Ostarine: The ‘Invisible’ Doping Threat Trapping Innocent Athletes
February 18, 2026
Background
Dermatitis artefacta, also known as factitious dermatitis or self-inflicted dermatosis, is a psychological condition in which individuals intentionally create or exaggerate skin lesions or symptoms to gain attention, sympathy, or medical treatment. It falls under the broader category of factitious disorders, which involve the deliberate production of physical or psychological symptoms without any underlying medical cause.
This condition is often considered a form of self-harm and is driven by underlying psychological factors such as a desire for attention, a need to be cared for, or a way to communicate distress when words alone might not suffice. Individuals with dermatitis artefacta may use various methods to induce skin damage, including scratching, cutting, burning, or otherwise injuring their skin. These actions can lead to real skin damage and may even result in infections, scarring, or other complications.
Treatment of dermatitis artefacta is complex and requires a multidisciplinary approach. It involves addressing both the underlying psychological issues and the physical skin damage. Psychotherapy, particularly cognitive-behavioral therapy (CBT), can be effective in helping individuals understand and manage the psychological factors driving their behavior.
Epidemiology
Anatomy
Pathophysiology
Etiology
Genetics
Prognostic Factors
Clinical History
Age: Dermatitis artefacta can occur at any age, but it is commonly observed in adolescents & young adults. It may also be seen in older adults, though less frequently. The age of onset can provide insight into potential underlying psychological factors and triggers.
Physical Examination
Skin Lesions:
Distribution and Location:
Abrasions and Scars:
Surrounding Skin:
Nail and Hair Examination:
Age group
Associated comorbidity
Individuals with dermatitis artefacta often have underlying psychological comorbidities, such as depression, anxiety disorders, personality disorders, or somatic symptom disorder. These conditions can contribute to the development and maintenance of the self-inflicted behavior.
Associated activity
Acuity of presentation
The acuity of presentation can vary. Some individuals may present with acute and severe skin damage, while others might have a more chronic pattern with multiple episodes of self-inflicted lesions over time.
Differential Diagnoses
Other Dermatological Conditions:
Physical Illness with Skin Symptoms:
Psychological Conditions:
Laboratory Studies
Imaging Studies
Procedures
Histologic Findings
Staging
Treatment Paradigm
Assessment and Diagnosis:
Establish Therapeutic Alliance:
Psychotherapy:
by Stage
by Modality
Chemotherapy
Radiation Therapy
Surgical Interventions
Hormone Therapy
Immunotherapy
Hyperthermia
Photodynamic Therapy
Stem Cell Transplant
Targeted Therapy
Palliative Care
non-pharmacological-treatment-of-dermatitis-artefacta
Lifestyle modifications:
Psychological Support:
Stress Management:
Healthy Coping Strategies:
Social Support:
Hobbies and Activities:
Addressing Underlying Issues:
Avoidance of Triggers:
Use of Topical Antimicrobials in the treatment of Dermatitis Artefacta
Topical antimicrobial agents, such as Neomycin/polymyxin B/bacitracin (Neo-Polycin, Neosporin) and fusidic acid, are not typically used as primary treatments for dermatitis artefacta, which is a psychological condition involving self-inflicted skin lesions.
The focus of treatment for dermatitis artefacta is addressing the underlying psychological factors that drive the behavior.
Neomycin/Polymyxin B/Bacitracin (Neo-Polycin, Neosporin): Used to prevent or treat infections in minor cuts, scrapes, and burns.
Fusidic Acid: Used to treat bacterial skin infections, particularly those caused by Staphylococcus aureus.
Use of antibiotics in the treatment of Dermatitis Artefacta
Cephalexin (Keflex):
Cephalexin is a broad-spectrum antibiotic used to treat bacterial infections.
Erythromycin (E.E.C. 400, PCE, Ery-Tab):
Use of Antidepressants, SSRIs in the treatment of Dermatitis Artefacta
SSRIs are used to treat various mental health conditions, primarily depression and anxiety disorders. While SSRIs are not a direct treatment for dermatitis artefacta (self-inflicted skin lesions), they might be considered as part of a comprehensive treatment plan if the self-inflicted behavior is associated with underlying depression, anxiety, or other mental health issues.
Fluoxetine (Prozac):
Sertraline (Zoloft):
Paroxetine (Paxil, Pexeva):
Fluvoxamine (Luvox CR):
Citalopram (Celexa) and Escitalopram (Lexapro):
Use of Antidepressants, TCAs in the treatment of Dermatitis Artefacta
TCAs are not a direct treatment for dermatitis artefacta (self-inflicted skin lesions), they might be considered as part of a comprehensive treatment plan if the self-inflicted behavior is associated with underlying depression, anxiety, or other mental health issues.
Doxepin:
Amitriptyline:
Clomipramine (Anafranil):
Nortriptyline (Pamelor):
Desipramine (Norpramin):
Use of 1st Generation Antipsychotics of Dermatitis Artefacta
Antipsychotic medications, including first-generation antipsychotics like pimozide (Orap), are not typically considered as primary treatments for dermatitis artefacta (self-inflicted skin lesions).
Antipsychotics might be considered if there are concurrent mental health conditions, like psychosis or severe mood disorders, that contribute to the self-inflicted behavior.
Pimozide (Orap):
Use of 2nd Generation Antipsychotics in the treatment of Dermatitis Artefacta
Second-generation antipsychotics, also known as atypical antipsychotics, are a class of medications commonly used to treat schizophrenia, bipolar disorder, and certain mood disorders.
While these medications are not typically used as primary treatments for dermatitis artefacta (self-inflicted skin lesions), they might be considered in cases where there are concurrent severe mental health issues contributing to the self-inflicted behavior.
Risperidone (Risperdal):
Iloperidone (Fanapt):
Paliperidone (Invega):
Olanzapine (Zyprexa):
Quetiapine (Seroquel):
various-procedures-involved-in-dermatitis-artefacta
Wound Care and Dressings:
Skin Lesion Management:
Scar Management:
Infection Management:
Surgical Consultation:
management-of-dermatitis-artefacta
Assessment and Diagnosis:
Psychological Intervention:
Wound Care and Treatment:
Safety and Risk Assessment:
Supportive Care:
Psychological Treatment:
Relapse Prevention:
Emotional Regulation:
Supportive Care:
Medication
Future Trends
Dermatitis artefacta, also known as factitious dermatitis or self-inflicted dermatosis, is a psychological condition in which individuals intentionally create or exaggerate skin lesions or symptoms to gain attention, sympathy, or medical treatment. It falls under the broader category of factitious disorders, which involve the deliberate production of physical or psychological symptoms without any underlying medical cause.
This condition is often considered a form of self-harm and is driven by underlying psychological factors such as a desire for attention, a need to be cared for, or a way to communicate distress when words alone might not suffice. Individuals with dermatitis artefacta may use various methods to induce skin damage, including scratching, cutting, burning, or otherwise injuring their skin. These actions can lead to real skin damage and may even result in infections, scarring, or other complications.
Treatment of dermatitis artefacta is complex and requires a multidisciplinary approach. It involves addressing both the underlying psychological issues and the physical skin damage. Psychotherapy, particularly cognitive-behavioral therapy (CBT), can be effective in helping individuals understand and manage the psychological factors driving their behavior.
Age: Dermatitis artefacta can occur at any age, but it is commonly observed in adolescents & young adults. It may also be seen in older adults, though less frequently. The age of onset can provide insight into potential underlying psychological factors and triggers.
Skin Lesions:
Distribution and Location:
Abrasions and Scars:
Surrounding Skin:
Nail and Hair Examination:
Individuals with dermatitis artefacta often have underlying psychological comorbidities, such as depression, anxiety disorders, personality disorders, or somatic symptom disorder. These conditions can contribute to the development and maintenance of the self-inflicted behavior.
The acuity of presentation can vary. Some individuals may present with acute and severe skin damage, while others might have a more chronic pattern with multiple episodes of self-inflicted lesions over time.
Other Dermatological Conditions:
Physical Illness with Skin Symptoms:
Psychological Conditions:
Assessment and Diagnosis:
Establish Therapeutic Alliance:
Psychotherapy:
Lifestyle modifications:
Psychological Support:
Stress Management:
Healthy Coping Strategies:
Social Support:
Hobbies and Activities:
Addressing Underlying Issues:
Avoidance of Triggers:
Topical antimicrobial agents, such as Neomycin/polymyxin B/bacitracin (Neo-Polycin, Neosporin) and fusidic acid, are not typically used as primary treatments for dermatitis artefacta, which is a psychological condition involving self-inflicted skin lesions.
The focus of treatment for dermatitis artefacta is addressing the underlying psychological factors that drive the behavior.
Neomycin/Polymyxin B/Bacitracin (Neo-Polycin, Neosporin): Used to prevent or treat infections in minor cuts, scrapes, and burns.
Fusidic Acid: Used to treat bacterial skin infections, particularly those caused by Staphylococcus aureus.
Cephalexin (Keflex):
Cephalexin is a broad-spectrum antibiotic used to treat bacterial infections.
Erythromycin (E.E.C. 400, PCE, Ery-Tab):
SSRIs are used to treat various mental health conditions, primarily depression and anxiety disorders. While SSRIs are not a direct treatment for dermatitis artefacta (self-inflicted skin lesions), they might be considered as part of a comprehensive treatment plan if the self-inflicted behavior is associated with underlying depression, anxiety, or other mental health issues.
Fluoxetine (Prozac):
Sertraline (Zoloft):
Paroxetine (Paxil, Pexeva):
Fluvoxamine (Luvox CR):
Citalopram (Celexa) and Escitalopram (Lexapro):
TCAs are not a direct treatment for dermatitis artefacta (self-inflicted skin lesions), they might be considered as part of a comprehensive treatment plan if the self-inflicted behavior is associated with underlying depression, anxiety, or other mental health issues.
Doxepin:
Amitriptyline:
Clomipramine (Anafranil):
Nortriptyline (Pamelor):
Desipramine (Norpramin):
Antipsychotic medications, including first-generation antipsychotics like pimozide (Orap), are not typically considered as primary treatments for dermatitis artefacta (self-inflicted skin lesions).
Antipsychotics might be considered if there are concurrent mental health conditions, like psychosis or severe mood disorders, that contribute to the self-inflicted behavior.
Pimozide (Orap):
Second-generation antipsychotics, also known as atypical antipsychotics, are a class of medications commonly used to treat schizophrenia, bipolar disorder, and certain mood disorders.
While these medications are not typically used as primary treatments for dermatitis artefacta (self-inflicted skin lesions), they might be considered in cases where there are concurrent severe mental health issues contributing to the self-inflicted behavior.
Risperidone (Risperdal):
Iloperidone (Fanapt):
Paliperidone (Invega):
Olanzapine (Zyprexa):
Quetiapine (Seroquel):
Wound Care and Dressings:
Skin Lesion Management:
Scar Management:
Infection Management:
Surgical Consultation:
Assessment and Diagnosis:
Psychological Intervention:
Wound Care and Treatment:
Safety and Risk Assessment:
Supportive Care:
Psychological Treatment:
Relapse Prevention:
Emotional Regulation:
Supportive Care:
Dermatitis artefacta, also known as factitious dermatitis or self-inflicted dermatosis, is a psychological condition in which individuals intentionally create or exaggerate skin lesions or symptoms to gain attention, sympathy, or medical treatment. It falls under the broader category of factitious disorders, which involve the deliberate production of physical or psychological symptoms without any underlying medical cause.
This condition is often considered a form of self-harm and is driven by underlying psychological factors such as a desire for attention, a need to be cared for, or a way to communicate distress when words alone might not suffice. Individuals with dermatitis artefacta may use various methods to induce skin damage, including scratching, cutting, burning, or otherwise injuring their skin. These actions can lead to real skin damage and may even result in infections, scarring, or other complications.
Treatment of dermatitis artefacta is complex and requires a multidisciplinary approach. It involves addressing both the underlying psychological issues and the physical skin damage. Psychotherapy, particularly cognitive-behavioral therapy (CBT), can be effective in helping individuals understand and manage the psychological factors driving their behavior.
Age: Dermatitis artefacta can occur at any age, but it is commonly observed in adolescents & young adults. It may also be seen in older adults, though less frequently. The age of onset can provide insight into potential underlying psychological factors and triggers.
Skin Lesions:
Distribution and Location:
Abrasions and Scars:
Surrounding Skin:
Nail and Hair Examination:
Individuals with dermatitis artefacta often have underlying psychological comorbidities, such as depression, anxiety disorders, personality disorders, or somatic symptom disorder. These conditions can contribute to the development and maintenance of the self-inflicted behavior.
The acuity of presentation can vary. Some individuals may present with acute and severe skin damage, while others might have a more chronic pattern with multiple episodes of self-inflicted lesions over time.
Other Dermatological Conditions:
Physical Illness with Skin Symptoms:
Psychological Conditions:
Assessment and Diagnosis:
Establish Therapeutic Alliance:
Psychotherapy:
Lifestyle modifications:
Psychological Support:
Stress Management:
Healthy Coping Strategies:
Social Support:
Hobbies and Activities:
Addressing Underlying Issues:
Avoidance of Triggers:
Topical antimicrobial agents, such as Neomycin/polymyxin B/bacitracin (Neo-Polycin, Neosporin) and fusidic acid, are not typically used as primary treatments for dermatitis artefacta, which is a psychological condition involving self-inflicted skin lesions.
The focus of treatment for dermatitis artefacta is addressing the underlying psychological factors that drive the behavior.
Neomycin/Polymyxin B/Bacitracin (Neo-Polycin, Neosporin): Used to prevent or treat infections in minor cuts, scrapes, and burns.
Fusidic Acid: Used to treat bacterial skin infections, particularly those caused by Staphylococcus aureus.
Cephalexin (Keflex):
Cephalexin is a broad-spectrum antibiotic used to treat bacterial infections.
Erythromycin (E.E.C. 400, PCE, Ery-Tab):
SSRIs are used to treat various mental health conditions, primarily depression and anxiety disorders. While SSRIs are not a direct treatment for dermatitis artefacta (self-inflicted skin lesions), they might be considered as part of a comprehensive treatment plan if the self-inflicted behavior is associated with underlying depression, anxiety, or other mental health issues.
Fluoxetine (Prozac):
Sertraline (Zoloft):
Paroxetine (Paxil, Pexeva):
Fluvoxamine (Luvox CR):
Citalopram (Celexa) and Escitalopram (Lexapro):
TCAs are not a direct treatment for dermatitis artefacta (self-inflicted skin lesions), they might be considered as part of a comprehensive treatment plan if the self-inflicted behavior is associated with underlying depression, anxiety, or other mental health issues.
Doxepin:
Amitriptyline:
Clomipramine (Anafranil):
Nortriptyline (Pamelor):
Desipramine (Norpramin):
Antipsychotic medications, including first-generation antipsychotics like pimozide (Orap), are not typically considered as primary treatments for dermatitis artefacta (self-inflicted skin lesions).
Antipsychotics might be considered if there are concurrent mental health conditions, like psychosis or severe mood disorders, that contribute to the self-inflicted behavior.
Pimozide (Orap):
Second-generation antipsychotics, also known as atypical antipsychotics, are a class of medications commonly used to treat schizophrenia, bipolar disorder, and certain mood disorders.
While these medications are not typically used as primary treatments for dermatitis artefacta (self-inflicted skin lesions), they might be considered in cases where there are concurrent severe mental health issues contributing to the self-inflicted behavior.
Risperidone (Risperdal):
Iloperidone (Fanapt):
Paliperidone (Invega):
Olanzapine (Zyprexa):
Quetiapine (Seroquel):
Wound Care and Dressings:
Skin Lesion Management:
Scar Management:
Infection Management:
Surgical Consultation:
Assessment and Diagnosis:
Psychological Intervention:
Wound Care and Treatment:
Safety and Risk Assessment:
Supportive Care:
Psychological Treatment:
Relapse Prevention:
Emotional Regulation:
Supportive Care:
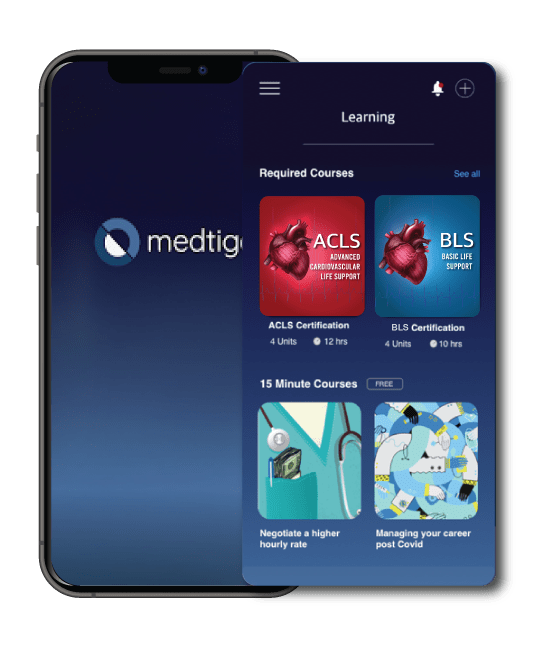
Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.
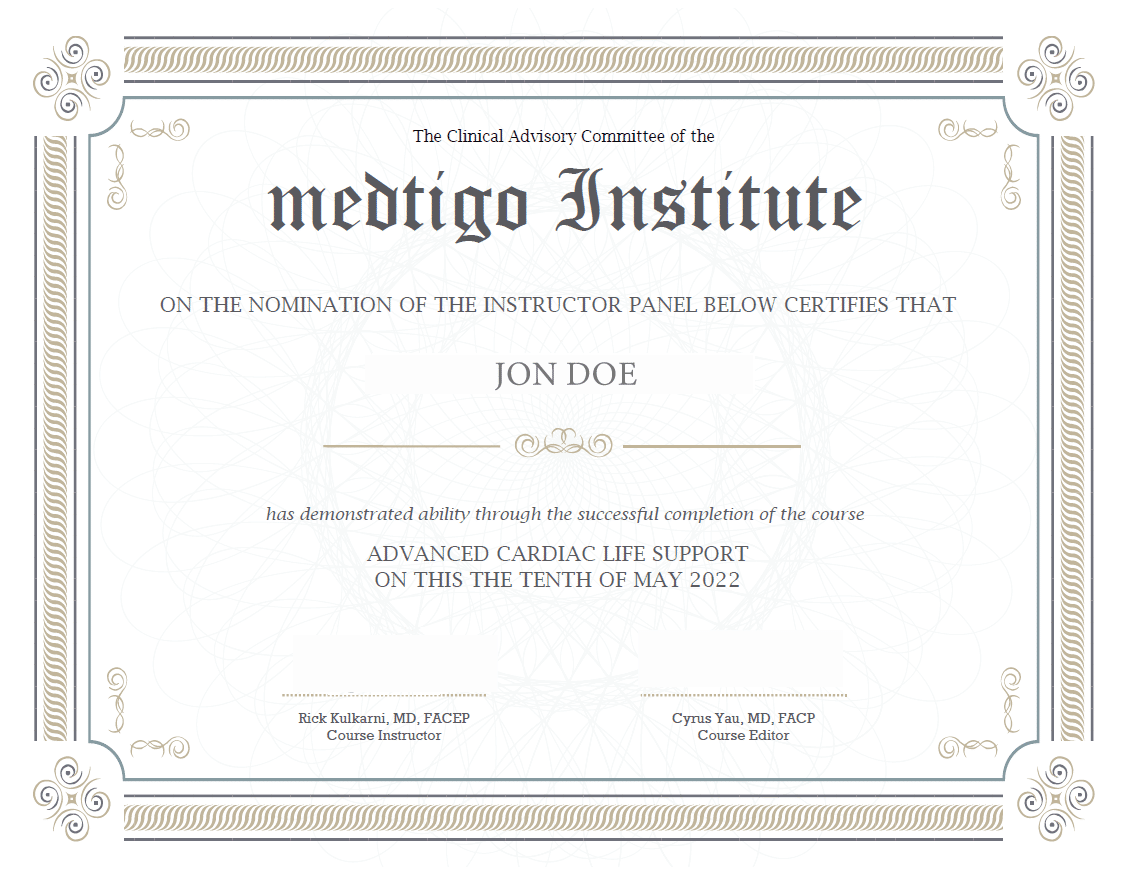
On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.
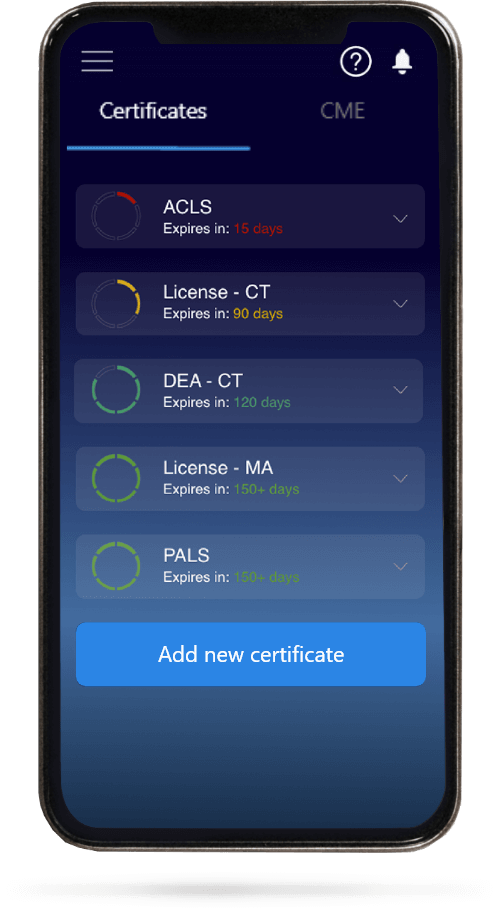
When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.