Can Extra Weekend Sleep Improve Glucose Health? What Researchers Found
March 4, 2026
Background
Herpes simplex keratitis is a frequent and potentially blinding disease characterized by recurrent corneal involvement with the herpes simplex virus (HSV). Currently, it is the leading cause of infectious corneal ulcers and blindness in the world. There are several types of herpes simplex virus, out of which, the two common types that affect humans are the HSV-1 and HSV-2; HSV-1 is normally present in the oral, labial and ocular region, whereas HSV-2 affects genital region. Primary infection with HSV occurs through contact with mucocutaneous surfaces, a time which the virus may not be evident. Primary infection of HSV occurs, and the virus is transported to the dorsal root ganglia, although it may later become active and recur as subsequent infections in the same dermatome.
HSK can occur as the initial episode of ocular herpes simplex virus or as recurrent episode. After the primary infection in the eye, further infection develops in the eye and, through the trigeminal nerve to the trigeminal ganglion. This gets activated by the virus bringing it back to the cornea, in this case leading to inflammation of the structures of the eye such as the conjunctiva, cornea, the front chamber of the eye, the iris, the lens, vitreous body and the retina.
Epidemiology
Anatomy
Pathophysiology
HSV belongs to DNA virus and is easily transmitted among people mainly through close contact with lesions or secretions which contain the viruses. Oral – ocular disease is normally esteemed due to HSV-1 while genital disease is normally esteemed because of HSV-2. However, HSV-2 can also cause ocular infection through direct mouth to genital contact, and it can also be transmitted through genital HSV-2 infected mothers during delivery.
First episodes of HSV-1 are usually seen in mucocutaneous form of trigeminal nerve which may appear like a viral pharyngitis. Subsequently, the virus invades epithelial cells and moves up to neural ganglia via nerve axons to get residing in the trigeminal ganglion. This implies that subsequent ocular disease can occur in an individual without having to have a primary ocular HSV infection.
Recurrent ocular HSV has classically been described to originate from reactivation in the trigeminal ganglion, with the virus spreading towards the ocular tissues through the nerve axons, resulting in a lytic infection.
Etiology
The causes of various manifestations of HSV keratitis are as follows:
Genetics
Prognostic Factors
Like most herpes viral infections, the prognosis for HSV keratitis is usually favorable if the disease is adequately managed. Small and simple dendritic ulcers do not need treatment and usually heal within a few days. Localized infection with the yeast can be easily treated with two weeks topical antifungal agents sometimes with local curettage as needed. Yet, epithelial or disciform keratitis lasting for a long time ends with scarring, vascularization, and in some cases, the loss of vision’s acuity.
Clinical History
Age Groups Affected
Children: Often seen with first episode herpes gingiva stomatitis and ocular lesions can result from auto inoculation.
Adults: Mainly involving recurrent herpes simplex keratitis in the third and fifth decades of the affected person’s life.
Physical Examination
Age group
Associated comorbidity
Associated activity
Acuity of presentation
Differential Diagnoses
Laboratory Studies
Imaging Studies
Procedures
Histologic Findings
Staging
Treatment Paradigm
Antiviral Therapy:
Topical Antivirals: Application of trifluridine or ganciclovir gel immediately after day of the procedure to reduce the viral shedding and replication in the corneal tissue.
Systemic Antivirals: For severe or recurrent forms systemic antiviral such as acyclovir, valacyclovir or famciclovir may be prescribed and incorporated in topical preparations.
Corticosteroids:
Topical Corticosteroids: When administered orally after the viruses are replication to calm the inflammation which may cause sclerosis formation.
Systemic Corticosteroids: Given in high doses and only for the severe patients because of the possible boost in the rate of replication of the virus.
Supportive Therapy:
Artificial Tears: For application of lubricants to decrease the manifestations of dryness and to treat the corneal epithelial diseases.
Pain Management: Use of non–steroidal anti-inflammatory drugs or applying something cold on the pain and swelling.
Procedural Interventions:
Debridement: Debridement to enhance the likelihood of antiviral effectiveness, because dead tissues or invasive pathogens need to be removed.
Surgical Options: In a worst-case scenario where the scarring has become severe, or the structures have been perforated, further action entails the use of the amniotic membrane transplantation or therapeutic keratoplasty.
Long-term Management:
Suppressive Therapy: They may make decisions for long-term oral antiviral therapy for episodes and manage to keep corneal clarity.
Monitoring and Follow-up: More follow ups for recovery, review vision and to monitor any side effects.
by Stage
by Modality
Chemotherapy
Radiation Therapy
Surgical Interventions
Hormone Therapy
Immunotherapy
Hyperthermia
Photodynamic Therapy
Stem Cell Transplant
Targeted Therapy
Palliative Care
use-of-a-non-pharmacological-approach-for-treating-herpes-simplex-keratitis
Cold Compresses: In cases where the closure of eyelids is possible, cooling with ice packs may be helpful in reducing congestion, as well as for providing symptomatic relief in the early stages.
Eye Hygiene: Stress proper handling and cleaning of the eyes pointing out that attempting to remove crusting by rubbing or using harsh soap can worsen the situation and lead to secondary bacterial infection.
Artificial Tears: The application of preservative-free artificial tears can help to reduce dryness and sustain appropriate lubrication on the corneal abrasion, therefore promoting epithelial cell regeneration.
UV Protection: Counsel the patient to use protective eyewear such as sunglasses while in the sun as UV light can bring on the virus.
Avoidance of Triggers: Inform the patient the following: Common trigger factors are stress, exposure to sunlight, and from contact lenses if any should avoid it.
Role of Anti-viral agents
use-of-intervention-with-a-procedure-in-treating-herpes-simplex-keratitis
use-of-phases-in-managing-herpes-simplex-keratitis
The overall approach to the management of herpes simplex keratitis is therefore divided into various subphases for optimum therapy and prevention of recurrence.
First, during the acute stage, the choice of an antiviral agent such as trifluridine or ganciclovir in the form of gel is clearly required to prevent the replication of the virus and reduce the manifestations of the disease. The following steps include assessment of the client’s reaction to the treatment, changes in the therapy plan, and supportive care that could involve eye irrigation and application of artificial tears.
The chronic or recurrent cases may necessitate the long-term low dose oral antiviral therapy to minimize the flare ups and careful observation for complications such as corneal scarring. In all phases of management, patient education on factors causing flares and compliance with treatment can be very helpful in improving the overall quality of life of the patient with this chronic viral ailment to the eyes.
Medication
Administer 0.1% solution one drop into the affected eye
Gradually reduce the frequency to every six hours a day or every two hours a day
Maintain this treatment regimen for a minimum of seven days
Administer dose of 50 mg/kg of body weight daily
Take dose of 1 gram four times a day for one to two weeks
Future Trends
References
Herpes simplex keratitis is a frequent and potentially blinding disease characterized by recurrent corneal involvement with the herpes simplex virus (HSV). Currently, it is the leading cause of infectious corneal ulcers and blindness in the world. There are several types of herpes simplex virus, out of which, the two common types that affect humans are the HSV-1 and HSV-2; HSV-1 is normally present in the oral, labial and ocular region, whereas HSV-2 affects genital region. Primary infection with HSV occurs through contact with mucocutaneous surfaces, a time which the virus may not be evident. Primary infection of HSV occurs, and the virus is transported to the dorsal root ganglia, although it may later become active and recur as subsequent infections in the same dermatome.
HSK can occur as the initial episode of ocular herpes simplex virus or as recurrent episode. After the primary infection in the eye, further infection develops in the eye and, through the trigeminal nerve to the trigeminal ganglion. This gets activated by the virus bringing it back to the cornea, in this case leading to inflammation of the structures of the eye such as the conjunctiva, cornea, the front chamber of the eye, the iris, the lens, vitreous body and the retina.
HSV belongs to DNA virus and is easily transmitted among people mainly through close contact with lesions or secretions which contain the viruses. Oral – ocular disease is normally esteemed due to HSV-1 while genital disease is normally esteemed because of HSV-2. However, HSV-2 can also cause ocular infection through direct mouth to genital contact, and it can also be transmitted through genital HSV-2 infected mothers during delivery.
First episodes of HSV-1 are usually seen in mucocutaneous form of trigeminal nerve which may appear like a viral pharyngitis. Subsequently, the virus invades epithelial cells and moves up to neural ganglia via nerve axons to get residing in the trigeminal ganglion. This implies that subsequent ocular disease can occur in an individual without having to have a primary ocular HSV infection.
Recurrent ocular HSV has classically been described to originate from reactivation in the trigeminal ganglion, with the virus spreading towards the ocular tissues through the nerve axons, resulting in a lytic infection.
The causes of various manifestations of HSV keratitis are as follows:
Like most herpes viral infections, the prognosis for HSV keratitis is usually favorable if the disease is adequately managed. Small and simple dendritic ulcers do not need treatment and usually heal within a few days. Localized infection with the yeast can be easily treated with two weeks topical antifungal agents sometimes with local curettage as needed. Yet, epithelial or disciform keratitis lasting for a long time ends with scarring, vascularization, and in some cases, the loss of vision’s acuity.
Age Groups Affected
Children: Often seen with first episode herpes gingiva stomatitis and ocular lesions can result from auto inoculation.
Adults: Mainly involving recurrent herpes simplex keratitis in the third and fifth decades of the affected person’s life.
Antiviral Therapy:
Topical Antivirals: Application of trifluridine or ganciclovir gel immediately after day of the procedure to reduce the viral shedding and replication in the corneal tissue.
Systemic Antivirals: For severe or recurrent forms systemic antiviral such as acyclovir, valacyclovir or famciclovir may be prescribed and incorporated in topical preparations.
Corticosteroids:
Topical Corticosteroids: When administered orally after the viruses are replication to calm the inflammation which may cause sclerosis formation.
Systemic Corticosteroids: Given in high doses and only for the severe patients because of the possible boost in the rate of replication of the virus.
Supportive Therapy:
Artificial Tears: For application of lubricants to decrease the manifestations of dryness and to treat the corneal epithelial diseases.
Pain Management: Use of non–steroidal anti-inflammatory drugs or applying something cold on the pain and swelling.
Procedural Interventions:
Debridement: Debridement to enhance the likelihood of antiviral effectiveness, because dead tissues or invasive pathogens need to be removed.
Surgical Options: In a worst-case scenario where the scarring has become severe, or the structures have been perforated, further action entails the use of the amniotic membrane transplantation or therapeutic keratoplasty.
Long-term Management:
Suppressive Therapy: They may make decisions for long-term oral antiviral therapy for episodes and manage to keep corneal clarity.
Monitoring and Follow-up: More follow ups for recovery, review vision and to monitor any side effects.
Ophthalmology
Cold Compresses: In cases where the closure of eyelids is possible, cooling with ice packs may be helpful in reducing congestion, as well as for providing symptomatic relief in the early stages.
Eye Hygiene: Stress proper handling and cleaning of the eyes pointing out that attempting to remove crusting by rubbing or using harsh soap can worsen the situation and lead to secondary bacterial infection.
Artificial Tears: The application of preservative-free artificial tears can help to reduce dryness and sustain appropriate lubrication on the corneal abrasion, therefore promoting epithelial cell regeneration.
UV Protection: Counsel the patient to use protective eyewear such as sunglasses while in the sun as UV light can bring on the virus.
Avoidance of Triggers: Inform the patient the following: Common trigger factors are stress, exposure to sunlight, and from contact lenses if any should avoid it.
Ophthalmology
Ophthalmology
Ophthalmology
The overall approach to the management of herpes simplex keratitis is therefore divided into various subphases for optimum therapy and prevention of recurrence.
First, during the acute stage, the choice of an antiviral agent such as trifluridine or ganciclovir in the form of gel is clearly required to prevent the replication of the virus and reduce the manifestations of the disease. The following steps include assessment of the client’s reaction to the treatment, changes in the therapy plan, and supportive care that could involve eye irrigation and application of artificial tears.
The chronic or recurrent cases may necessitate the long-term low dose oral antiviral therapy to minimize the flare ups and careful observation for complications such as corneal scarring. In all phases of management, patient education on factors causing flares and compliance with treatment can be very helpful in improving the overall quality of life of the patient with this chronic viral ailment to the eyes.
Herpes simplex keratitis is a frequent and potentially blinding disease characterized by recurrent corneal involvement with the herpes simplex virus (HSV). Currently, it is the leading cause of infectious corneal ulcers and blindness in the world. There are several types of herpes simplex virus, out of which, the two common types that affect humans are the HSV-1 and HSV-2; HSV-1 is normally present in the oral, labial and ocular region, whereas HSV-2 affects genital region. Primary infection with HSV occurs through contact with mucocutaneous surfaces, a time which the virus may not be evident. Primary infection of HSV occurs, and the virus is transported to the dorsal root ganglia, although it may later become active and recur as subsequent infections in the same dermatome.
HSK can occur as the initial episode of ocular herpes simplex virus or as recurrent episode. After the primary infection in the eye, further infection develops in the eye and, through the trigeminal nerve to the trigeminal ganglion. This gets activated by the virus bringing it back to the cornea, in this case leading to inflammation of the structures of the eye such as the conjunctiva, cornea, the front chamber of the eye, the iris, the lens, vitreous body and the retina.
HSV belongs to DNA virus and is easily transmitted among people mainly through close contact with lesions or secretions which contain the viruses. Oral – ocular disease is normally esteemed due to HSV-1 while genital disease is normally esteemed because of HSV-2. However, HSV-2 can also cause ocular infection through direct mouth to genital contact, and it can also be transmitted through genital HSV-2 infected mothers during delivery.
First episodes of HSV-1 are usually seen in mucocutaneous form of trigeminal nerve which may appear like a viral pharyngitis. Subsequently, the virus invades epithelial cells and moves up to neural ganglia via nerve axons to get residing in the trigeminal ganglion. This implies that subsequent ocular disease can occur in an individual without having to have a primary ocular HSV infection.
Recurrent ocular HSV has classically been described to originate from reactivation in the trigeminal ganglion, with the virus spreading towards the ocular tissues through the nerve axons, resulting in a lytic infection.
The causes of various manifestations of HSV keratitis are as follows:
Like most herpes viral infections, the prognosis for HSV keratitis is usually favorable if the disease is adequately managed. Small and simple dendritic ulcers do not need treatment and usually heal within a few days. Localized infection with the yeast can be easily treated with two weeks topical antifungal agents sometimes with local curettage as needed. Yet, epithelial or disciform keratitis lasting for a long time ends with scarring, vascularization, and in some cases, the loss of vision’s acuity.
Age Groups Affected
Children: Often seen with first episode herpes gingiva stomatitis and ocular lesions can result from auto inoculation.
Adults: Mainly involving recurrent herpes simplex keratitis in the third and fifth decades of the affected person’s life.
Antiviral Therapy:
Topical Antivirals: Application of trifluridine or ganciclovir gel immediately after day of the procedure to reduce the viral shedding and replication in the corneal tissue.
Systemic Antivirals: For severe or recurrent forms systemic antiviral such as acyclovir, valacyclovir or famciclovir may be prescribed and incorporated in topical preparations.
Corticosteroids:
Topical Corticosteroids: When administered orally after the viruses are replication to calm the inflammation which may cause sclerosis formation.
Systemic Corticosteroids: Given in high doses and only for the severe patients because of the possible boost in the rate of replication of the virus.
Supportive Therapy:
Artificial Tears: For application of lubricants to decrease the manifestations of dryness and to treat the corneal epithelial diseases.
Pain Management: Use of non–steroidal anti-inflammatory drugs or applying something cold on the pain and swelling.
Procedural Interventions:
Debridement: Debridement to enhance the likelihood of antiviral effectiveness, because dead tissues or invasive pathogens need to be removed.
Surgical Options: In a worst-case scenario where the scarring has become severe, or the structures have been perforated, further action entails the use of the amniotic membrane transplantation or therapeutic keratoplasty.
Long-term Management:
Suppressive Therapy: They may make decisions for long-term oral antiviral therapy for episodes and manage to keep corneal clarity.
Monitoring and Follow-up: More follow ups for recovery, review vision and to monitor any side effects.
Ophthalmology
Cold Compresses: In cases where the closure of eyelids is possible, cooling with ice packs may be helpful in reducing congestion, as well as for providing symptomatic relief in the early stages.
Eye Hygiene: Stress proper handling and cleaning of the eyes pointing out that attempting to remove crusting by rubbing or using harsh soap can worsen the situation and lead to secondary bacterial infection.
Artificial Tears: The application of preservative-free artificial tears can help to reduce dryness and sustain appropriate lubrication on the corneal abrasion, therefore promoting epithelial cell regeneration.
UV Protection: Counsel the patient to use protective eyewear such as sunglasses while in the sun as UV light can bring on the virus.
Avoidance of Triggers: Inform the patient the following: Common trigger factors are stress, exposure to sunlight, and from contact lenses if any should avoid it.
Ophthalmology
Ophthalmology
Ophthalmology
The overall approach to the management of herpes simplex keratitis is therefore divided into various subphases for optimum therapy and prevention of recurrence.
First, during the acute stage, the choice of an antiviral agent such as trifluridine or ganciclovir in the form of gel is clearly required to prevent the replication of the virus and reduce the manifestations of the disease. The following steps include assessment of the client’s reaction to the treatment, changes in the therapy plan, and supportive care that could involve eye irrigation and application of artificial tears.
The chronic or recurrent cases may necessitate the long-term low dose oral antiviral therapy to minimize the flare ups and careful observation for complications such as corneal scarring. In all phases of management, patient education on factors causing flares and compliance with treatment can be very helpful in improving the overall quality of life of the patient with this chronic viral ailment to the eyes.
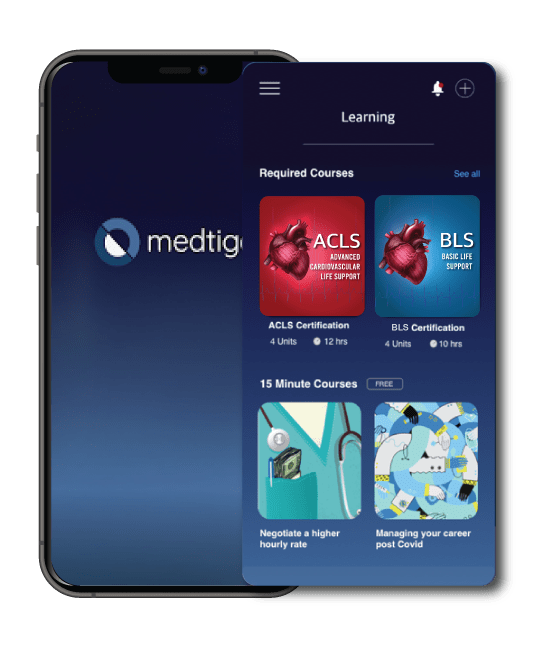
Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.
On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.
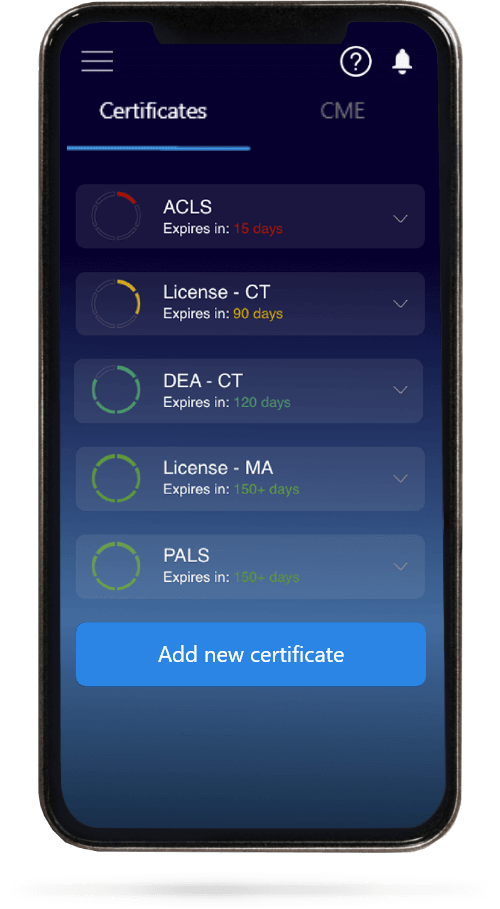
When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.