to check the improvement of patients along with treatment response.
Anemia associated with chemotherapy is a complicated condition in patients undergoing treatment for cancer.
Chemotherapy drugs attack on fast-growing cells including cancer and healthy bone marrow cells.
Less red blood cells or hemoglobin count reduces oxygen-carrying capacity of blood to cause anemia.
Chemotherapy can affect kidney function to reduce the production of erythropoietin. The inflammatory response to cancer and its treatment can increase levels of cytokines.
Patients with chemotherapy-associated anemia may experience symptoms as:
Fatigue and weakness
Shortness of breath
Pale skin
Rapid heartbeat
Anemia is prevalent in cancer patients with 30% to 90% cases depends on cancer type and chemotherapy treatment.
Chemotherapy-induced anemia is common in patients with hematologic malignancies and solid tumors.
Chemotherapy treatment increases anemia risk from bone marrow suppression. Cancer patients experience anemia due to inflammation and infections.
Chemotherapy affects stromal cells and extracellular matrix to damage the microenvironment of bone marrow.
Cytokines decrease red blood cell production to inhibit progenitor cell growth.
Chemotherapy enhances reactive oxygen species production that cause oxidative damage to RBCs.
Tumors and chemotherapy may cause chronic blood loss and affect required vitamin absorption for DNA synthesis and RBC production.
Elderly patients are at higher risk for severe anemia due to various factors.
Poor nutrition and deficiencies in iron, vitamin B12, and folate damages anemia condition to affect recovery.
Blood cancers in bone marrow increase risk of severe anemia.
Advanced cancer equals higher tumor burden, inflammation, marrow suppression, severe anemia risks.
Chemotherapy with myelosuppressive agents increases risk of anemia.
It includes information about demography, medical history, family history, and presenting symptoms of patient.
Acute symptoms as:
Chronic symptoms as:
Use Erythropoiesis-Stimulating Agents in patients with chemotherapy-induced anemia those with chronic kidney disease or cancer-related anemia.
Nutritional support and supplementation should be given in form of iron supplementation through various route.
Management of chemotherapy to reduce dose intensity or frequency of myelosuppressive agents.
Management of chronic diseases is conducted to optimize renal function and consider erythropoietin therapy.
Red blood cell transfusions method is used to manage symptomatic anemia.
Platelet transfusions are indicated to prevent bleeding in thrombocytopenia cases.
Oncology, Radiation
Ensure safe environment to prevent falls and accidents in patients with weakness or dizziness.
Balanced diet includes iron, B12, and folate supplementation to maintain adequate nutrition level.
Use HEPA filters to reduce airborne particles and lower infection risk efficiently.
Maintain ventilation in patient rooms for air quality control. Prepare food properly to prevent foodborne infections.
Proper awareness about anemia associated chemotherapy should be provided and its related causes with management strategies.
Appointments with an oncologist and preventing recurrence of disorder is an ongoing life-long effort.
Oncology, Radiation
Epoetin:
It is hormonal drug that stimulates red blood cell production.
Oncology, Radiation
Ferric carboxymaltose:
It is iron hydroxide in a complex with carboxymaltose that releases iron to transport oxygen.
Oncology, Radiation
Blood transfusions method indicated to increase hemoglobin levels and severe symptoms of anemia.
Bone marrow biopsy was performed to evaluate bone marrow function and eliminate bone marrow infiltration.
Oncology, Radiation
In the initial assessment phase, evaluation of patient history, physical examination, and laboratory test to confirm diagnosis.
Pharmacologic therapy is effective in the treatment phase as it includes use of Erythropoiesis-Stimulating Agents and iron supplementation.
In supportive care and management phase, patients should receive required attention such as lifestyle modification and intervention therapies.
The regular follow-up visits with the oncologist are scheduled to check the improvement of patients along with treatment response.
Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

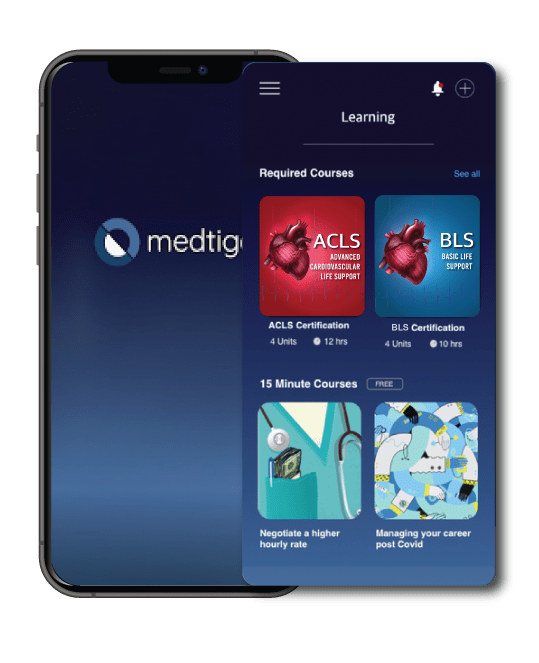
When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.




