Ostarine: The ‘Invisible’ Doping Threat Trapping Innocent Athletes
February 18, 2026
Background
Head and neck cancer is a term used to describe a group of cancers that usually develop in the squamous cells lining the mucosal surfaces of the head and neck region. This includes the oral cavity (mouth), throat (pharynx), voice box (larynx), and the nasal cavity and sinuses. The most common type of head and neck cancer is squamous cell carcinoma. It can arise in various locations, including the oral cavity (lips, tongue, gums, cheeks), throat (pharynx), voice box (larynx), paranasal sinuses, nasal cavity, and salivary glands. Other types of cancers, such as those affecting the brain, eye, esophagus, thyroid gland, and head and neck skin, are not typically classified as head and neck cancers.
Risk factors for the head and neck cancer include tobacco use, alcohol abuse, and infection with oncogenic viruses like human papillomavirus (HPV) and Epstein-Barr virus. These cancers pose significant challenges in treatment and require a multidisciplinary approach that often involves surgery, radiotherapy, and systemic therapy. Early detection of head and neck cancer is important for improved outcomes, but it can be challenging due to vague and undifferentiated symptoms, leading to delayed referral to specialist services. Dental practitioners play a significant role in early diagnosis, as they have regular contact with patients and can identify red flag signs and symptoms, particularly in the oral cavity.
Epidemiology
Head and neck cancer is a significant health concern with increasing incidence rates globally, particularly oropharyngeal cancer. Several risk factors contribute to developing head and neck cancer, including tobacco smoking, alcohol consumption, betel chewing (in Southeast Asian individuals), and human papillomavirus (HPV) infection, especially in oropharyngeal cancer.
Disease Burden and Incidence:
Mortality:
Risk Factors:
Prevention and Recommendations:
Anatomy
Pathophysiology
The primary sites where head and neck cancers can form include the oral cavity (including the lips, tongue, gums, cheeks, floor of the mouth, and hard palate), throat (pharynx), sinuses, salivary glands, and muscles or nerves in the head and neck region.
The development of the head and neck squamous cell carcinomas (HNSCCs) is often associated with risk factors such as exposure to tobacco-derived carcinogens, excessive alcohol consumption, and infection with oncogenic strains of human papillomavirus (HPV), primarily HPV-16. Smoking is strongly associated with HNSCCs of the oral cavity and larynx, predominantly HPV-negative. HPV-positive HNSCCs, commonly found in the oropharynx, are primarily caused by HPV infection.
The pathophysiology of head and neck cancer involves various factors. Tobacco and alcohol use are the most common risk factors for the head and neck cancer, and they are likely synergistic in causing these cancers. Smokeless tobacco and cigar smoking are also associated with an enhanced risk of oral and pharyngeal cancers. Other potential environmental carcinogens, such as marijuana and occupational exposures to substances like nickel and textile fibers, may also contribute to developing head and neck cancer.
Etiology
The etiology of head and neck cancer involves various factors and risk factors. However, head and neck cancers can also originate from other areas, such as the salivary glands, sinuses, or muscles and nerves in the head and neck, although these are less common.
Several risk factors contribute to the development of head and neck cancer. The predominant risk factors include tobacco use and alcohol abuse. Both smoking and heavy alcohol consumption enhanced risk of developing head and neck cancer. Additionally, certain oncogenic viruses, such as human papillomavirus (HPV) and Epstein-Barr virus (EBV), are associated with an enhanced risk of developing head and neck cancer.
Tobacco use, including smoking cigarettes and smokeless tobacco, is a significant risk factor for head and neck cancer. The carcinogens present in tobacco can damage the DNA in cells lining the oral cavity and throat, leading to the development of cancer.
Alcohol abuse is another well-established risk factor for head and neck cancer. Heavy alcohol consumption can cause chronic irritation and inflammation in the mucosal lining of the upper aerodigestive tract, increasing the risk of cancer development.
Genetics
Prognostic Factors
Prognostic factors are characteristics or variables that can help predict a disease’s likely outcome or prognosis. Several prognostic factors have been identified in the case of head and neck cancer. It’s important to note that the significance and impact of these factors can vary depending on the specific type and stage of head and neck cancer.
Tumor Stage:
The cancer stage, determined by the size of the tumor and its reach to nearby lymph nodes or distant organs, is one of the most important prognostic factors. Generally, earlier stages of cancer (lower tumor size and limited spread) have a better prognosis than advanced stages.
Location and Site:
The specific site where cancer originated within the head and neck can influence prognosis. For example, oral cavity cancers generally have better outcomes than cancers in the larynx or hypopharynx.
Lymph Node Involvement:
The presence/absence of cancer in regional lymph nodes is a significant prognostic factor. The spread of cancer to lymph nodes indicates a higher risk of recurrence and may impact treatment decisions.
Histological Grade:
The grade of the tumor, which describes the degree of abnormality and aggressiveness of cancer cells when viewed under a microscope, is an important prognostic factor. High-grade tumors tend to be more aggressive and have a worse prognosis than low-grade tumors.
Performance Status:
The overall health and functional status of the patient, as measured by performance status scales (e.g., Eastern Cooperative Oncology Group [ECOG] performance status), can influence prognosis. Patients with better performance status often have better treatment tolerance and outcomes.
HPV (Human Papillomavirus) Status:
In cases of oropharyngeal cancer, HPV infection can significantly impact prognosis. HPV-positive oropharyngeal cancers generally have a better prognosis compared to HPV-negative cases.
Patient Age and Gender:
Younger patients, generally those below 40, have better outcomes. Additionally, some studies have suggested that female patients with certain types of head and neck cancers may have better prognoses than males.
Smoking and Alcohol Use:
Tobacco smoking and heavy alcohol consumption are known risk factors for head and neck cancer. These habits can affect treatment response and overall prognosis.
Comorbidities:
Other medical conditions, such as diabetes, heart disease, or immune system disorders, can impact the prognosis and treatment options for head and neck cancer.
Clinical History
The clinical presentation of head and neck cancer might vary based on various factors like the age group, associated comorbidity or activity, and the acuity of presentation. Here’s a comprehensive reply based on the information provided:
Age Group: Head and neck cancer can affect individuals of any age group, but it is more commonly diagnosed in older adults, especially those above 40. However, it’s worth noting that there has been an observed increase in head and neck cancer incidence among younger individuals due to the rise in human papillomavirus (HPV)-related oropharyngeal cancers.
Associated Comorbidity or Activity: Patients with head and neck cancer often have a higher burden of comorbidities than the general population. Common comorbid conditions associated with head and neck cancer include cardiovascular disease, chronic obstructive pulmonary disease (COPD), diabetes, and alcohol and tobacco use. Comorbidity burden has been shown to impact survival outcomes in head and neck cancer patients.
The acuity of Presentation: The presentation of head and neck cancer can vary in terms of acuity. Some patients may present with early-stage disease, where the symptoms are relatively mild and localized. These symptoms can include a persistent sore throat, difficulty swallowing, voice changes, or a lump or swelling in the neck. On the other hand, some patients may present with more advanced disease, characterized by aggressive symptoms such as significant weight loss, severe pain, bleeding, and visible tumor growth in the affected area.
Physical Examination
Physical examination plays a crucial role in evaluating head and neck cancer. Here are some critical aspects of the physical examination for head and neck cancer:
Age group
Associated comorbidity
Associated activity
Acuity of presentation
Differential Diagnoses
Head and neck cancer can present with various symptoms and manifestations, and it is essential to consider a broad range of the differential diagnoses when evaluating patients with suspected head and neck malignancies.
Laboratory Studies
Imaging Studies
Procedures
Histologic Findings
Staging
Treatment Paradigm
Radiation therapy:
Radiation therapy can be used as the primary treatment for certain types of cancer, especially when the tumor is localized and surgery is not feasible. It can also be combined with surgery or chemotherapy in a multimodal treatment approach. The decision to use radiation therapy as part of the treatment plan depends on various factors, such as the type and stage of cancer, the location of the tumor, and the overall health of the patient.
External Beam Radiation Therapy: In this method, a machine called a linear accelerator directs a focused beam of high-energy radiation from outside the body towards the tumor. The radiation is carefully targeted to the tumor site, while minimizing exposure to surrounding healthy tissues. The treatment is typically delivered in multiple sessions over a period of several weeks, with each session lasting only a few minutes.
Brachytherapy: This form of radiation therapy involves placing a radioactive source directly into or near the tumor. The radioactive material may be inserted temporarily or permanently. Temporary brachytherapy involves placing a radioactive source temporarily within the body, usually using applicators or catheters. Permanent brachytherapy, on the other hand, involves implanting small radioactive seeds or pellets near the tumor, which gradually release radiation over time.
Surgery:
The extent of the surgical procedure depends on several factors such as the location, size, and stage of the tumor. The primary goal of surgery is to remove the tumor along with the nearby lymph nodes that may be affected.
The specific surgical approach will vary depending on the location of the tumor. For example, in cases of oral cavity or throat cancers, surgery may involve removing a portion of the affected tissue or even the entire affected organ, such as a part of the tongue or the larynx (voice box). In some cases, neck dissection may be performed to remove the lymph nodes in the neck that could potentially harbor cancer cells.
Chemotherapy:
In head and neck cancers, chemotherapy can be employed in different ways. Neoadjuvant chemotherapy refers to the administration of chemotherapy before surgery or radiation therapy. This approach aims to shrink the tumors and make them more manageable for subsequent treatments.
Adjuvant chemotherapy, on the other hand, is given after surgery or radiation therapy. It is used to eliminate any remaining cancer cells that may not have been eradicated by the initial treatment. Adjuvant chemotherapy helps reduce the risk of cancer recurrence.
Additionally, chemotherapy can be combined with radiation therapy, known as chemoradiation. This combined approach is often used for advanced or metastatic head and neck cancers. Chemoradiation can improve treatment outcomes by targeting cancer cells with both chemotherapy drugs and radiation, which enhances the chances of killing cancer cells and preventing their spread.
Targeted therapy:
Targeted therapy drugs specifically target molecules or pathways involved in the growth and spread of cancer cells. Genetic mutations or specific biomarkers present in the cancer cells can help determine the suitability of targeted therapy. It can be used alone or in combination with other treatments.
by Stage
by Modality
Chemotherapy
Radiation Therapy
Surgical Interventions
Hormone Therapy
Immunotherapy
Hyperthermia
Photodynamic Therapy
Stem Cell Transplant
Targeted Therapy
Palliative Care
occupational-and-environmental-exposures-as-non-pharmacological-therapy
Industrial Carcinogens:
Minimizing exposure to occupational hazards, such as asbestos, formaldehyde, and certain chemicals used in industries, can reduce the risk of developing head and neck cancer.
Radiation Exposure:
Limiting unnecessary exposure to radiation, such as excessive medical imaging scans, is important to reduce the potential risk of developing cancer.
prevention-and-cure-as-non-pharmacological-therapy
Tobacco and Alcohol:
Avoiding or reducing tobacco and alcohol use can significantly lower the risk of developing head and neck cancer. Smoking cessation programs and alcohol moderation are important preventive measures.
Healthy Diet:
Intake a balanced diet rich in fruits and vegetables may help diminish the risk of head and neck cancer. Certain dietary components, such as antioxidants and phytochemicals, have shown potential protective effects.
Human Papillomavirus (HPV):
HPV Vaccination: HPV infection is a significant risk factor for specific types of head and neck cancer. Vaccination against HPV can help prevent HPV-related head and neck cancers.
use-of-supportive-care-and-rehabilitation-as-non-pharmacological-therapy
Oral Hygiene:
Maintaining good oral hygiene is key for patients with head and neck cancer, as it helps prevent complications and improves quality of life.
Speech and Swallowing Therapy:
Rehabilitation programs focusing on speech and swallowing exercises can help patients regain or improve their ability to communicate and swallow.
Psychosocial Support:
Providing emotional and psychological support to patients and their families can help them cope with the challenges of head and neck cancer.
Use of Radiation Therapy and Surgery for the Management of Squamous Cell Carcinomas
Radiation therapy (RT) and surgical intervention yield comparable rates of local control and survival for numerous anatomical sites. The selection of the appropriate treatment approach is generally determined by factors such as the unique characteristics and demands of the site, the ease of surgical access to the tumor, and the anticipated functional outcomes and associated morbidity for each treatment modality.
Use of traditional surgical approaches for the management of squamous cell carcinomas
Traditional surgical methods involving skin incisions are commonly employed for the management of salivary and thyroid cancers, which are easily accessible. However, for other anatomical sites, minimally invasive techniques have emerged as effective alternatives. For instance, transoral laser microsurgery (TOLM) has enhanced transoral access for treating cancers of the larynx and hypopharynx, while transoral robotic surgery (TORS) has proven beneficial for oropharyngeal cancers, allowing for improved surgical access through the mouth.
Use of surgery, RT, or chemotherapy for Locoregionally advanced disease in managing squamous cell carcinomas
Locoregionally advanced (stage III/IV) squamous cell carcinoma of the head and neck carries a significant risk of both local recurrence and also distant metastases. To maximize the likelihood of long-term disease control, combined modality approaches that involve a combination of surgery, radiation therapy (RT), and/or chemotherapy are typically necessary. These comprehensive treatment strategies are aimed at addressing the primary tumor as well as any spread to the regional lymph nodes, with the objective of achieving optimal disease control and improving overall outcomes for patients.
Use of Reconstruction and rehabilitation in managing squamous cell carcinomas
The surgical removal of the mandible, palate, and larynx can give rise to challenges in managing the airway, mastication (chewing), deglutition (swallowing), speech, and cosmetic appearance. Additionally, radiation therapy (RT) and chemoradiotherapy can further compromise functional abilities.
These treatments can negatively impact the normal functioning of these structures, leading to difficulties in breathing, eating, swallowing, speaking, and overall aesthetic appearance.
Patients who are generally not suitable candidates for surgical intervention can explore prosthetic rehabilitation as an alternative option. In cases where there are defects in the hard palate or maxilla, custom-made obturator prostheses can be utilized to provide coverage and restoration.
These prostheses are specifically designed to address the anatomical deficiencies and help improve functions such as speech, swallowing, and overall oral health. Prosthetic rehabilitation offers a viable solution for patients who are unable to undergo surgical procedures and aims to enhance their quality of life and oral function.
Medication
In Combination with Radiation therapy, a Complete IV administration 1hr before radiation therapy :
400
mg/m^2
Intravenous (IV)
as the initial dose over 2hrs administered one week before initiating a course of radiation therapy, and the Maintenance dose is 250 mg per m2 IV over 1hr once a week for the duration of radiation therapy, 6-7 weeks
Concomitant therapy with irradiation :
80
mg/kg
Orally
once every three days
Future Trends
Head and neck cancer is a term used to describe a group of cancers that usually develop in the squamous cells lining the mucosal surfaces of the head and neck region. This includes the oral cavity (mouth), throat (pharynx), voice box (larynx), and the nasal cavity and sinuses. The most common type of head and neck cancer is squamous cell carcinoma. It can arise in various locations, including the oral cavity (lips, tongue, gums, cheeks), throat (pharynx), voice box (larynx), paranasal sinuses, nasal cavity, and salivary glands. Other types of cancers, such as those affecting the brain, eye, esophagus, thyroid gland, and head and neck skin, are not typically classified as head and neck cancers.
Risk factors for the head and neck cancer include tobacco use, alcohol abuse, and infection with oncogenic viruses like human papillomavirus (HPV) and Epstein-Barr virus. These cancers pose significant challenges in treatment and require a multidisciplinary approach that often involves surgery, radiotherapy, and systemic therapy. Early detection of head and neck cancer is important for improved outcomes, but it can be challenging due to vague and undifferentiated symptoms, leading to delayed referral to specialist services. Dental practitioners play a significant role in early diagnosis, as they have regular contact with patients and can identify red flag signs and symptoms, particularly in the oral cavity.
Head and neck cancer is a significant health concern with increasing incidence rates globally, particularly oropharyngeal cancer. Several risk factors contribute to developing head and neck cancer, including tobacco smoking, alcohol consumption, betel chewing (in Southeast Asian individuals), and human papillomavirus (HPV) infection, especially in oropharyngeal cancer.
Disease Burden and Incidence:
Mortality:
Risk Factors:
Prevention and Recommendations:
The primary sites where head and neck cancers can form include the oral cavity (including the lips, tongue, gums, cheeks, floor of the mouth, and hard palate), throat (pharynx), sinuses, salivary glands, and muscles or nerves in the head and neck region.
The development of the head and neck squamous cell carcinomas (HNSCCs) is often associated with risk factors such as exposure to tobacco-derived carcinogens, excessive alcohol consumption, and infection with oncogenic strains of human papillomavirus (HPV), primarily HPV-16. Smoking is strongly associated with HNSCCs of the oral cavity and larynx, predominantly HPV-negative. HPV-positive HNSCCs, commonly found in the oropharynx, are primarily caused by HPV infection.
The pathophysiology of head and neck cancer involves various factors. Tobacco and alcohol use are the most common risk factors for the head and neck cancer, and they are likely synergistic in causing these cancers. Smokeless tobacco and cigar smoking are also associated with an enhanced risk of oral and pharyngeal cancers. Other potential environmental carcinogens, such as marijuana and occupational exposures to substances like nickel and textile fibers, may also contribute to developing head and neck cancer.
The etiology of head and neck cancer involves various factors and risk factors. However, head and neck cancers can also originate from other areas, such as the salivary glands, sinuses, or muscles and nerves in the head and neck, although these are less common.
Several risk factors contribute to the development of head and neck cancer. The predominant risk factors include tobacco use and alcohol abuse. Both smoking and heavy alcohol consumption enhanced risk of developing head and neck cancer. Additionally, certain oncogenic viruses, such as human papillomavirus (HPV) and Epstein-Barr virus (EBV), are associated with an enhanced risk of developing head and neck cancer.
Tobacco use, including smoking cigarettes and smokeless tobacco, is a significant risk factor for head and neck cancer. The carcinogens present in tobacco can damage the DNA in cells lining the oral cavity and throat, leading to the development of cancer.
Alcohol abuse is another well-established risk factor for head and neck cancer. Heavy alcohol consumption can cause chronic irritation and inflammation in the mucosal lining of the upper aerodigestive tract, increasing the risk of cancer development.
Prognostic factors are characteristics or variables that can help predict a disease’s likely outcome or prognosis. Several prognostic factors have been identified in the case of head and neck cancer. It’s important to note that the significance and impact of these factors can vary depending on the specific type and stage of head and neck cancer.
Tumor Stage:
The cancer stage, determined by the size of the tumor and its reach to nearby lymph nodes or distant organs, is one of the most important prognostic factors. Generally, earlier stages of cancer (lower tumor size and limited spread) have a better prognosis than advanced stages.
Location and Site:
The specific site where cancer originated within the head and neck can influence prognosis. For example, oral cavity cancers generally have better outcomes than cancers in the larynx or hypopharynx.
Lymph Node Involvement:
The presence/absence of cancer in regional lymph nodes is a significant prognostic factor. The spread of cancer to lymph nodes indicates a higher risk of recurrence and may impact treatment decisions.
Histological Grade:
The grade of the tumor, which describes the degree of abnormality and aggressiveness of cancer cells when viewed under a microscope, is an important prognostic factor. High-grade tumors tend to be more aggressive and have a worse prognosis than low-grade tumors.
Performance Status:
The overall health and functional status of the patient, as measured by performance status scales (e.g., Eastern Cooperative Oncology Group [ECOG] performance status), can influence prognosis. Patients with better performance status often have better treatment tolerance and outcomes.
HPV (Human Papillomavirus) Status:
In cases of oropharyngeal cancer, HPV infection can significantly impact prognosis. HPV-positive oropharyngeal cancers generally have a better prognosis compared to HPV-negative cases.
Patient Age and Gender:
Younger patients, generally those below 40, have better outcomes. Additionally, some studies have suggested that female patients with certain types of head and neck cancers may have better prognoses than males.
Smoking and Alcohol Use:
Tobacco smoking and heavy alcohol consumption are known risk factors for head and neck cancer. These habits can affect treatment response and overall prognosis.
Comorbidities:
Other medical conditions, such as diabetes, heart disease, or immune system disorders, can impact the prognosis and treatment options for head and neck cancer.
The clinical presentation of head and neck cancer might vary based on various factors like the age group, associated comorbidity or activity, and the acuity of presentation. Here’s a comprehensive reply based on the information provided:
Age Group: Head and neck cancer can affect individuals of any age group, but it is more commonly diagnosed in older adults, especially those above 40. However, it’s worth noting that there has been an observed increase in head and neck cancer incidence among younger individuals due to the rise in human papillomavirus (HPV)-related oropharyngeal cancers.
Associated Comorbidity or Activity: Patients with head and neck cancer often have a higher burden of comorbidities than the general population. Common comorbid conditions associated with head and neck cancer include cardiovascular disease, chronic obstructive pulmonary disease (COPD), diabetes, and alcohol and tobacco use. Comorbidity burden has been shown to impact survival outcomes in head and neck cancer patients.
The acuity of Presentation: The presentation of head and neck cancer can vary in terms of acuity. Some patients may present with early-stage disease, where the symptoms are relatively mild and localized. These symptoms can include a persistent sore throat, difficulty swallowing, voice changes, or a lump or swelling in the neck. On the other hand, some patients may present with more advanced disease, characterized by aggressive symptoms such as significant weight loss, severe pain, bleeding, and visible tumor growth in the affected area.
Physical examination plays a crucial role in evaluating head and neck cancer. Here are some critical aspects of the physical examination for head and neck cancer:
Head and neck cancer can present with various symptoms and manifestations, and it is essential to consider a broad range of the differential diagnoses when evaluating patients with suspected head and neck malignancies.
Radiation therapy:
Radiation therapy can be used as the primary treatment for certain types of cancer, especially when the tumor is localized and surgery is not feasible. It can also be combined with surgery or chemotherapy in a multimodal treatment approach. The decision to use radiation therapy as part of the treatment plan depends on various factors, such as the type and stage of cancer, the location of the tumor, and the overall health of the patient.
External Beam Radiation Therapy: In this method, a machine called a linear accelerator directs a focused beam of high-energy radiation from outside the body towards the tumor. The radiation is carefully targeted to the tumor site, while minimizing exposure to surrounding healthy tissues. The treatment is typically delivered in multiple sessions over a period of several weeks, with each session lasting only a few minutes.
Brachytherapy: This form of radiation therapy involves placing a radioactive source directly into or near the tumor. The radioactive material may be inserted temporarily or permanently. Temporary brachytherapy involves placing a radioactive source temporarily within the body, usually using applicators or catheters. Permanent brachytherapy, on the other hand, involves implanting small radioactive seeds or pellets near the tumor, which gradually release radiation over time.
Surgery:
The extent of the surgical procedure depends on several factors such as the location, size, and stage of the tumor. The primary goal of surgery is to remove the tumor along with the nearby lymph nodes that may be affected.
The specific surgical approach will vary depending on the location of the tumor. For example, in cases of oral cavity or throat cancers, surgery may involve removing a portion of the affected tissue or even the entire affected organ, such as a part of the tongue or the larynx (voice box). In some cases, neck dissection may be performed to remove the lymph nodes in the neck that could potentially harbor cancer cells.
Chemotherapy:
In head and neck cancers, chemotherapy can be employed in different ways. Neoadjuvant chemotherapy refers to the administration of chemotherapy before surgery or radiation therapy. This approach aims to shrink the tumors and make them more manageable for subsequent treatments.
Adjuvant chemotherapy, on the other hand, is given after surgery or radiation therapy. It is used to eliminate any remaining cancer cells that may not have been eradicated by the initial treatment. Adjuvant chemotherapy helps reduce the risk of cancer recurrence.
Additionally, chemotherapy can be combined with radiation therapy, known as chemoradiation. This combined approach is often used for advanced or metastatic head and neck cancers. Chemoradiation can improve treatment outcomes by targeting cancer cells with both chemotherapy drugs and radiation, which enhances the chances of killing cancer cells and preventing their spread.
Targeted therapy:
Targeted therapy drugs specifically target molecules or pathways involved in the growth and spread of cancer cells. Genetic mutations or specific biomarkers present in the cancer cells can help determine the suitability of targeted therapy. It can be used alone or in combination with other treatments.
Oncology, Medical
Oncology, Other
Oncology, Radiation
Industrial Carcinogens:
Minimizing exposure to occupational hazards, such as asbestos, formaldehyde, and certain chemicals used in industries, can reduce the risk of developing head and neck cancer.
Radiation Exposure:
Limiting unnecessary exposure to radiation, such as excessive medical imaging scans, is important to reduce the potential risk of developing cancer.
Oncology, Medical
Oncology, Other
Oncology, Radiation
Tobacco and Alcohol:
Avoiding or reducing tobacco and alcohol use can significantly lower the risk of developing head and neck cancer. Smoking cessation programs and alcohol moderation are important preventive measures.
Healthy Diet:
Intake a balanced diet rich in fruits and vegetables may help diminish the risk of head and neck cancer. Certain dietary components, such as antioxidants and phytochemicals, have shown potential protective effects.
Human Papillomavirus (HPV):
HPV Vaccination: HPV infection is a significant risk factor for specific types of head and neck cancer. Vaccination against HPV can help prevent HPV-related head and neck cancers.
Oncology, Medical
Oncology, Other
Oncology, Radiation
Oral Hygiene:
Maintaining good oral hygiene is key for patients with head and neck cancer, as it helps prevent complications and improves quality of life.
Speech and Swallowing Therapy:
Rehabilitation programs focusing on speech and swallowing exercises can help patients regain or improve their ability to communicate and swallow.
Psychosocial Support:
Providing emotional and psychological support to patients and their families can help them cope with the challenges of head and neck cancer.
Oncology, Medical
Oncology, Other
Oncology, Radiation
Radiation therapy (RT) and surgical intervention yield comparable rates of local control and survival for numerous anatomical sites. The selection of the appropriate treatment approach is generally determined by factors such as the unique characteristics and demands of the site, the ease of surgical access to the tumor, and the anticipated functional outcomes and associated morbidity for each treatment modality.
Oncology, Medical
Oncology, Other
Oncology, Radiation
Traditional surgical methods involving skin incisions are commonly employed for the management of salivary and thyroid cancers, which are easily accessible. However, for other anatomical sites, minimally invasive techniques have emerged as effective alternatives. For instance, transoral laser microsurgery (TOLM) has enhanced transoral access for treating cancers of the larynx and hypopharynx, while transoral robotic surgery (TORS) has proven beneficial for oropharyngeal cancers, allowing for improved surgical access through the mouth.
Locoregionally advanced (stage III/IV) squamous cell carcinoma of the head and neck carries a significant risk of both local recurrence and also distant metastases. To maximize the likelihood of long-term disease control, combined modality approaches that involve a combination of surgery, radiation therapy (RT), and/or chemotherapy are typically necessary. These comprehensive treatment strategies are aimed at addressing the primary tumor as well as any spread to the regional lymph nodes, with the objective of achieving optimal disease control and improving overall outcomes for patients.
The surgical removal of the mandible, palate, and larynx can give rise to challenges in managing the airway, mastication (chewing), deglutition (swallowing), speech, and cosmetic appearance. Additionally, radiation therapy (RT) and chemoradiotherapy can further compromise functional abilities.
These treatments can negatively impact the normal functioning of these structures, leading to difficulties in breathing, eating, swallowing, speaking, and overall aesthetic appearance.
Patients who are generally not suitable candidates for surgical intervention can explore prosthetic rehabilitation as an alternative option. In cases where there are defects in the hard palate or maxilla, custom-made obturator prostheses can be utilized to provide coverage and restoration.
These prostheses are specifically designed to address the anatomical deficiencies and help improve functions such as speech, swallowing, and overall oral health. Prosthetic rehabilitation offers a viable solution for patients who are unable to undergo surgical procedures and aims to enhance their quality of life and oral function.
Head and neck cancer is a term used to describe a group of cancers that usually develop in the squamous cells lining the mucosal surfaces of the head and neck region. This includes the oral cavity (mouth), throat (pharynx), voice box (larynx), and the nasal cavity and sinuses. The most common type of head and neck cancer is squamous cell carcinoma. It can arise in various locations, including the oral cavity (lips, tongue, gums, cheeks), throat (pharynx), voice box (larynx), paranasal sinuses, nasal cavity, and salivary glands. Other types of cancers, such as those affecting the brain, eye, esophagus, thyroid gland, and head and neck skin, are not typically classified as head and neck cancers.
Risk factors for the head and neck cancer include tobacco use, alcohol abuse, and infection with oncogenic viruses like human papillomavirus (HPV) and Epstein-Barr virus. These cancers pose significant challenges in treatment and require a multidisciplinary approach that often involves surgery, radiotherapy, and systemic therapy. Early detection of head and neck cancer is important for improved outcomes, but it can be challenging due to vague and undifferentiated symptoms, leading to delayed referral to specialist services. Dental practitioners play a significant role in early diagnosis, as they have regular contact with patients and can identify red flag signs and symptoms, particularly in the oral cavity.
Head and neck cancer is a significant health concern with increasing incidence rates globally, particularly oropharyngeal cancer. Several risk factors contribute to developing head and neck cancer, including tobacco smoking, alcohol consumption, betel chewing (in Southeast Asian individuals), and human papillomavirus (HPV) infection, especially in oropharyngeal cancer.
Disease Burden and Incidence:
Mortality:
Risk Factors:
Prevention and Recommendations:
The primary sites where head and neck cancers can form include the oral cavity (including the lips, tongue, gums, cheeks, floor of the mouth, and hard palate), throat (pharynx), sinuses, salivary glands, and muscles or nerves in the head and neck region.
The development of the head and neck squamous cell carcinomas (HNSCCs) is often associated with risk factors such as exposure to tobacco-derived carcinogens, excessive alcohol consumption, and infection with oncogenic strains of human papillomavirus (HPV), primarily HPV-16. Smoking is strongly associated with HNSCCs of the oral cavity and larynx, predominantly HPV-negative. HPV-positive HNSCCs, commonly found in the oropharynx, are primarily caused by HPV infection.
The pathophysiology of head and neck cancer involves various factors. Tobacco and alcohol use are the most common risk factors for the head and neck cancer, and they are likely synergistic in causing these cancers. Smokeless tobacco and cigar smoking are also associated with an enhanced risk of oral and pharyngeal cancers. Other potential environmental carcinogens, such as marijuana and occupational exposures to substances like nickel and textile fibers, may also contribute to developing head and neck cancer.
The etiology of head and neck cancer involves various factors and risk factors. However, head and neck cancers can also originate from other areas, such as the salivary glands, sinuses, or muscles and nerves in the head and neck, although these are less common.
Several risk factors contribute to the development of head and neck cancer. The predominant risk factors include tobacco use and alcohol abuse. Both smoking and heavy alcohol consumption enhanced risk of developing head and neck cancer. Additionally, certain oncogenic viruses, such as human papillomavirus (HPV) and Epstein-Barr virus (EBV), are associated with an enhanced risk of developing head and neck cancer.
Tobacco use, including smoking cigarettes and smokeless tobacco, is a significant risk factor for head and neck cancer. The carcinogens present in tobacco can damage the DNA in cells lining the oral cavity and throat, leading to the development of cancer.
Alcohol abuse is another well-established risk factor for head and neck cancer. Heavy alcohol consumption can cause chronic irritation and inflammation in the mucosal lining of the upper aerodigestive tract, increasing the risk of cancer development.
Prognostic factors are characteristics or variables that can help predict a disease’s likely outcome or prognosis. Several prognostic factors have been identified in the case of head and neck cancer. It’s important to note that the significance and impact of these factors can vary depending on the specific type and stage of head and neck cancer.
Tumor Stage:
The cancer stage, determined by the size of the tumor and its reach to nearby lymph nodes or distant organs, is one of the most important prognostic factors. Generally, earlier stages of cancer (lower tumor size and limited spread) have a better prognosis than advanced stages.
Location and Site:
The specific site where cancer originated within the head and neck can influence prognosis. For example, oral cavity cancers generally have better outcomes than cancers in the larynx or hypopharynx.
Lymph Node Involvement:
The presence/absence of cancer in regional lymph nodes is a significant prognostic factor. The spread of cancer to lymph nodes indicates a higher risk of recurrence and may impact treatment decisions.
Histological Grade:
The grade of the tumor, which describes the degree of abnormality and aggressiveness of cancer cells when viewed under a microscope, is an important prognostic factor. High-grade tumors tend to be more aggressive and have a worse prognosis than low-grade tumors.
Performance Status:
The overall health and functional status of the patient, as measured by performance status scales (e.g., Eastern Cooperative Oncology Group [ECOG] performance status), can influence prognosis. Patients with better performance status often have better treatment tolerance and outcomes.
HPV (Human Papillomavirus) Status:
In cases of oropharyngeal cancer, HPV infection can significantly impact prognosis. HPV-positive oropharyngeal cancers generally have a better prognosis compared to HPV-negative cases.
Patient Age and Gender:
Younger patients, generally those below 40, have better outcomes. Additionally, some studies have suggested that female patients with certain types of head and neck cancers may have better prognoses than males.
Smoking and Alcohol Use:
Tobacco smoking and heavy alcohol consumption are known risk factors for head and neck cancer. These habits can affect treatment response and overall prognosis.
Comorbidities:
Other medical conditions, such as diabetes, heart disease, or immune system disorders, can impact the prognosis and treatment options for head and neck cancer.
The clinical presentation of head and neck cancer might vary based on various factors like the age group, associated comorbidity or activity, and the acuity of presentation. Here’s a comprehensive reply based on the information provided:
Age Group: Head and neck cancer can affect individuals of any age group, but it is more commonly diagnosed in older adults, especially those above 40. However, it’s worth noting that there has been an observed increase in head and neck cancer incidence among younger individuals due to the rise in human papillomavirus (HPV)-related oropharyngeal cancers.
Associated Comorbidity or Activity: Patients with head and neck cancer often have a higher burden of comorbidities than the general population. Common comorbid conditions associated with head and neck cancer include cardiovascular disease, chronic obstructive pulmonary disease (COPD), diabetes, and alcohol and tobacco use. Comorbidity burden has been shown to impact survival outcomes in head and neck cancer patients.
The acuity of Presentation: The presentation of head and neck cancer can vary in terms of acuity. Some patients may present with early-stage disease, where the symptoms are relatively mild and localized. These symptoms can include a persistent sore throat, difficulty swallowing, voice changes, or a lump or swelling in the neck. On the other hand, some patients may present with more advanced disease, characterized by aggressive symptoms such as significant weight loss, severe pain, bleeding, and visible tumor growth in the affected area.
Physical examination plays a crucial role in evaluating head and neck cancer. Here are some critical aspects of the physical examination for head and neck cancer:
Head and neck cancer can present with various symptoms and manifestations, and it is essential to consider a broad range of the differential diagnoses when evaluating patients with suspected head and neck malignancies.
Radiation therapy:
Radiation therapy can be used as the primary treatment for certain types of cancer, especially when the tumor is localized and surgery is not feasible. It can also be combined with surgery or chemotherapy in a multimodal treatment approach. The decision to use radiation therapy as part of the treatment plan depends on various factors, such as the type and stage of cancer, the location of the tumor, and the overall health of the patient.
External Beam Radiation Therapy: In this method, a machine called a linear accelerator directs a focused beam of high-energy radiation from outside the body towards the tumor. The radiation is carefully targeted to the tumor site, while minimizing exposure to surrounding healthy tissues. The treatment is typically delivered in multiple sessions over a period of several weeks, with each session lasting only a few minutes.
Brachytherapy: This form of radiation therapy involves placing a radioactive source directly into or near the tumor. The radioactive material may be inserted temporarily or permanently. Temporary brachytherapy involves placing a radioactive source temporarily within the body, usually using applicators or catheters. Permanent brachytherapy, on the other hand, involves implanting small radioactive seeds or pellets near the tumor, which gradually release radiation over time.
Surgery:
The extent of the surgical procedure depends on several factors such as the location, size, and stage of the tumor. The primary goal of surgery is to remove the tumor along with the nearby lymph nodes that may be affected.
The specific surgical approach will vary depending on the location of the tumor. For example, in cases of oral cavity or throat cancers, surgery may involve removing a portion of the affected tissue or even the entire affected organ, such as a part of the tongue or the larynx (voice box). In some cases, neck dissection may be performed to remove the lymph nodes in the neck that could potentially harbor cancer cells.
Chemotherapy:
In head and neck cancers, chemotherapy can be employed in different ways. Neoadjuvant chemotherapy refers to the administration of chemotherapy before surgery or radiation therapy. This approach aims to shrink the tumors and make them more manageable for subsequent treatments.
Adjuvant chemotherapy, on the other hand, is given after surgery or radiation therapy. It is used to eliminate any remaining cancer cells that may not have been eradicated by the initial treatment. Adjuvant chemotherapy helps reduce the risk of cancer recurrence.
Additionally, chemotherapy can be combined with radiation therapy, known as chemoradiation. This combined approach is often used for advanced or metastatic head and neck cancers. Chemoradiation can improve treatment outcomes by targeting cancer cells with both chemotherapy drugs and radiation, which enhances the chances of killing cancer cells and preventing their spread.
Targeted therapy:
Targeted therapy drugs specifically target molecules or pathways involved in the growth and spread of cancer cells. Genetic mutations or specific biomarkers present in the cancer cells can help determine the suitability of targeted therapy. It can be used alone or in combination with other treatments.
Oncology, Medical
Oncology, Other
Oncology, Radiation
Industrial Carcinogens:
Minimizing exposure to occupational hazards, such as asbestos, formaldehyde, and certain chemicals used in industries, can reduce the risk of developing head and neck cancer.
Radiation Exposure:
Limiting unnecessary exposure to radiation, such as excessive medical imaging scans, is important to reduce the potential risk of developing cancer.
Oncology, Medical
Oncology, Other
Oncology, Radiation
Tobacco and Alcohol:
Avoiding or reducing tobacco and alcohol use can significantly lower the risk of developing head and neck cancer. Smoking cessation programs and alcohol moderation are important preventive measures.
Healthy Diet:
Intake a balanced diet rich in fruits and vegetables may help diminish the risk of head and neck cancer. Certain dietary components, such as antioxidants and phytochemicals, have shown potential protective effects.
Human Papillomavirus (HPV):
HPV Vaccination: HPV infection is a significant risk factor for specific types of head and neck cancer. Vaccination against HPV can help prevent HPV-related head and neck cancers.
Oncology, Medical
Oncology, Other
Oncology, Radiation
Oral Hygiene:
Maintaining good oral hygiene is key for patients with head and neck cancer, as it helps prevent complications and improves quality of life.
Speech and Swallowing Therapy:
Rehabilitation programs focusing on speech and swallowing exercises can help patients regain or improve their ability to communicate and swallow.
Psychosocial Support:
Providing emotional and psychological support to patients and their families can help them cope with the challenges of head and neck cancer.
Oncology, Medical
Oncology, Other
Oncology, Radiation
Radiation therapy (RT) and surgical intervention yield comparable rates of local control and survival for numerous anatomical sites. The selection of the appropriate treatment approach is generally determined by factors such as the unique characteristics and demands of the site, the ease of surgical access to the tumor, and the anticipated functional outcomes and associated morbidity for each treatment modality.
Oncology, Medical
Oncology, Other
Oncology, Radiation
Traditional surgical methods involving skin incisions are commonly employed for the management of salivary and thyroid cancers, which are easily accessible. However, for other anatomical sites, minimally invasive techniques have emerged as effective alternatives. For instance, transoral laser microsurgery (TOLM) has enhanced transoral access for treating cancers of the larynx and hypopharynx, while transoral robotic surgery (TORS) has proven beneficial for oropharyngeal cancers, allowing for improved surgical access through the mouth.
Locoregionally advanced (stage III/IV) squamous cell carcinoma of the head and neck carries a significant risk of both local recurrence and also distant metastases. To maximize the likelihood of long-term disease control, combined modality approaches that involve a combination of surgery, radiation therapy (RT), and/or chemotherapy are typically necessary. These comprehensive treatment strategies are aimed at addressing the primary tumor as well as any spread to the regional lymph nodes, with the objective of achieving optimal disease control and improving overall outcomes for patients.
The surgical removal of the mandible, palate, and larynx can give rise to challenges in managing the airway, mastication (chewing), deglutition (swallowing), speech, and cosmetic appearance. Additionally, radiation therapy (RT) and chemoradiotherapy can further compromise functional abilities.
These treatments can negatively impact the normal functioning of these structures, leading to difficulties in breathing, eating, swallowing, speaking, and overall aesthetic appearance.
Patients who are generally not suitable candidates for surgical intervention can explore prosthetic rehabilitation as an alternative option. In cases where there are defects in the hard palate or maxilla, custom-made obturator prostheses can be utilized to provide coverage and restoration.
These prostheses are specifically designed to address the anatomical deficiencies and help improve functions such as speech, swallowing, and overall oral health. Prosthetic rehabilitation offers a viable solution for patients who are unable to undergo surgical procedures and aims to enhance their quality of life and oral function.
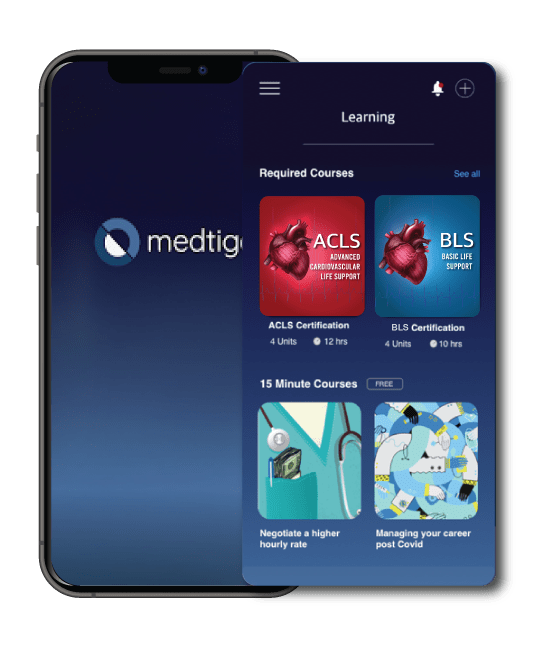
Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.
On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.
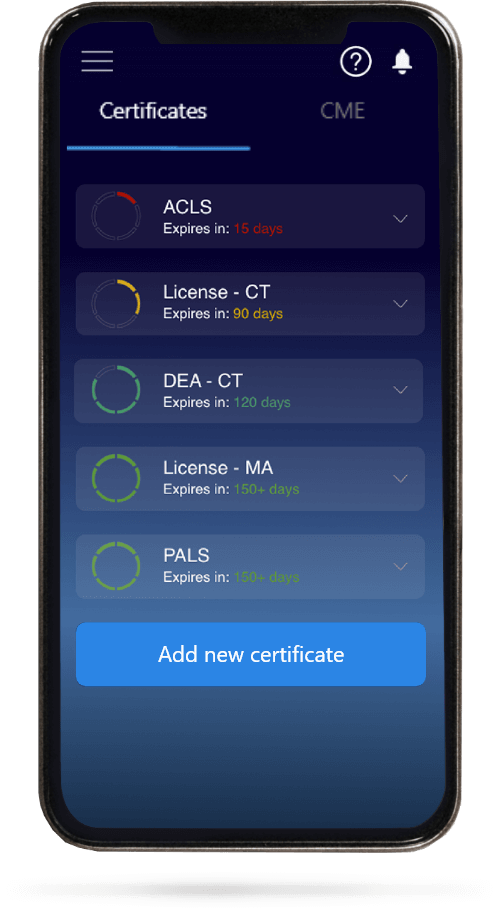
When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.