Sleepless and Costly: How OSA Is Hitting US and UK Workforces
March 3, 2026
Background
Having low hemoglobin levels defines anemia. Lacking iron usually causes this condition. Iron is a key ingredient of hemoglobin. Deficient iron commonly makes red blood cells tiny and pale. It’s the world’s most widespread anemia trigger. Various factors dictate iron shortage’s origin, like person’s age, gender, background. Folks may feel constantly tired or breathless, particularly with effort. Fixing the core problem treats anemia, with iron pills typically prescribed. But sometimes, IV iron doses are needed. Untreated, iron anemia lengthens hospital stays and worsens health outcomes.
Epidemiology
Anemia: a common illness found in around a fourth of people worldwide. Iron deficiency causes half of all anemia cases. It’s the top reason. For American men under 50, only 1% have iron deficiency anemia. But in developing countries, the rates are higher. About 10% of women of childbearing age in the U.S. experience iron deficiency anemia. This is mostly due to menstrual bleeding. For children aged 12 to 36 months, 9% have iron deficiency. One-third of these kids develop anemia. Though overall iron deficiency anemia rates are low in the U.S., low-income families face a higher risk.
Anatomy
Pathophysiology
Iron deficiency makes people have microcytic hypochromic anemia. This means they lack healthy red blood cells. Iron is needed to make hemoglobin. Hemoglobin carries oxygen in red blood cells throughout the body. Without enough iron, hemoglobin can’t be produced well. Then, organs and tissues don’t get enough oxygen. This causes anemia symptoms. Iron deficiency anemia can happen for many reasons. Not eating enough iron-rich foods is one cause. Losing blood is another cause. Trouble absorbing iron can also cause it. Bleeding gums may contribute to iron deficiency anemia. In adults over 50, bleeding in the digestive system and iron deficiency anemia could mean cancer. But sometimes the cause is unknown. Celiac disease or inflammatory bowel disease can also lead to iron deficiency anemia. Pregnancy, periods, or growth spurts in kids increase iron needs too. The American Academy of Pediatrics says to give iron supplements for iron deficiency. The amount depends on age and nutrition.
Etiology
Iron deficiency anemia has different reasons behind it. It depends on things like a person’s age, if they’re male or female, and how well off they are. It can happen because you don’t get enough iron in your diet. Or your body might not absorb iron properly. Blood loss is also a big factor, especially in older adults. Pregnancy increases the body’s need for iron, which can lead to this condition. Some diseases like celiac disease stop iron from being absorbed right. For babies, breastmilk gives them iron that’s easier for their bodies to use compared to cow’s milk. That helps prevent iron deficiency.
Genetics
Prognostic Factors
Patients mostly have a good outlook in the short term. However, if the root problem persists, their prognosis worsens. Iron shortage over time may cause lung or heart issues. This can be fatal.
Clinical History
Physical Examination
Age group
Associated comorbidity
Associated activity
Acuity of presentation
Differential Diagnoses
Laboratory Studies
Imaging Studies
Procedures
Histologic Findings
Staging
Treatment Paradigm
Iron deficiency has several possible causes. Treatment depends on the root issue. It’s important to eat iron-rich foods like red meat, poultry, fish, beans, lentils, tofu, fortified cereals, and leafy greens. For mild to moderate iron deficiency anemia, taking oral iron supplements is usually the first treatment tried. But for severe anemia, iron intolerance, non-compliance, or insufficient oral supplement response, intravenous (IV) iron therapy may be an alternative option.
by Stage
by Modality
Chemotherapy
Radiation Therapy
Surgical Interventions
Hormone Therapy
Immunotherapy
Hyperthermia
Photodynamic Therapy
Stem Cell Transplant
Targeted Therapy
Palliative Care
use-of-non-pharmacological-approach-for-iron-deficiency-anemia
Public campaigns inform about iron-rich foods and balanced diets. This combats poor diet access. Better sanitation stops diseases, reducing iron deficiency anemia. Focus on women’s health during pregnancy and periods. Increased iron needs then. Control parasitic infections. They cause blood loss, worsening iron deficiency. Community iron supplements also help in high anemia areas. These improve iron levels and health results.
Use of Oral Iron Supplements
Iron supplements come in forms like Ferrous Sulfate, Gluconate, and Fumarate. The ferrous (Fe2+) iron gets absorbed better. Usually, people take them one to three times daily, between meals to boost absorption. Another type is Iron Polysaccharide Complex, which may be easier on the stomach for some folks who get side effects – it might be easier to tolerate.
Use of Intravenous (IV) Iron Preparations
Iron Dextran and Iron Sucrose: Iron Dextran and Iron Sucrose are IV formulations used when oral iron causes trouble. Doctors prescribe IV iron for severe iron deficiency anemia. It’s also suitable when the body struggles to absorb oral iron or oral iron is hard to tolerate.
use-of-intervention-with-a-procedure-in-treating-iron-deficiency-anemia
Giving iron intravenously, or IV, is an option when taking it by mouth is not enough or causes side effects. Direct iron delivery into the bloodstream helps. If anemia is severe or life-threatening, a blood transfusion may rapidly increase hemoglobin levels. This is needed in some cases. If bleeding in the digestive tract causes iron deficiency anemia, doctors may order endoscopic tests. These include gastroscopy and colonoscopy to find and treat the cause.
use-of-phases-in-managing-iron-deficiency-anemia
Medication
Prophylactic measure:60mg elemental iron every day
Treatment: 60mg elemental iron every 6-12 hours
Mineral/vitamin supplementation
Initial dose:48 to 144mg/day orally ferrous gluconate,1 to 3 times daily
Daily intake recommendation
Women: 18mg of elemental iron orally every day
Lactating women: 9mg elemental iron orally every day
Pregnant women: 27mg of elemental iron orally every day
Men: 8mg elemental iron orally every day
360 mg orally daily (120 mg/day Fe) for 3 months
Take a dose of 50 mg orally three times daily
Prophylaxis of Iron Deficiency
Take daily dose of 300 mg orally
Administer dose of 25 to 100 mg intravenously
Not more than 100 mg/day
400 mg/5 ml given orally for premature infants. FAC mixture is usually given for 3 to 4 months after the discharge
tetraferric tricitrate decahydrate
with CKD not on dialysis
:
Initial dose: 210 mg (i.e., 1 tablet) orally 3 times a day with meals
Titrate when required to attain and maintain target haemoglobin levels
should not exceed more than 12 tablets a day
The average dosage in the clinical study was 5 tablets a day
100 - 200 mg is given as intravenous infusion
5ml consisting of 27.5mg of iron is given as oral solution. It can be increased gradually to 10ml thrice a day
Indicated in the management of iron deficiency anemia
The typical amount of elemental iron recommended for adults dealing with iron deficiency anemia ranges from 60 to 120 milligrams (mg) via oral administration per day. However, initial doses for addressing anemia can be as low as 15 milligrams of iron per day
The duration of the treatment will be for 6 to 8 weeks
Dose Adjustments
N/A
Indicated for the treatment of iron deficiency anemia
The usual dose recommended via oral administration is 1.5 to 2.0 mg/kg every 8 hours in a day
Duration: 6–8 weeks following the restoration to normal of the haemoglobin level and red cell indices
Note:Correction of haemoglobin level and replenishment of bodily iron reserves are the two main objectives of iron deficiency therapy
Dose Adjustments
N/A
It is administered orally in the form of a solution or tablet.
Initial dosage of 600 mg per day for 3 months divided in 1 to 3 times a day
Wt: ≥50 kg
750 mg IV in two doses that are at least seven days apart;
Do not exceed cumulative dose of 1500 mg/course
Wt: <50 kg
15 mg/kg IV in two doses that are at least seven days apart
Note: Treatment for people with non-dialysis dependent chronic kidney disease who have iron deficiency anemia (IDA) and have an intolerance to or unsatisfactory response to oral iron
210 mg orally thrice daily with meals
Do not exceed 12 tablets per day
Wt < 50 kg: 20 mg/kg intravenous infusion
Wt > 50 kg: 1000 mg intravenous infusion
If iron deficiency anemia reappears, repeat the dosage.
Note: Indicated for people with iron deficiency anemia who are intolerant to oral iron or who have not responded satisfactorily to oral iron
Additionally recommended for persons with non-hemodialysis dependent chronic renal disease who have iron deficient anemia
125 mg Intravenous infusion for one hour; maximum of 250 mg per infusion for 8 hemodialysis episodes
You could dilute it in 100 mL of 0.9% NaCl and take it for an hour
Provide undiluted medicine, however you shouldn't give more than 12.5 mg per minute
Note: It is recommended for use in treating iron deficiency anemia in adults and children older than six years old who have chronic kidney disease, are getting hemodialysis, and are receiving additional epoetin therapy
Many patients may need to receive a cumulative dose of 1000 mg of elemental iron over the course of 8 dialysis sessions for repletion treatment
Age: ≥6 years
8 hemodialysis sessions with an IV injection of 1.5 mg/kg elemental Fe over 1 hour
No more than 125 mg/dose
Note: It is recommended for use in treating iron deficiency anemia in adults and children older than six years old who have chronic kidney disease, are getting hemodialysis, and are receiving additional epoetin therapy
30 mg orally twice daily
100-200 mg orally divided 2 times a day; extended-release form can be administered once daily
510 mg intravenously for 15 minutes
Administer the second dose 3-8 days later
100-200 mg orally divided 2 times a day; extended-release form can be administered once daily
Elemental iron prophylaxis
60 mg orally daily
100 - 200 mg is given as intravenous infusion
Prophylactic measure:1-2mg elemental iron/kg/day orally. Do not exceed 15mg/day
Treatment: 3-6mg elemental iron/kg/day orally
Daily intake recommendation
0-6 months:0.27mg elemental iron orally every day
7-12 months: 11mg elemental iron orally every day
1-3 years: 7mg elemental iron orally every day
4-8 years: 10mg elemental iron orally every day
9-1 years: 8mg elemental iron orally every day
14-18 years: 15 mg elemental iron orally every day (females)
11mg elemental iron orally every day (males)
3-6 mg /kg orally every Day
Prophylaxis, Iron-deficiency Anemia
1-2 mg/kg/day orally every Day
The maximum dose recommended a day is ≤15 mg
3-6 mg /kg orally every Day
Prophylaxis, Iron-deficiency Anemia
1-2 mg/kg/day orally every Day
The maximum dose recommended a day is ≤15 mg
Severe Iron Deficiency Anemia
Take a dose of 4 to 6 mg/kg orally divided every 8 hour
Mild to Moderate Iron Deficiency Anemia
Take daily dose of 3 mg/kg orally
Prophylaxis
Take a dose of 1 to 2 mg/kg orally and it should not be more than 15 mg orally
For >15 kg:
0.0442(Desired Hemoglobin - Observed Hemoglobin) x Lean body weight(kg) + (0.26 × Lean body weight)
For 5 to 15 kg:
Not used in starting four months of life
Dose = 0.0442(Desired Hemoglobin - Observed Hemoglobin) x body weight(kg) + (0.26 × body weight)
Indicated in the management of iron deficiency anemia
For toddlers, newborns, and kids up to 14 years old, the UL is 40 milligrams
Side effects from consuming chelated iron are more likely to happen if the UL is achieved in healthy individuals
The duration of the treatment will be for 6 to 8 weeks
Dose Adjustments
N/A
0 years to 5 years: 15 mg/kg to 30 mg/kg per day
5 years to 12 years: 300 mg per day
12 to 18 years males: 2 tablets of 300 mg per day orally
12 to 18 years females: 300 mg to 600 mg per day orally
Wt: ≥50 kg
750 mg IV in two doses that are at least seven days apart;
Do not exceed cumulative dose of 1500 mg/course
Wt: <50 kg
15 mg/kg IV in two doses that are at least seven days apart
Note: Treatment for people with non-dialysis dependent chronic kidney disease who have iron deficiency anaemia (IDA) and have an intolerance to or unsatisfactory response to oral iron
3-6 mg Fe/kg/day orally divided 3 times daily
Elemental iron prophylaxis
> 4month: 1 mg/kg orally daily
6 months-2 years: 2 mg/kg orally daily
2-5 years: 2 mg/kg orally daily
>5 years: 30 mg orally daily with folic acid
Adolescents: 60 mg orally daily with folic acid
Future Trends
Having low hemoglobin levels defines anemia. Lacking iron usually causes this condition. Iron is a key ingredient of hemoglobin. Deficient iron commonly makes red blood cells tiny and pale. It’s the world’s most widespread anemia trigger. Various factors dictate iron shortage’s origin, like person’s age, gender, background. Folks may feel constantly tired or breathless, particularly with effort. Fixing the core problem treats anemia, with iron pills typically prescribed. But sometimes, IV iron doses are needed. Untreated, iron anemia lengthens hospital stays and worsens health outcomes.
Anemia: a common illness found in around a fourth of people worldwide. Iron deficiency causes half of all anemia cases. It’s the top reason. For American men under 50, only 1% have iron deficiency anemia. But in developing countries, the rates are higher. About 10% of women of childbearing age in the U.S. experience iron deficiency anemia. This is mostly due to menstrual bleeding. For children aged 12 to 36 months, 9% have iron deficiency. One-third of these kids develop anemia. Though overall iron deficiency anemia rates are low in the U.S., low-income families face a higher risk.
Iron deficiency makes people have microcytic hypochromic anemia. This means they lack healthy red blood cells. Iron is needed to make hemoglobin. Hemoglobin carries oxygen in red blood cells throughout the body. Without enough iron, hemoglobin can’t be produced well. Then, organs and tissues don’t get enough oxygen. This causes anemia symptoms. Iron deficiency anemia can happen for many reasons. Not eating enough iron-rich foods is one cause. Losing blood is another cause. Trouble absorbing iron can also cause it. Bleeding gums may contribute to iron deficiency anemia. In adults over 50, bleeding in the digestive system and iron deficiency anemia could mean cancer. But sometimes the cause is unknown. Celiac disease or inflammatory bowel disease can also lead to iron deficiency anemia. Pregnancy, periods, or growth spurts in kids increase iron needs too. The American Academy of Pediatrics says to give iron supplements for iron deficiency. The amount depends on age and nutrition.
Iron deficiency anemia has different reasons behind it. It depends on things like a person’s age, if they’re male or female, and how well off they are. It can happen because you don’t get enough iron in your diet. Or your body might not absorb iron properly. Blood loss is also a big factor, especially in older adults. Pregnancy increases the body’s need for iron, which can lead to this condition. Some diseases like celiac disease stop iron from being absorbed right. For babies, breastmilk gives them iron that’s easier for their bodies to use compared to cow’s milk. That helps prevent iron deficiency.
Patients mostly have a good outlook in the short term. However, if the root problem persists, their prognosis worsens. Iron shortage over time may cause lung or heart issues. This can be fatal.
Iron deficiency has several possible causes. Treatment depends on the root issue. It’s important to eat iron-rich foods like red meat, poultry, fish, beans, lentils, tofu, fortified cereals, and leafy greens. For mild to moderate iron deficiency anemia, taking oral iron supplements is usually the first treatment tried. But for severe anemia, iron intolerance, non-compliance, or insufficient oral supplement response, intravenous (IV) iron therapy may be an alternative option.
Hematology
Public campaigns inform about iron-rich foods and balanced diets. This combats poor diet access. Better sanitation stops diseases, reducing iron deficiency anemia. Focus on women’s health during pregnancy and periods. Increased iron needs then. Control parasitic infections. They cause blood loss, worsening iron deficiency. Community iron supplements also help in high anemia areas. These improve iron levels and health results.
Hematology
Iron supplements come in forms like Ferrous Sulfate, Gluconate, and Fumarate. The ferrous (Fe2+) iron gets absorbed better. Usually, people take them one to three times daily, between meals to boost absorption. Another type is Iron Polysaccharide Complex, which may be easier on the stomach for some folks who get side effects – it might be easier to tolerate.
Hematology
Iron Dextran and Iron Sucrose: Iron Dextran and Iron Sucrose are IV formulations used when oral iron causes trouble. Doctors prescribe IV iron for severe iron deficiency anemia. It’s also suitable when the body struggles to absorb oral iron or oral iron is hard to tolerate.
Hematology
Giving iron intravenously, or IV, is an option when taking it by mouth is not enough or causes side effects. Direct iron delivery into the bloodstream helps. If anemia is severe or life-threatening, a blood transfusion may rapidly increase hemoglobin levels. This is needed in some cases. If bleeding in the digestive tract causes iron deficiency anemia, doctors may order endoscopic tests. These include gastroscopy and colonoscopy to find and treat the cause.
Hematology
Having low hemoglobin levels defines anemia. Lacking iron usually causes this condition. Iron is a key ingredient of hemoglobin. Deficient iron commonly makes red blood cells tiny and pale. It’s the world’s most widespread anemia trigger. Various factors dictate iron shortage’s origin, like person’s age, gender, background. Folks may feel constantly tired or breathless, particularly with effort. Fixing the core problem treats anemia, with iron pills typically prescribed. But sometimes, IV iron doses are needed. Untreated, iron anemia lengthens hospital stays and worsens health outcomes.
Anemia: a common illness found in around a fourth of people worldwide. Iron deficiency causes half of all anemia cases. It’s the top reason. For American men under 50, only 1% have iron deficiency anemia. But in developing countries, the rates are higher. About 10% of women of childbearing age in the U.S. experience iron deficiency anemia. This is mostly due to menstrual bleeding. For children aged 12 to 36 months, 9% have iron deficiency. One-third of these kids develop anemia. Though overall iron deficiency anemia rates are low in the U.S., low-income families face a higher risk.
Iron deficiency makes people have microcytic hypochromic anemia. This means they lack healthy red blood cells. Iron is needed to make hemoglobin. Hemoglobin carries oxygen in red blood cells throughout the body. Without enough iron, hemoglobin can’t be produced well. Then, organs and tissues don’t get enough oxygen. This causes anemia symptoms. Iron deficiency anemia can happen for many reasons. Not eating enough iron-rich foods is one cause. Losing blood is another cause. Trouble absorbing iron can also cause it. Bleeding gums may contribute to iron deficiency anemia. In adults over 50, bleeding in the digestive system and iron deficiency anemia could mean cancer. But sometimes the cause is unknown. Celiac disease or inflammatory bowel disease can also lead to iron deficiency anemia. Pregnancy, periods, or growth spurts in kids increase iron needs too. The American Academy of Pediatrics says to give iron supplements for iron deficiency. The amount depends on age and nutrition.
Iron deficiency anemia has different reasons behind it. It depends on things like a person’s age, if they’re male or female, and how well off they are. It can happen because you don’t get enough iron in your diet. Or your body might not absorb iron properly. Blood loss is also a big factor, especially in older adults. Pregnancy increases the body’s need for iron, which can lead to this condition. Some diseases like celiac disease stop iron from being absorbed right. For babies, breastmilk gives them iron that’s easier for their bodies to use compared to cow’s milk. That helps prevent iron deficiency.
Patients mostly have a good outlook in the short term. However, if the root problem persists, their prognosis worsens. Iron shortage over time may cause lung or heart issues. This can be fatal.
Iron deficiency has several possible causes. Treatment depends on the root issue. It’s important to eat iron-rich foods like red meat, poultry, fish, beans, lentils, tofu, fortified cereals, and leafy greens. For mild to moderate iron deficiency anemia, taking oral iron supplements is usually the first treatment tried. But for severe anemia, iron intolerance, non-compliance, or insufficient oral supplement response, intravenous (IV) iron therapy may be an alternative option.
Hematology
Public campaigns inform about iron-rich foods and balanced diets. This combats poor diet access. Better sanitation stops diseases, reducing iron deficiency anemia. Focus on women’s health during pregnancy and periods. Increased iron needs then. Control parasitic infections. They cause blood loss, worsening iron deficiency. Community iron supplements also help in high anemia areas. These improve iron levels and health results.
Hematology
Iron supplements come in forms like Ferrous Sulfate, Gluconate, and Fumarate. The ferrous (Fe2+) iron gets absorbed better. Usually, people take them one to three times daily, between meals to boost absorption. Another type is Iron Polysaccharide Complex, which may be easier on the stomach for some folks who get side effects – it might be easier to tolerate.
Hematology
Iron Dextran and Iron Sucrose: Iron Dextran and Iron Sucrose are IV formulations used when oral iron causes trouble. Doctors prescribe IV iron for severe iron deficiency anemia. It’s also suitable when the body struggles to absorb oral iron or oral iron is hard to tolerate.
Hematology
Giving iron intravenously, or IV, is an option when taking it by mouth is not enough or causes side effects. Direct iron delivery into the bloodstream helps. If anemia is severe or life-threatening, a blood transfusion may rapidly increase hemoglobin levels. This is needed in some cases. If bleeding in the digestive tract causes iron deficiency anemia, doctors may order endoscopic tests. These include gastroscopy and colonoscopy to find and treat the cause.
Hematology
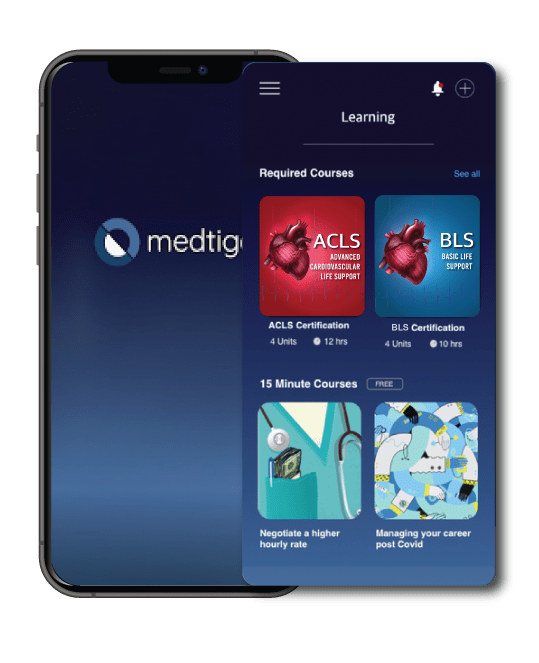
Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.
On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.
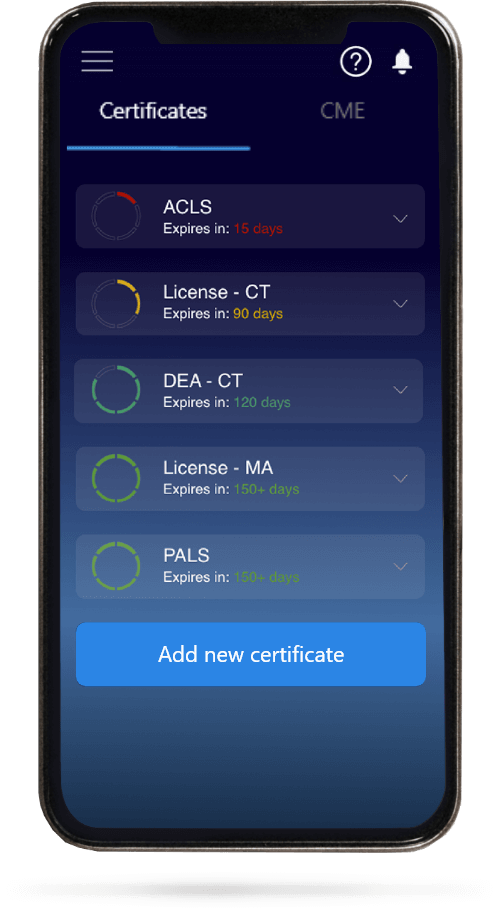
When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.