Sleepless and Costly: How OSA Is Hitting US and UK Workforces
March 3, 2026
Background
Colorectal surgery is a significant intervention commonly employed in the treatment of various diseases, including colorectal cancer, diverticulitis, inflammatory bowel disease, and other gastrointestinal conditions. Even at this era of diverse types of surgical interventions with adequate post-operative care, infections still top the list among the major complications after colorectal surgery. Contracting any of these infections increases morbidity rates, prolongs hospital stays, and increases, to a large extent, healthcare costs; worst of all, the death rate increases respectively.
Types of Colorectal Infections
Surgical Site Infections (SSIs):
Superficial Incisional SSI: Pertains only to the tissues right down to the skin and the subcutaneous layer at the site of the incision.
Deep Incisional SSI: Works on layers of muscles and connective tissue or fascia, respectively.
Organ/Space SSI: Any organ or space of the body’s anatomy other than the incision site or area that was incised or operated on.
Anastomotic Leaks: These occur after the Surgically created anastomosis between two intestinal segments breaks down, leading to leakage in the intestines’ content into the peritoneal cavity. It follows infection and subsequent sepsis.
Intra-abdominal Abscesses: This involves the collection of pus in the abdomen. It can occur as a sequel to contamination of the cavity during surgery.
Risk Factors
The risk of developing post-operative infection after colorectal surgery is influenced by several factors, including:
Patient-Related Factors: The factors include age, other diseases, such as diabetes and obesity, immunosuppressive status, malnutrition, smoking, and other chronic diseases like cardiac diseases, diabetes, and chronic obstructive airway diseases etc.
Procedure-Related Factors: Perioperative or intravenous glucose administration, length of surgery, nature of the surgery, whether it was an emergency surgery or routine one, and the use of antibiotics for surgical prophylaxis.
Factors related to the Hospital: Preoperative culture, scrupulousness of the surgeon regarding surgical asepsis, and soft tissue handling/ postoperative wound care practices.
Epidemiology
Anatomy
Pathophysiology
Etiology
Genetics
Prognostic Factors
Clinical History
Physical Examination
Age group
Associated comorbidity
Associated activity
Acuity of presentation
Differential Diagnoses
Laboratory Studies
Imaging Studies
Procedures
Histologic Findings
Staging
Treatment Paradigm
by Stage
by Modality
Chemotherapy
Radiation Therapy
Surgical Interventions
Hormone Therapy
Immunotherapy
Hyperthermia
Photodynamic Therapy
Stem Cell Transplant
Targeted Therapy
Palliative Care
postoperative-sepsis-after-colorectal-surgery
Validated findings indicated that postoperative sepsis is a substantial challenge in colorectal surgery. It is a normal response to infection involving the body’s inflammation system. If not appropriately managed or treated in time, it can cause severe sickness or even become fatal.
Causes
Intra-abdominal infections: Anastomotic breakdown of the bowel, formation of an abscess, or peritonitis.
Surgical site infections (SSIs): Infections of the sutured area.
Other infections: Any kind of infections that may include urinary tract infections, pneumonia, or catheter-related bloodstream infections.
Risk Factors
Advanced age: Older patients are more susceptible.
Comorbidities: Diabetes, obesity, immunosuppression, or chronic kidney or liver disease.
Malnutrition: Poor nutritional status.
Prolonged surgery: Which indicates that, the overall operative times poses risk with increase in duration of the operation.
Emergency surgery: They are associated with a higher risk than those procedures that are not vital or necessary for the wellbeing of a patient.
wound-infection-after-colorectal-surgery
Postoperative wound infections are always a significant concern because of the level of risk of contamination having regard to the nature of the surgery which involves the colon rectum. Consequently, it can develop severe outcomes, which in turn prolong the hospital stay and require more treatments.
Causes
Bacterial Contamination: The large bowel is heavily colonized, and any procedure carried out in this area exposes the operation site to bacterial colonization.
Surgical Technique: The mode and accuracy of surgery is one of the significant factors. Finally, it also demonstrated that patients with the poor technique of using the developed system contains more chances for infection.
Type of Surgery: Certain procedures in colorectal surgery are automatically at a higher risk level depending on the nature and area of operation.
Risk Factors
Patient-Related Factors:
Age: Patients of advanced age usually are at a higher risk of getting infected.
Comorbidities: Pathologies such infections diabetes, obesity, immunosuppression the due to medication or HIV enhances the risk disease progression.
Nutritional Status: Protein energy-malnutrition directly influences the healing process.
respiratory-complications-after-colorectal-surgery
Postoperative pulmonary problems are therefore a significant factor of concern in patients who have undergone colorectal surgery. These complexities may include Pneumonia, atelectasis, respiratory failure, and worsened chronic respiratory diseases.
Causes
Anesthesia: General anesthesia mainly affects the respiratory system by depressing the patient’s breathing and can cause hypoventilation, aspiration, and other related complications.
Surgical Trauma: The patient’s muscles and physical wellbeing are shocked during surgery which can in turn affect lung performance and likelihood of adverse effects.
Pain: This is because postoperative pain usually inhibits adequate deep breathing and dry coughing that prevent formation of atelectasis and subsequently pneumonia.
Infection: Surgical site infections can occur and extend to the lung, causing pneumonia.
Prolonged Immobilization: Immobility after surgery exposes the patient to such complications as atelectasis, and pnuemonia due to decreased lung expansion.
Risk Factors
Patient-Related Factors:
Age: Patients over sixty-five are deemed to have higher risks.
Comorbidities: Other comorbidities that have been reported to indicate potential risks include COPD, asthma, heart disease, and diabetes.
Smoking: Patients with lung disease and those who smoke also have higher risks because of poor lung function and the act of mucociliary clearance.
Obesity: Obesity that leads to excessive body weight affects the ability of a patient’s respiratory muscles and the diffusion of gases.
Pre-existing Respiratory Conditions: Some illnesses which aggravate the probability of having complications include bronchitis and emphysema.
Surgery-Related Factors:
Type of Surgery: Surgical interventions that are more complex or that involve the invasion of a body’s integrity have higher risks than others.
Duration of Surgery: Postoperative respiratory complications are also more common in longer surgeries because the patient is on a breathing tube for quite a long time.
Type of Anesthesia: With the administration of general anesthesia, there is a relatively higher risk than regional anesthesia.
Postoperative Care:
Pain Management: Inadequate pain control can prevent effective coughing and deep breathing.
Ventilation Support: The use of mechanical ventilation for a long time raises the rates of ventilator-associated pneumonia.
Medication
1 gm orally every 6 to 8 hours for three doses
1 gm orally every 6 to 8 hours for three doses
Diagnostic imaging for Colorectal disease
CEA-Scan® undergoes reconstitution with a solution of sodium pertechnetate Tc 99m before utilization
The usual adult recommended dose comprises a 1 mg single dose of Arcitumomab labeled with 20 to 30 mCi of Technetium Tc 99m
The dosage is given as a 2 ml intravenous injection after being diluted with 1 ml of Sodium Chloride Injection, USP
Alternatively, the contents of the vial may be diluted with Sodium Chloride isotonic Injection, USP, to a total volume of 30 ml, and the infusion can be given intravenously over a period of 5 to 20 minutes
For best imaging quality, the injection should take place four hours after reconstitution and within five minutes of that time
Before infusion, the sterile, non-pyrogenic, reconstituted mixture can be kept at room temperature without the need for bacteriostatic preservatives
The individual's dose is calculated in a dose calibrator prior to administration
Using immediate thin-layer chromatography, the radiochemical purity is required to be greater than 90% (ITLC)
It is essential to visually inspect for particles or discoloration; if found, dispose of the item right away and notify the manufacturer
It is advised to do immunoscintigraphy utilizing planar and SPECT (Single-Photon Emission Computed Tomography) techniques between two and five hours after injection
Additional views may be obtained up to twenty-four hours later, depending on the results of previous imaging tests
Dose Adjustments
Limited data is available
Future Trends
Colorectal surgery is a significant intervention commonly employed in the treatment of various diseases, including colorectal cancer, diverticulitis, inflammatory bowel disease, and other gastrointestinal conditions. Even at this era of diverse types of surgical interventions with adequate post-operative care, infections still top the list among the major complications after colorectal surgery. Contracting any of these infections increases morbidity rates, prolongs hospital stays, and increases, to a large extent, healthcare costs; worst of all, the death rate increases respectively.
Types of Colorectal Infections
Surgical Site Infections (SSIs):
Superficial Incisional SSI: Pertains only to the tissues right down to the skin and the subcutaneous layer at the site of the incision.
Deep Incisional SSI: Works on layers of muscles and connective tissue or fascia, respectively.
Organ/Space SSI: Any organ or space of the body’s anatomy other than the incision site or area that was incised or operated on.
Anastomotic Leaks: These occur after the Surgically created anastomosis between two intestinal segments breaks down, leading to leakage in the intestines’ content into the peritoneal cavity. It follows infection and subsequent sepsis.
Intra-abdominal Abscesses: This involves the collection of pus in the abdomen. It can occur as a sequel to contamination of the cavity during surgery.
Risk Factors
The risk of developing post-operative infection after colorectal surgery is influenced by several factors, including:
Patient-Related Factors: The factors include age, other diseases, such as diabetes and obesity, immunosuppressive status, malnutrition, smoking, and other chronic diseases like cardiac diseases, diabetes, and chronic obstructive airway diseases etc.
Procedure-Related Factors: Perioperative or intravenous glucose administration, length of surgery, nature of the surgery, whether it was an emergency surgery or routine one, and the use of antibiotics for surgical prophylaxis.
Factors related to the Hospital: Preoperative culture, scrupulousness of the surgeon regarding surgical asepsis, and soft tissue handling/ postoperative wound care practices.
Infectious Disease
Validated findings indicated that postoperative sepsis is a substantial challenge in colorectal surgery. It is a normal response to infection involving the body’s inflammation system. If not appropriately managed or treated in time, it can cause severe sickness or even become fatal.
Causes
Intra-abdominal infections: Anastomotic breakdown of the bowel, formation of an abscess, or peritonitis.
Surgical site infections (SSIs): Infections of the sutured area.
Other infections: Any kind of infections that may include urinary tract infections, pneumonia, or catheter-related bloodstream infections.
Risk Factors
Advanced age: Older patients are more susceptible.
Comorbidities: Diabetes, obesity, immunosuppression, or chronic kidney or liver disease.
Malnutrition: Poor nutritional status.
Prolonged surgery: Which indicates that, the overall operative times poses risk with increase in duration of the operation.
Emergency surgery: They are associated with a higher risk than those procedures that are not vital or necessary for the wellbeing of a patient.
Infectious Disease
Postoperative wound infections are always a significant concern because of the level of risk of contamination having regard to the nature of the surgery which involves the colon rectum. Consequently, it can develop severe outcomes, which in turn prolong the hospital stay and require more treatments.
Causes
Bacterial Contamination: The large bowel is heavily colonized, and any procedure carried out in this area exposes the operation site to bacterial colonization.
Surgical Technique: The mode and accuracy of surgery is one of the significant factors. Finally, it also demonstrated that patients with the poor technique of using the developed system contains more chances for infection.
Type of Surgery: Certain procedures in colorectal surgery are automatically at a higher risk level depending on the nature and area of operation.
Risk Factors
Patient-Related Factors:
Age: Patients of advanced age usually are at a higher risk of getting infected.
Comorbidities: Pathologies such infections diabetes, obesity, immunosuppression the due to medication or HIV enhances the risk disease progression.
Nutritional Status: Protein energy-malnutrition directly influences the healing process.
Postoperative pulmonary problems are therefore a significant factor of concern in patients who have undergone colorectal surgery. These complexities may include Pneumonia, atelectasis, respiratory failure, and worsened chronic respiratory diseases.
Causes
Anesthesia: General anesthesia mainly affects the respiratory system by depressing the patient’s breathing and can cause hypoventilation, aspiration, and other related complications.
Surgical Trauma: The patient’s muscles and physical wellbeing are shocked during surgery which can in turn affect lung performance and likelihood of adverse effects.
Pain: This is because postoperative pain usually inhibits adequate deep breathing and dry coughing that prevent formation of atelectasis and subsequently pneumonia.
Infection: Surgical site infections can occur and extend to the lung, causing pneumonia.
Prolonged Immobilization: Immobility after surgery exposes the patient to such complications as atelectasis, and pnuemonia due to decreased lung expansion.
Risk Factors
Patient-Related Factors:
Age: Patients over sixty-five are deemed to have higher risks.
Comorbidities: Other comorbidities that have been reported to indicate potential risks include COPD, asthma, heart disease, and diabetes.
Smoking: Patients with lung disease and those who smoke also have higher risks because of poor lung function and the act of mucociliary clearance.
Obesity: Obesity that leads to excessive body weight affects the ability of a patient’s respiratory muscles and the diffusion of gases.
Pre-existing Respiratory Conditions: Some illnesses which aggravate the probability of having complications include bronchitis and emphysema.
Surgery-Related Factors:
Type of Surgery: Surgical interventions that are more complex or that involve the invasion of a body’s integrity have higher risks than others.
Duration of Surgery: Postoperative respiratory complications are also more common in longer surgeries because the patient is on a breathing tube for quite a long time.
Type of Anesthesia: With the administration of general anesthesia, there is a relatively higher risk than regional anesthesia.
Postoperative Care:
Pain Management: Inadequate pain control can prevent effective coughing and deep breathing.
Ventilation Support: The use of mechanical ventilation for a long time raises the rates of ventilator-associated pneumonia.
Colorectal surgery is a significant intervention commonly employed in the treatment of various diseases, including colorectal cancer, diverticulitis, inflammatory bowel disease, and other gastrointestinal conditions. Even at this era of diverse types of surgical interventions with adequate post-operative care, infections still top the list among the major complications after colorectal surgery. Contracting any of these infections increases morbidity rates, prolongs hospital stays, and increases, to a large extent, healthcare costs; worst of all, the death rate increases respectively.
Types of Colorectal Infections
Surgical Site Infections (SSIs):
Superficial Incisional SSI: Pertains only to the tissues right down to the skin and the subcutaneous layer at the site of the incision.
Deep Incisional SSI: Works on layers of muscles and connective tissue or fascia, respectively.
Organ/Space SSI: Any organ or space of the body’s anatomy other than the incision site or area that was incised or operated on.
Anastomotic Leaks: These occur after the Surgically created anastomosis between two intestinal segments breaks down, leading to leakage in the intestines’ content into the peritoneal cavity. It follows infection and subsequent sepsis.
Intra-abdominal Abscesses: This involves the collection of pus in the abdomen. It can occur as a sequel to contamination of the cavity during surgery.
Risk Factors
The risk of developing post-operative infection after colorectal surgery is influenced by several factors, including:
Patient-Related Factors: The factors include age, other diseases, such as diabetes and obesity, immunosuppressive status, malnutrition, smoking, and other chronic diseases like cardiac diseases, diabetes, and chronic obstructive airway diseases etc.
Procedure-Related Factors: Perioperative or intravenous glucose administration, length of surgery, nature of the surgery, whether it was an emergency surgery or routine one, and the use of antibiotics for surgical prophylaxis.
Factors related to the Hospital: Preoperative culture, scrupulousness of the surgeon regarding surgical asepsis, and soft tissue handling/ postoperative wound care practices.
Infectious Disease
Validated findings indicated that postoperative sepsis is a substantial challenge in colorectal surgery. It is a normal response to infection involving the body’s inflammation system. If not appropriately managed or treated in time, it can cause severe sickness or even become fatal.
Causes
Intra-abdominal infections: Anastomotic breakdown of the bowel, formation of an abscess, or peritonitis.
Surgical site infections (SSIs): Infections of the sutured area.
Other infections: Any kind of infections that may include urinary tract infections, pneumonia, or catheter-related bloodstream infections.
Risk Factors
Advanced age: Older patients are more susceptible.
Comorbidities: Diabetes, obesity, immunosuppression, or chronic kidney or liver disease.
Malnutrition: Poor nutritional status.
Prolonged surgery: Which indicates that, the overall operative times poses risk with increase in duration of the operation.
Emergency surgery: They are associated with a higher risk than those procedures that are not vital or necessary for the wellbeing of a patient.
Infectious Disease
Postoperative wound infections are always a significant concern because of the level of risk of contamination having regard to the nature of the surgery which involves the colon rectum. Consequently, it can develop severe outcomes, which in turn prolong the hospital stay and require more treatments.
Causes
Bacterial Contamination: The large bowel is heavily colonized, and any procedure carried out in this area exposes the operation site to bacterial colonization.
Surgical Technique: The mode and accuracy of surgery is one of the significant factors. Finally, it also demonstrated that patients with the poor technique of using the developed system contains more chances for infection.
Type of Surgery: Certain procedures in colorectal surgery are automatically at a higher risk level depending on the nature and area of operation.
Risk Factors
Patient-Related Factors:
Age: Patients of advanced age usually are at a higher risk of getting infected.
Comorbidities: Pathologies such infections diabetes, obesity, immunosuppression the due to medication or HIV enhances the risk disease progression.
Nutritional Status: Protein energy-malnutrition directly influences the healing process.
Postoperative pulmonary problems are therefore a significant factor of concern in patients who have undergone colorectal surgery. These complexities may include Pneumonia, atelectasis, respiratory failure, and worsened chronic respiratory diseases.
Causes
Anesthesia: General anesthesia mainly affects the respiratory system by depressing the patient’s breathing and can cause hypoventilation, aspiration, and other related complications.
Surgical Trauma: The patient’s muscles and physical wellbeing are shocked during surgery which can in turn affect lung performance and likelihood of adverse effects.
Pain: This is because postoperative pain usually inhibits adequate deep breathing and dry coughing that prevent formation of atelectasis and subsequently pneumonia.
Infection: Surgical site infections can occur and extend to the lung, causing pneumonia.
Prolonged Immobilization: Immobility after surgery exposes the patient to such complications as atelectasis, and pnuemonia due to decreased lung expansion.
Risk Factors
Patient-Related Factors:
Age: Patients over sixty-five are deemed to have higher risks.
Comorbidities: Other comorbidities that have been reported to indicate potential risks include COPD, asthma, heart disease, and diabetes.
Smoking: Patients with lung disease and those who smoke also have higher risks because of poor lung function and the act of mucociliary clearance.
Obesity: Obesity that leads to excessive body weight affects the ability of a patient’s respiratory muscles and the diffusion of gases.
Pre-existing Respiratory Conditions: Some illnesses which aggravate the probability of having complications include bronchitis and emphysema.
Surgery-Related Factors:
Type of Surgery: Surgical interventions that are more complex or that involve the invasion of a body’s integrity have higher risks than others.
Duration of Surgery: Postoperative respiratory complications are also more common in longer surgeries because the patient is on a breathing tube for quite a long time.
Type of Anesthesia: With the administration of general anesthesia, there is a relatively higher risk than regional anesthesia.
Postoperative Care:
Pain Management: Inadequate pain control can prevent effective coughing and deep breathing.
Ventilation Support: The use of mechanical ventilation for a long time raises the rates of ventilator-associated pneumonia.
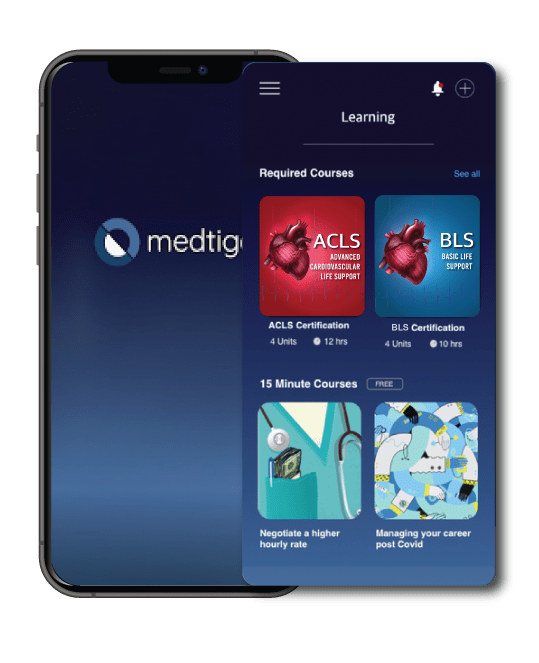
Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.
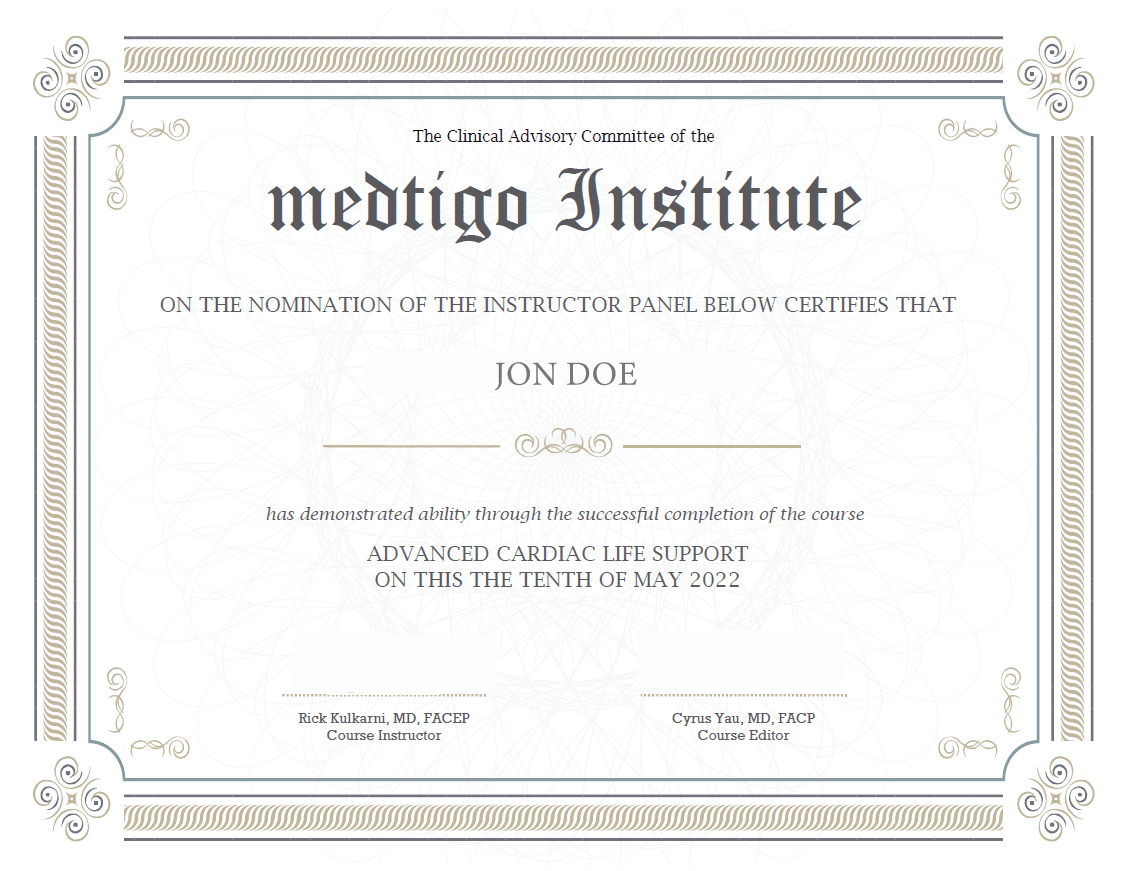
On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.
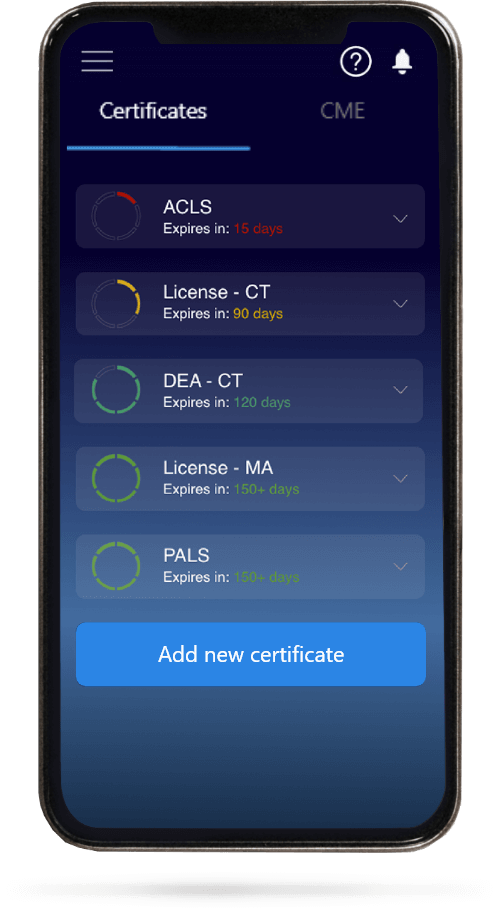
When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.