Human Doctor or AI? Understanding Patient Preferences in AI-Assisted Medical Care
March 6, 2026
Background
Diabetes mellitus is a chronic metabolic disorder characterized by high hyperglycemia resulting from defects in insulin production, insulin action, or both. Insulin is a hormone produced by the pancreas that plays a crucial role in regulating blood sugar levels and facilitating glucose uptake by cells for energy.
The origin of diabetes mellitus dates back thousands of years. The term “diabetes” comes from the Greek word for “siphon” or “to pass through,” referring to the excessive urination associated with the condition. The term “mellitus” was added in the 17th century to describe the sweet taste of the urine of people with diabetes.
While the exact origins of diabetes mellitus are not entirely clear, historical records and research indicate that the disease has been present for centuries. The earliest known written documentation describing symptoms resembling diabetes dates back to ancient Egyptian manuscripts from around 1500 BCE. These documents describe a condition characterized by excessive thirst, frequent urination, and weight loss.
Epidemiology
Diabetes has reached epidemic proportions globally. According to the International Diabetes Federation (IDF), approximately 463 million adults (aged 20-79) had diabetes in 2019. This number will rise to 700 million by 2045 if current trends continue. Type 1 diabetes typically begins in childhood or adolescence and accounts for about 5-10% of all diagnosed cases. Its prevalence varies across different populations and regions, with the highest rates reported in Northern Europe and the lowest in parts of Asia.
Type 2 diabetes is the most common form, accounting for approximately 90-95% of all diabetes cases. It is strongly associated with lifestyle factors, such as obesity, physical inactivity, and unhealthy diets. The prevalence of type 2 diabetes has been increasing rapidly worldwide. It is more prevalent in older age groups but is increasingly affecting younger individuals due to rising obesity rates.
Diabetes poses a significant burden on healthcare systems globally. It requires long-term management, including regular monitoring, medication, lifestyle modifications, and diabetes education. The economic burden associated with diabetes, including direct medical costs and indirect costs due to productivity loss, is substantial.
Anatomy
Pathophysiology
Patients with diabetes mellitus are at risk of developing hyperglycemia, but the underlying pathology can be multifactorial and complex. Hyperglycemia itself can impair the function of pancreatic beta cells, leading to decreased insulin secretion. This sets off a vicious cycle where hyperglycemia contributes to further metabolic dysfunction. Although there is no universally defined cutoff, blood glucose levels above 180 mg/dL are typically considered hyperglycemic.
At levels above 250 mg/dL, patients often experience symptoms such as polyuria (excessive urination) and polydipsia (excessive thirst) due to osmotic diuresis caused by saturated glucose transporters in the nephrons. Insulin resistance, which is a hallmark of type 2 diabetes (T2DM), is influenced by various factors, including elevated fatty acids and proinflammatory cytokines.
These factors impede glucose transport and promote an increased breakdown of fat. In response to inadequate insulin action, the body compensates by inappropriately increasing glucagon levels, further exacerbating hyperglycemia. While insulin resistance is a key component of T2DM, the disease fully manifests when insulin is insufficient to compensate for the resistance. Chronic hyperglycemia also leads to nonenzymatic glycation of proteins and lipids in the body.
This process can be assessed by measuring glycated hemoglobin (HbA1c) levels. Glycation contributes to the damage of small blood vessels, particularly in the retina, kidneys, and peripheral nerves. Higher glucose levels accelerate this damage. Consequently, diabetic complications such as diabetic nephropathy, retinopathy, and neuropathy can occur, leading to potential outcomes such as blindness, the need for dialysis, and amputations, respectively.
Etiology
Within the pancreas, the islets of Langerhans contain two main types of endocrine cells: beta cells, which produce insulin, and alpha cells, which secrete glucagon. These cells dynamically adjust their hormone secretions in response to the glucose environment. Maintaining a balance between insulin and glucagon is crucial for appropriately regulating blood glucose levels. However, in diabetes mellitus (DM), there is a disruption in this balance, resulting in abnormal glucose levels.
Type 1 diabetes mellitus (T1DM) is characterized by the destruction of beta cells in the pancreas, typically due to an autoimmune process. As a result, there is a severe deficiency or absence of insulin production. In contrast, type 2 diabetes mellitus (T2DM) has a more gradual onset and is associated with an imbalance between insulin levels and insulin sensitivity, leading to a functional deficit of insulin. Insulin resistance, a key factor in T2DM, is influenced by multiple factors, including obesity and aging.
Genetic factors play a significant role in both types of diabetes. Specific genetic loci have been identified as risk factors for T1DM, including major histocompatibility complex (MHC) and human leukocyte antigen (HLA) genes. In T2DM, the genetic background is also important, and studies have identified approximately 50 polymorphisms associated with an increased risk or protection against the disease. These genetic variations affect various pathways involved in the development of diabetes, such as pancreatic development, insulin synthesis and secretion, amyloid deposition in beta cells, insulin resistance, and regulation of gluconeogenesis.
Genetics
Prognostic Factors
Clinical History
Clinical History
During the patient’s history gathering information about the patient’s family history, autoimmune diseases, and insulin resistance is crucial in diagnosing diabetes mellitus (DM). While DM can initially present asymptomatically, patients typically exhibit polyuria (excessive urination), polydipsia (excessive thirst), and unexplained weight loss when symptoms arise. It is important to inquire about the patient’s family history of diabetes, as DM has a significant genetic component.
Having a first-degree relative, such as a parent or sibling, with DM increases an individual’s risk of developing the disease. Additionally, a family history of autoimmune diseases, particularly type 1 diabetes, may suggest a higher likelihood of autoimmune-related DM. As DM can be asymptomatic in its early stages, it is crucial to assess for any potential symptoms that may have developed. Despite normal or increased food intake, unexplained weight loss may also indicate diabetes.
Physical Examination
Physical Examination
Certain findings may be observed during a physical examination of a person with hyperglycemia. Poor skin turgor can be evident due to dehydration caused by excessive urination. In cases where ketosis is present, the patient’s breath may have a distinctive fruity odor. In the context of diabetic ketoacidosis, additional signs can be noted. Kussmaul respirations, which are deep and rapid breathing patterns, may be observed. Fatigue, nausea, and vomiting can also manifest as manifestations of DKA.
Hemorrhages or exudates on the macula may be seen in cases of diabetic retinopathy. In more advanced stages, retinal venules can appear dilated or impeded. The proliferation of new blood vessels is of particular concern as it can accelerate macular edema and retinal hemorrhages, potentially leading to blindness. Ophthalmologists play a vital role in assessing and managing diabetic eye complications.
While both type 1 diabetes and type 2 diabetes can present with similar symptoms, there are distinguishing factors based on clinical history and examination. T2DM patients tend to be overweight or obese and commonly exhibit signs of insulin resistance. These signs may include hyperpigmented and velvety patches on the skin in areas such as the neck and inguinal folds or axillary folds.
Patients with a more prolonged duration of hyperglycemia may experience additional symptoms. Blurry vision, numbness, frequent yeast infections, or neuropathic pain can occur. Clinicians must inquire about any recent skin changes in the feet during each visit, as the diabetic foot exam involving the monofilament test should be a routine part of the physical examination.
Age group
Associated comorbidity
Associated activity
Acuity of presentation
Differential Diagnoses
Differential Diagnoses
Gestational Diabetes
Thyroid Disorders
Hereditary Hemochromatosis
Laboratory Studies
Imaging Studies
Procedures
Histologic Findings
Staging
Treatment Paradigm
The treatment approaches for type 1 diabetes mellitus (T1DM), and type 2 diabetes mellitus (T2DM) differ based on the underlying mechanisms of the disease. In T1DM, characterized by the absence of insulin, the mainstay of treatment is insulin administration. This is typically done through daily injections or by using an insulin pump. The goal is to provide the body with insulin to regulate blood glucose levels effectively. For T2DM, initial treatment may involve lifestyle modifications focusing on diet and exercise.
These measures can help control blood glucose levels, especially in the early stages of the disease. However, as the disease progresses, additional therapies may be required to target insulin sensitivity or increase insulin secretion by the pancreas. In some cases, T2DM may progress to a point where insulin administration becomes necessary, particularly when glucose management is inadequate. Additionally, for morbidly obese individuals with T2DM who have not responded to other treatments and have significant comorbidities, bariatric surgery may be considered as a means to normalize glucose levels.
Managing the complications of diabetes is also crucial. The FDA has approved medications such as duloxetine and pregabalin for treating diabetic peripheral neuropathy, a common complication. Tricyclic antidepressants and anticonvulsants are also occasionally used to manage the pain associated with diabetic neuropathy. Regular screenings are essential for early detection and management of microvascular complications in diabetes.
Qualified medical personnel should perform regular diabetic retinal exams to assess for diabetic retinopathy. Neurologic examinations, including monofilament testing, can identify patients with neuropathy at risk for amputation. By employing a combination of medication, lifestyle modifications, and regular screenings, healthcare providers aim to achieve optimal glucose control and prevent or manage the complications associated with diabetes.
by Stage
by Modality
Chemotherapy
Radiation Therapy
Surgical Interventions
Hormone Therapy
Immunotherapy
Hyperthermia
Photodynamic Therapy
Stem Cell Transplant
Targeted Therapy
Palliative Care
Medication
2mg/30 mg or 4mg/30 mg orally every day The Maximum dose is 8mg/45mg
The recommended dosage is 300 mg two times orally daily
Indicated for Angina, Diabetes mellitus
50 to 200 mg orally every day
CHF
100 mg orally in divided two-three times a day
Myocardial preservation for the heart surgery
200 mg orally every day
50 - 200 mg daily
More than 80 units of insulin beef is required in a day.
The 1980s observed a significant decrease in the usage of animal insulin as human insulin became available through recombinant DNA technology.
In the US, commercial supplies of beef, pork, and pork insulin are no longer available. If a patient cannot receive human insulin treatment, the US FDA may permit the personal importation of cattle or pork insulin from another nation.
The dosage must be personalized and adjusted based on the patient's metabolic requirements, results from blood glucose monitoring, and the goal of glycemic control
It is generally administered in combination with intermediate- or long-acting insulin
When administered via subcutaneous injection, inject approximately 30 minutes before a meal into the thigh, upper arm, abdomen, or buttock
If administered via IV infusion, it should be done only under medical supervision with close monitoring of blood glucose and potassium levels
Dose adjustments may be necessary when transitioning from another insulin or experiencing changes in meal patterns, physical activity, hepatic or renal function, or during acute illness
Dosage recommendations may vary among individual products and countries (refer to detailed product information or local guidelines)
• Type 1: Typically, total daily insulin requirements fall within the range of 0.5 to 1 unit per kg per day
• Type 2: Initial doses often range from 4 to 6 units or 0.1 units per kg or 10% of the basal insulin dose
• Utilize HbA1c values to inform therapy decisions and refer to current guidelines for optimal target ranges
Dose Adjustments
Limited data is available
M. paradisiaca fruit peels show excellent anti-diabetic effects, reducing blood sugar levels by up to 25.5% and 20.5%, respectively, at a dosage of 500 mg/kg body weight
alpha-Lipoic acid/minerals/multivitamins
One capsule every day
10-15 g orally in divided doses with food
Hydroalcoholic extract: 1 g orally daily
Seed: 5 g orally daily
Take one tablet orally twice daily with food
Off-label:
It is given at 5 mg/kg intraperitoneally for 15 days, displays antioxidant properties and protects the pancreas in rats with streptozotocin-induced diabetes
Moreover, a single intraperitoneal dose ranging from 40 to 200 mg/kg exhibits significant protection against α-amanitin intoxication in mice
Off-label:
Traditional suggestions propose up to 12 grams of dry root daily and up to 2 milliliters of liquid seed extract
Note:
It's crucial to be cautious as these traditional recommendations lack solid clinical support, emphasizing the need for further research to establish appropriate burdock dosages
Typically, total daily insulin requirements fall within the range of 0.5 to 1 unit per kg per day
Safety and efficacy are not seen in pediatrics < 6
Administer via subcutaneous injection about 30 minutes before a meal
The dosage should be tailored and adapted based on the patient's metabolic requirements, blood glucose monitoring outcomes, and the desired glycemic control goal
Specific product and country guidelines, as outlined in detailed product information or local protocols, may offer varying dosage recommendations
Type 2: The initial doses typically fall within the range between 4 and 6 units, or 0.1 units per kg, or 10% of the basal insulin dose
Utilize HbA1c values to inform therapy decisions; refer to current guidelines for optimal target ranges
Future Trends
References
Diabetes mellitus is a chronic metabolic disorder characterized by high hyperglycemia resulting from defects in insulin production, insulin action, or both. Insulin is a hormone produced by the pancreas that plays a crucial role in regulating blood sugar levels and facilitating glucose uptake by cells for energy.
The origin of diabetes mellitus dates back thousands of years. The term “diabetes” comes from the Greek word for “siphon” or “to pass through,” referring to the excessive urination associated with the condition. The term “mellitus” was added in the 17th century to describe the sweet taste of the urine of people with diabetes.
While the exact origins of diabetes mellitus are not entirely clear, historical records and research indicate that the disease has been present for centuries. The earliest known written documentation describing symptoms resembling diabetes dates back to ancient Egyptian manuscripts from around 1500 BCE. These documents describe a condition characterized by excessive thirst, frequent urination, and weight loss.
Diabetes has reached epidemic proportions globally. According to the International Diabetes Federation (IDF), approximately 463 million adults (aged 20-79) had diabetes in 2019. This number will rise to 700 million by 2045 if current trends continue. Type 1 diabetes typically begins in childhood or adolescence and accounts for about 5-10% of all diagnosed cases. Its prevalence varies across different populations and regions, with the highest rates reported in Northern Europe and the lowest in parts of Asia.
Type 2 diabetes is the most common form, accounting for approximately 90-95% of all diabetes cases. It is strongly associated with lifestyle factors, such as obesity, physical inactivity, and unhealthy diets. The prevalence of type 2 diabetes has been increasing rapidly worldwide. It is more prevalent in older age groups but is increasingly affecting younger individuals due to rising obesity rates.
Diabetes poses a significant burden on healthcare systems globally. It requires long-term management, including regular monitoring, medication, lifestyle modifications, and diabetes education. The economic burden associated with diabetes, including direct medical costs and indirect costs due to productivity loss, is substantial.
Patients with diabetes mellitus are at risk of developing hyperglycemia, but the underlying pathology can be multifactorial and complex. Hyperglycemia itself can impair the function of pancreatic beta cells, leading to decreased insulin secretion. This sets off a vicious cycle where hyperglycemia contributes to further metabolic dysfunction. Although there is no universally defined cutoff, blood glucose levels above 180 mg/dL are typically considered hyperglycemic.
At levels above 250 mg/dL, patients often experience symptoms such as polyuria (excessive urination) and polydipsia (excessive thirst) due to osmotic diuresis caused by saturated glucose transporters in the nephrons. Insulin resistance, which is a hallmark of type 2 diabetes (T2DM), is influenced by various factors, including elevated fatty acids and proinflammatory cytokines.
These factors impede glucose transport and promote an increased breakdown of fat. In response to inadequate insulin action, the body compensates by inappropriately increasing glucagon levels, further exacerbating hyperglycemia. While insulin resistance is a key component of T2DM, the disease fully manifests when insulin is insufficient to compensate for the resistance. Chronic hyperglycemia also leads to nonenzymatic glycation of proteins and lipids in the body.
This process can be assessed by measuring glycated hemoglobin (HbA1c) levels. Glycation contributes to the damage of small blood vessels, particularly in the retina, kidneys, and peripheral nerves. Higher glucose levels accelerate this damage. Consequently, diabetic complications such as diabetic nephropathy, retinopathy, and neuropathy can occur, leading to potential outcomes such as blindness, the need for dialysis, and amputations, respectively.
Within the pancreas, the islets of Langerhans contain two main types of endocrine cells: beta cells, which produce insulin, and alpha cells, which secrete glucagon. These cells dynamically adjust their hormone secretions in response to the glucose environment. Maintaining a balance between insulin and glucagon is crucial for appropriately regulating blood glucose levels. However, in diabetes mellitus (DM), there is a disruption in this balance, resulting in abnormal glucose levels.
Type 1 diabetes mellitus (T1DM) is characterized by the destruction of beta cells in the pancreas, typically due to an autoimmune process. As a result, there is a severe deficiency or absence of insulin production. In contrast, type 2 diabetes mellitus (T2DM) has a more gradual onset and is associated with an imbalance between insulin levels and insulin sensitivity, leading to a functional deficit of insulin. Insulin resistance, a key factor in T2DM, is influenced by multiple factors, including obesity and aging.
Genetic factors play a significant role in both types of diabetes. Specific genetic loci have been identified as risk factors for T1DM, including major histocompatibility complex (MHC) and human leukocyte antigen (HLA) genes. In T2DM, the genetic background is also important, and studies have identified approximately 50 polymorphisms associated with an increased risk or protection against the disease. These genetic variations affect various pathways involved in the development of diabetes, such as pancreatic development, insulin synthesis and secretion, amyloid deposition in beta cells, insulin resistance, and regulation of gluconeogenesis.
Clinical History
During the patient’s history gathering information about the patient’s family history, autoimmune diseases, and insulin resistance is crucial in diagnosing diabetes mellitus (DM). While DM can initially present asymptomatically, patients typically exhibit polyuria (excessive urination), polydipsia (excessive thirst), and unexplained weight loss when symptoms arise. It is important to inquire about the patient’s family history of diabetes, as DM has a significant genetic component.
Having a first-degree relative, such as a parent or sibling, with DM increases an individual’s risk of developing the disease. Additionally, a family history of autoimmune diseases, particularly type 1 diabetes, may suggest a higher likelihood of autoimmune-related DM. As DM can be asymptomatic in its early stages, it is crucial to assess for any potential symptoms that may have developed. Despite normal or increased food intake, unexplained weight loss may also indicate diabetes.
Physical Examination
Certain findings may be observed during a physical examination of a person with hyperglycemia. Poor skin turgor can be evident due to dehydration caused by excessive urination. In cases where ketosis is present, the patient’s breath may have a distinctive fruity odor. In the context of diabetic ketoacidosis, additional signs can be noted. Kussmaul respirations, which are deep and rapid breathing patterns, may be observed. Fatigue, nausea, and vomiting can also manifest as manifestations of DKA.
Hemorrhages or exudates on the macula may be seen in cases of diabetic retinopathy. In more advanced stages, retinal venules can appear dilated or impeded. The proliferation of new blood vessels is of particular concern as it can accelerate macular edema and retinal hemorrhages, potentially leading to blindness. Ophthalmologists play a vital role in assessing and managing diabetic eye complications.
While both type 1 diabetes and type 2 diabetes can present with similar symptoms, there are distinguishing factors based on clinical history and examination. T2DM patients tend to be overweight or obese and commonly exhibit signs of insulin resistance. These signs may include hyperpigmented and velvety patches on the skin in areas such as the neck and inguinal folds or axillary folds.
Patients with a more prolonged duration of hyperglycemia may experience additional symptoms. Blurry vision, numbness, frequent yeast infections, or neuropathic pain can occur. Clinicians must inquire about any recent skin changes in the feet during each visit, as the diabetic foot exam involving the monofilament test should be a routine part of the physical examination.
Differential Diagnoses
Gestational Diabetes
Thyroid Disorders
Hereditary Hemochromatosis
The treatment approaches for type 1 diabetes mellitus (T1DM), and type 2 diabetes mellitus (T2DM) differ based on the underlying mechanisms of the disease. In T1DM, characterized by the absence of insulin, the mainstay of treatment is insulin administration. This is typically done through daily injections or by using an insulin pump. The goal is to provide the body with insulin to regulate blood glucose levels effectively. For T2DM, initial treatment may involve lifestyle modifications focusing on diet and exercise.
These measures can help control blood glucose levels, especially in the early stages of the disease. However, as the disease progresses, additional therapies may be required to target insulin sensitivity or increase insulin secretion by the pancreas. In some cases, T2DM may progress to a point where insulin administration becomes necessary, particularly when glucose management is inadequate. Additionally, for morbidly obese individuals with T2DM who have not responded to other treatments and have significant comorbidities, bariatric surgery may be considered as a means to normalize glucose levels.
Managing the complications of diabetes is also crucial. The FDA has approved medications such as duloxetine and pregabalin for treating diabetic peripheral neuropathy, a common complication. Tricyclic antidepressants and anticonvulsants are also occasionally used to manage the pain associated with diabetic neuropathy. Regular screenings are essential for early detection and management of microvascular complications in diabetes.
Qualified medical personnel should perform regular diabetic retinal exams to assess for diabetic retinopathy. Neurologic examinations, including monofilament testing, can identify patients with neuropathy at risk for amputation. By employing a combination of medication, lifestyle modifications, and regular screenings, healthcare providers aim to achieve optimal glucose control and prevent or manage the complications associated with diabetes.
Diabetes mellitus is a chronic metabolic disorder characterized by high hyperglycemia resulting from defects in insulin production, insulin action, or both. Insulin is a hormone produced by the pancreas that plays a crucial role in regulating blood sugar levels and facilitating glucose uptake by cells for energy.
The origin of diabetes mellitus dates back thousands of years. The term “diabetes” comes from the Greek word for “siphon” or “to pass through,” referring to the excessive urination associated with the condition. The term “mellitus” was added in the 17th century to describe the sweet taste of the urine of people with diabetes.
While the exact origins of diabetes mellitus are not entirely clear, historical records and research indicate that the disease has been present for centuries. The earliest known written documentation describing symptoms resembling diabetes dates back to ancient Egyptian manuscripts from around 1500 BCE. These documents describe a condition characterized by excessive thirst, frequent urination, and weight loss.
Diabetes has reached epidemic proportions globally. According to the International Diabetes Federation (IDF), approximately 463 million adults (aged 20-79) had diabetes in 2019. This number will rise to 700 million by 2045 if current trends continue. Type 1 diabetes typically begins in childhood or adolescence and accounts for about 5-10% of all diagnosed cases. Its prevalence varies across different populations and regions, with the highest rates reported in Northern Europe and the lowest in parts of Asia.
Type 2 diabetes is the most common form, accounting for approximately 90-95% of all diabetes cases. It is strongly associated with lifestyle factors, such as obesity, physical inactivity, and unhealthy diets. The prevalence of type 2 diabetes has been increasing rapidly worldwide. It is more prevalent in older age groups but is increasingly affecting younger individuals due to rising obesity rates.
Diabetes poses a significant burden on healthcare systems globally. It requires long-term management, including regular monitoring, medication, lifestyle modifications, and diabetes education. The economic burden associated with diabetes, including direct medical costs and indirect costs due to productivity loss, is substantial.
Patients with diabetes mellitus are at risk of developing hyperglycemia, but the underlying pathology can be multifactorial and complex. Hyperglycemia itself can impair the function of pancreatic beta cells, leading to decreased insulin secretion. This sets off a vicious cycle where hyperglycemia contributes to further metabolic dysfunction. Although there is no universally defined cutoff, blood glucose levels above 180 mg/dL are typically considered hyperglycemic.
At levels above 250 mg/dL, patients often experience symptoms such as polyuria (excessive urination) and polydipsia (excessive thirst) due to osmotic diuresis caused by saturated glucose transporters in the nephrons. Insulin resistance, which is a hallmark of type 2 diabetes (T2DM), is influenced by various factors, including elevated fatty acids and proinflammatory cytokines.
These factors impede glucose transport and promote an increased breakdown of fat. In response to inadequate insulin action, the body compensates by inappropriately increasing glucagon levels, further exacerbating hyperglycemia. While insulin resistance is a key component of T2DM, the disease fully manifests when insulin is insufficient to compensate for the resistance. Chronic hyperglycemia also leads to nonenzymatic glycation of proteins and lipids in the body.
This process can be assessed by measuring glycated hemoglobin (HbA1c) levels. Glycation contributes to the damage of small blood vessels, particularly in the retina, kidneys, and peripheral nerves. Higher glucose levels accelerate this damage. Consequently, diabetic complications such as diabetic nephropathy, retinopathy, and neuropathy can occur, leading to potential outcomes such as blindness, the need for dialysis, and amputations, respectively.
Within the pancreas, the islets of Langerhans contain two main types of endocrine cells: beta cells, which produce insulin, and alpha cells, which secrete glucagon. These cells dynamically adjust their hormone secretions in response to the glucose environment. Maintaining a balance between insulin and glucagon is crucial for appropriately regulating blood glucose levels. However, in diabetes mellitus (DM), there is a disruption in this balance, resulting in abnormal glucose levels.
Type 1 diabetes mellitus (T1DM) is characterized by the destruction of beta cells in the pancreas, typically due to an autoimmune process. As a result, there is a severe deficiency or absence of insulin production. In contrast, type 2 diabetes mellitus (T2DM) has a more gradual onset and is associated with an imbalance between insulin levels and insulin sensitivity, leading to a functional deficit of insulin. Insulin resistance, a key factor in T2DM, is influenced by multiple factors, including obesity and aging.
Genetic factors play a significant role in both types of diabetes. Specific genetic loci have been identified as risk factors for T1DM, including major histocompatibility complex (MHC) and human leukocyte antigen (HLA) genes. In T2DM, the genetic background is also important, and studies have identified approximately 50 polymorphisms associated with an increased risk or protection against the disease. These genetic variations affect various pathways involved in the development of diabetes, such as pancreatic development, insulin synthesis and secretion, amyloid deposition in beta cells, insulin resistance, and regulation of gluconeogenesis.
Clinical History
During the patient’s history gathering information about the patient’s family history, autoimmune diseases, and insulin resistance is crucial in diagnosing diabetes mellitus (DM). While DM can initially present asymptomatically, patients typically exhibit polyuria (excessive urination), polydipsia (excessive thirst), and unexplained weight loss when symptoms arise. It is important to inquire about the patient’s family history of diabetes, as DM has a significant genetic component.
Having a first-degree relative, such as a parent or sibling, with DM increases an individual’s risk of developing the disease. Additionally, a family history of autoimmune diseases, particularly type 1 diabetes, may suggest a higher likelihood of autoimmune-related DM. As DM can be asymptomatic in its early stages, it is crucial to assess for any potential symptoms that may have developed. Despite normal or increased food intake, unexplained weight loss may also indicate diabetes.
Physical Examination
Certain findings may be observed during a physical examination of a person with hyperglycemia. Poor skin turgor can be evident due to dehydration caused by excessive urination. In cases where ketosis is present, the patient’s breath may have a distinctive fruity odor. In the context of diabetic ketoacidosis, additional signs can be noted. Kussmaul respirations, which are deep and rapid breathing patterns, may be observed. Fatigue, nausea, and vomiting can also manifest as manifestations of DKA.
Hemorrhages or exudates on the macula may be seen in cases of diabetic retinopathy. In more advanced stages, retinal venules can appear dilated or impeded. The proliferation of new blood vessels is of particular concern as it can accelerate macular edema and retinal hemorrhages, potentially leading to blindness. Ophthalmologists play a vital role in assessing and managing diabetic eye complications.
While both type 1 diabetes and type 2 diabetes can present with similar symptoms, there are distinguishing factors based on clinical history and examination. T2DM patients tend to be overweight or obese and commonly exhibit signs of insulin resistance. These signs may include hyperpigmented and velvety patches on the skin in areas such as the neck and inguinal folds or axillary folds.
Patients with a more prolonged duration of hyperglycemia may experience additional symptoms. Blurry vision, numbness, frequent yeast infections, or neuropathic pain can occur. Clinicians must inquire about any recent skin changes in the feet during each visit, as the diabetic foot exam involving the monofilament test should be a routine part of the physical examination.
Differential Diagnoses
Gestational Diabetes
Thyroid Disorders
Hereditary Hemochromatosis
The treatment approaches for type 1 diabetes mellitus (T1DM), and type 2 diabetes mellitus (T2DM) differ based on the underlying mechanisms of the disease. In T1DM, characterized by the absence of insulin, the mainstay of treatment is insulin administration. This is typically done through daily injections or by using an insulin pump. The goal is to provide the body with insulin to regulate blood glucose levels effectively. For T2DM, initial treatment may involve lifestyle modifications focusing on diet and exercise.
These measures can help control blood glucose levels, especially in the early stages of the disease. However, as the disease progresses, additional therapies may be required to target insulin sensitivity or increase insulin secretion by the pancreas. In some cases, T2DM may progress to a point where insulin administration becomes necessary, particularly when glucose management is inadequate. Additionally, for morbidly obese individuals with T2DM who have not responded to other treatments and have significant comorbidities, bariatric surgery may be considered as a means to normalize glucose levels.
Managing the complications of diabetes is also crucial. The FDA has approved medications such as duloxetine and pregabalin for treating diabetic peripheral neuropathy, a common complication. Tricyclic antidepressants and anticonvulsants are also occasionally used to manage the pain associated with diabetic neuropathy. Regular screenings are essential for early detection and management of microvascular complications in diabetes.
Qualified medical personnel should perform regular diabetic retinal exams to assess for diabetic retinopathy. Neurologic examinations, including monofilament testing, can identify patients with neuropathy at risk for amputation. By employing a combination of medication, lifestyle modifications, and regular screenings, healthcare providers aim to achieve optimal glucose control and prevent or manage the complications associated with diabetes.
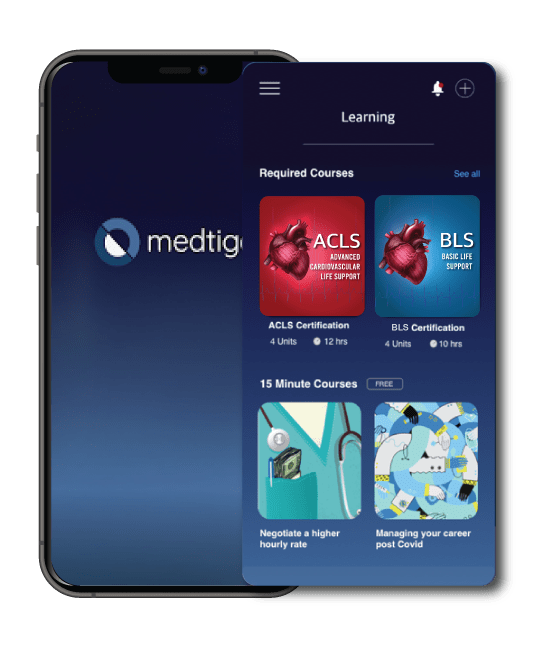
Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.
On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.
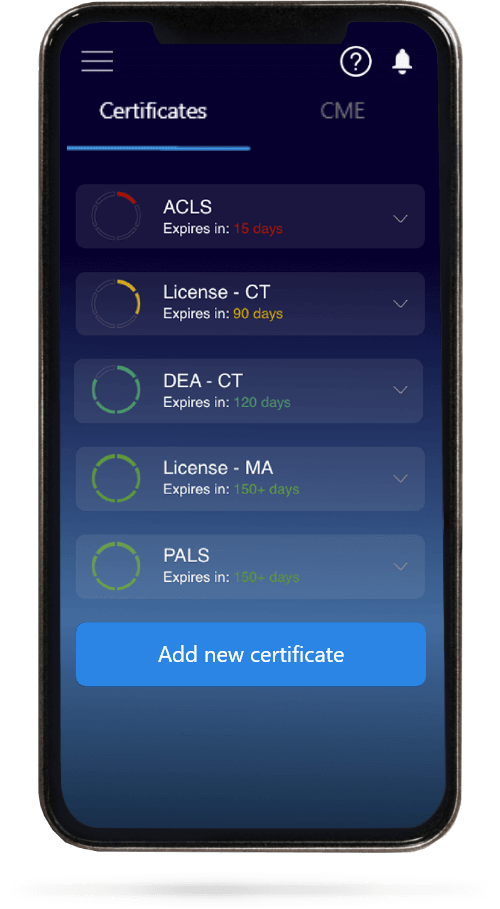
When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.