Background
Antrectomy, also known as distal gastrectomy, is a condition in which a tumor is present in the antrum of the stomach. It is considered part of an integrated plan as a gastrointestinal surgery that is performed along with other operations like gastrectomy or lymph node dissection.
Patients may also suffer from problems after the operation of the digestive system, which are some complications like anastomotic leaks, dumping syndrome, bile reflux, delayed gastric emptying, nutritional deficiencies, and a change in bowel habits.
Indications
Gastric Cancer: The antrectomy may be carried out as a curative part of treatment for the localization of early gastric cancer, which was localized only to the distal stomach.
Peptic Ulcer Disease: Antrectomy is necessary for patients whose treatment modalities fail as they do not respond well to medical management, endoscopic therapy, or after undergoing H. pylori eradication.
Gastric Polyps: Large or nodular polyps in the antrum that are high-risk or symptomatic call for complete removal, hence an antrectomy, to prevent a malignant condition or a recurrence.
Gastric Outlet Obstruction: In cases of gastric outlet obstruction due to benign or malignant strictures or tumors arising from the antrum or inflammatory scarring, anterectomy may be necessitated.
Gastric Motility Disorders: Patients with severe gastroparesis and motility disturbances in the antrum usually have delayed gastric emptying, and symptoms related to the gastrointestinal tract are often found. Thus, antrectomy can be performed for such patients.
Contraindications
Advanced Metastatic Gastric Cancer: If the cancer has advanced, and the disease has metastasized beyond the stomach, antrectomy will not be effective anymore.
Severe Malnutrition or Cachexia: Patients with severe malnutrition, cachexia or pronounced weight loss may have impaired nutrition and decreased physiologic reserves, making them unsuitable candidates for surgical procedure.
Uncontrolled Coagulopathy: Unchecked coagulopathy or some bleeding disorders may elevate perioperative bleeding risk in patients undergoing antrectomy.
Severe Cardiopulmonary Dysfunction: Such conditions as severe CHF, COPD, cor pulmonale may have a negative influence on the cardiopulmonary function and so may lead to complications in some patients.
Outcomes
Periprocedural Care
Informed Consent: An informed consent form for patients aims to provide information about the surgical procedure, for instance, what it does and why it is needed, its risks of failure or adverse events, alternatives existing or possible diagnostic tools, risks connected with anesthesia, and possible complications.
Preoperative Assessment: A complete preoperative assessment evaluates the medical history, physical finding results, laboratory test reports, imaging studies, and another related test.
Anesthesia Evaluation: Communication with the anesthesiologist is crucial since it helps to identify the patient’s anesthesia risks, as well as airway management and pain relief considerations.
Medication Management: It is important to review the patient’s medical profile thoroughly and consultation is necessary before the start of the procedure. This may include discontinuing or adjusting medicines that will increase the risk of bleeding, affect coagulation, or interact with any anesthesia drugs.
Equipment
Patient preparation
Medication Management: Evaluating the patient’s current medications ,and any drugs which will interfere with the surgical process or anesthesia are either changed or discontinued just as the surgeon suggests.
Smoking Cessation: Its significant to quit smoking before surgery for smoker’s patient to lower the risk of complications that include but not limited to; poor wound healing, respiratory problems, and cardiovascular issues. Smoking cessation support as well as counselling sessions can be provided to the patient when required.
Preoperative Skin Preparation: Preoperative skin preparation is done to reduce the incidence of surgical site infections. Also using antiseptic solutions to clean the skin before the procedure is recommended.
Distal Gastrectomy (Stomach Cancer Surgery)
Excision of Gastric (Pyloric) Antrum
Step:1- Anesthesia and Patient’s Positioning: To facilitate comfort and the patient’s immobilisation throughout the surgery, they are given general anaesthesia. A patient is placed on the operating table in supine, and his arms spread.
Step:2- Surgical Method: Surgeons often take different approaches when conducting antrectomy; the choice is affected by the extent of resection and their preferences. Various strategies that are often used include open surgery as well as laparoscopic surgery, including robot-assisted surgery.
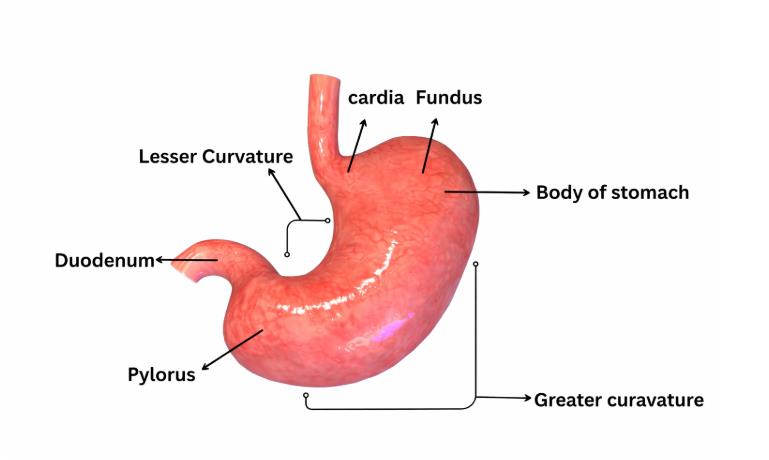
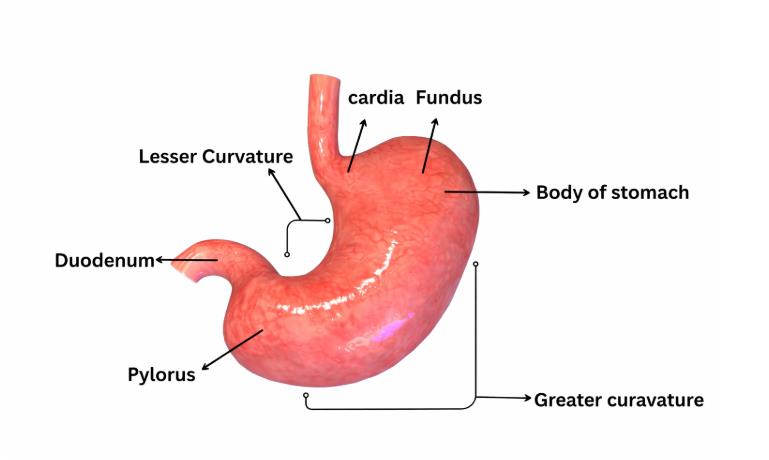
Step 3: Identification of Surgical Anatomy: The surgeon first establishes a pneumoperitoneum, which makes it possible to identify the primary landmarks, including the stomach, pyloric intestine, pylorus, duodenum, and their vicinity.
Step 4: Mobilization of the Stomach: The greater omentum is lifted and divided into two sides to make space and allow the stomach to be mobilized. The gastrocolic ligament is divided to visibly show the greater curvature of the stomach. The lesser omentum is incised to make space for the stomach to check the presence of the gastric cardia and fundus.
Step:5- Division of the gastric artery: In the resection process two gastric arteries- the right gastroepiploic artery and the left gastroepiploic artery and gastric branches on the arterial system are identified and ligated or clipped to prevent blood supply disruption.
Step:6- Stomach Transection: The involved surgical staplers or surgical scissors are used to transect (cut across) the stomach as created by the predetermined resection line. Efforts are exerted on the underside of the tumor around a border known as the resection margin to achieve an adequate margin unexpectedly and preserve the blood flow to the remaining stomach.
Step:7- Removal of Antrum and pylorus: The antral pyloric including structural pathology is meticulously separate from the abdomen.
Step:8-Closure Gastric Remnant: The end part of the stomach is closed or reconstructed as required, according to the extent of resection and the surgeon’s preference.
Complications
Bleeding: Tumor exudates and purulent discharge may appear during surgery in addition to postoperative bleeding which can result in a hematoma formation, hemorrhage or anemia.
Infection: Surgical site infections associated with wound infections, intra-abdominal abscesses, and peritonitis are some of the adverse conditions that may occur. Strategies such as appropriate preoperative antibiotic prophylaxis, aseptic surgical approaches, and meticulous wound care have proven to reduce the danger of infection.
Anastomotic Leak: In case of leaks, the digestive fluids can percolate into the abdominal cavity where peritonitis, sepsis, and abscesses can develop.
Dumping Syndrome: Some patients who had an antrectomy may endure dumping syndrome. Its symptoms are abdominal pain, vomiting, nausea, diarrhea, and palpitations, which are all caused by expedited gastric emptying.
Bowel Obstruction: The development of adhesions, internal hernias, or strictures as late complications affects the intraluminal volume of the bowel, thus interfering with normal bowel function, which may result in bowel obstruction. The manifestations include the abdominal pain, discomfort, nausea, vomiting and complications in passing stool.

Antrectomy, also known as distal gastrectomy, is a condition in which a tumor is present in the antrum of the stomach. It is considered part of an integrated plan as a gastrointestinal surgery that is performed along with other operations like gastrectomy or lymph node dissection.
Patients may also suffer from problems after the operation of the digestive system, which are some complications like anastomotic leaks, dumping syndrome, bile reflux, delayed gastric emptying, nutritional deficiencies, and a change in bowel habits.
Gastric Cancer: The antrectomy may be carried out as a curative part of treatment for the localization of early gastric cancer, which was localized only to the distal stomach.
Peptic Ulcer Disease: Antrectomy is necessary for patients whose treatment modalities fail as they do not respond well to medical management, endoscopic therapy, or after undergoing H. pylori eradication.
Gastric Polyps: Large or nodular polyps in the antrum that are high-risk or symptomatic call for complete removal, hence an antrectomy, to prevent a malignant condition or a recurrence.
Gastric Outlet Obstruction: In cases of gastric outlet obstruction due to benign or malignant strictures or tumors arising from the antrum or inflammatory scarring, anterectomy may be necessitated.
Gastric Motility Disorders: Patients with severe gastroparesis and motility disturbances in the antrum usually have delayed gastric emptying, and symptoms related to the gastrointestinal tract are often found. Thus, antrectomy can be performed for such patients.
Advanced Metastatic Gastric Cancer: If the cancer has advanced, and the disease has metastasized beyond the stomach, antrectomy will not be effective anymore.
Severe Malnutrition or Cachexia: Patients with severe malnutrition, cachexia or pronounced weight loss may have impaired nutrition and decreased physiologic reserves, making them unsuitable candidates for surgical procedure.
Uncontrolled Coagulopathy: Unchecked coagulopathy or some bleeding disorders may elevate perioperative bleeding risk in patients undergoing antrectomy.
Severe Cardiopulmonary Dysfunction: Such conditions as severe CHF, COPD, cor pulmonale may have a negative influence on the cardiopulmonary function and so may lead to complications in some patients.
Informed Consent: An informed consent form for patients aims to provide information about the surgical procedure, for instance, what it does and why it is needed, its risks of failure or adverse events, alternatives existing or possible diagnostic tools, risks connected with anesthesia, and possible complications.
Preoperative Assessment: A complete preoperative assessment evaluates the medical history, physical finding results, laboratory test reports, imaging studies, and another related test.
Anesthesia Evaluation: Communication with the anesthesiologist is crucial since it helps to identify the patient’s anesthesia risks, as well as airway management and pain relief considerations.
Medication Management: It is important to review the patient’s medical profile thoroughly and consultation is necessary before the start of the procedure. This may include discontinuing or adjusting medicines that will increase the risk of bleeding, affect coagulation, or interact with any anesthesia drugs.
Medication Management: Evaluating the patient’s current medications ,and any drugs which will interfere with the surgical process or anesthesia are either changed or discontinued just as the surgeon suggests.
Smoking Cessation: Its significant to quit smoking before surgery for smoker’s patient to lower the risk of complications that include but not limited to; poor wound healing, respiratory problems, and cardiovascular issues. Smoking cessation support as well as counselling sessions can be provided to the patient when required.
Preoperative Skin Preparation: Preoperative skin preparation is done to reduce the incidence of surgical site infections. Also using antiseptic solutions to clean the skin before the procedure is recommended.
Distal Gastrectomy (Stomach Cancer Surgery)
Step:1- Anesthesia and Patient’s Positioning: To facilitate comfort and the patient’s immobilisation throughout the surgery, they are given general anaesthesia. A patient is placed on the operating table in supine, and his arms spread.
Step:2- Surgical Method: Surgeons often take different approaches when conducting antrectomy; the choice is affected by the extent of resection and their preferences. Various strategies that are often used include open surgery as well as laparoscopic surgery, including robot-assisted surgery.
Step 3: Identification of Surgical Anatomy: The surgeon first establishes a pneumoperitoneum, which makes it possible to identify the primary landmarks, including the stomach, pyloric intestine, pylorus, duodenum, and their vicinity.
Step 4: Mobilization of the Stomach: The greater omentum is lifted and divided into two sides to make space and allow the stomach to be mobilized. The gastrocolic ligament is divided to visibly show the greater curvature of the stomach. The lesser omentum is incised to make space for the stomach to check the presence of the gastric cardia and fundus.
Step:5- Division of the gastric artery: In the resection process two gastric arteries- the right gastroepiploic artery and the left gastroepiploic artery and gastric branches on the arterial system are identified and ligated or clipped to prevent blood supply disruption.
Step:6- Stomach Transection: The involved surgical staplers or surgical scissors are used to transect (cut across) the stomach as created by the predetermined resection line. Efforts are exerted on the underside of the tumor around a border known as the resection margin to achieve an adequate margin unexpectedly and preserve the blood flow to the remaining stomach.
Step:7- Removal of Antrum and pylorus: The antral pyloric including structural pathology is meticulously separate from the abdomen.
Step:8-Closure Gastric Remnant: The end part of the stomach is closed or reconstructed as required, according to the extent of resection and the surgeon’s preference.
Bleeding: Tumor exudates and purulent discharge may appear during surgery in addition to postoperative bleeding which can result in a hematoma formation, hemorrhage or anemia.
Infection: Surgical site infections associated with wound infections, intra-abdominal abscesses, and peritonitis are some of the adverse conditions that may occur. Strategies such as appropriate preoperative antibiotic prophylaxis, aseptic surgical approaches, and meticulous wound care have proven to reduce the danger of infection.
Anastomotic Leak: In case of leaks, the digestive fluids can percolate into the abdominal cavity where peritonitis, sepsis, and abscesses can develop.
Dumping Syndrome: Some patients who had an antrectomy may endure dumping syndrome. Its symptoms are abdominal pain, vomiting, nausea, diarrhea, and palpitations, which are all caused by expedited gastric emptying.
Bowel Obstruction: The development of adhesions, internal hernias, or strictures as late complications affects the intraluminal volume of the bowel, thus interfering with normal bowel function, which may result in bowel obstruction. The manifestations include the abdominal pain, discomfort, nausea, vomiting and complications in passing stool.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



