Background
When patients with aortoiliac occlusive disease have no endovascular alternative or are unable to undergo an aortofemoral reconstruction then axillofemoral bypass surgery is indicated as a surgical revascularization technique.
For sufficient blood flow to the ipsilateral arm and one or both legs, the bypass relies on a healthy axillary artery.
One of the possibilities for treating patients who arrive with infected aortic grafts or aortoenteric fistulae is this extra-anatomic reconstructive technique. Next five years, bypass patency rates have been estimated between 40-80%.
Clinical variables affect patency rates and patients with claudicants have better patency than those with critical limb-threatening ischemia (CLTI).
The first successful examples shows that it was possible to bypass blocked sections of the aortoiliac arteries and create a conduit from the axillary artery in the chest to the femoral artery in the groin.
Indications
Individuals who have no endovascular choices for treating their ischemia symptoms
Symptomatic lower-extremity ischemia, acute or chronic
Patients who are at high risk and have serious comorbidities that prevent inline repair using aortic inflow
Infected aortic grafts or prosthetics
Aortoenteric fistulae
Aortic coarctation
Contraindications
Diseased axillary or subclavian arteries
Extreme medical risks for surgery
Active systemic infection or sepsis
Uncontrolled coagulopathy or bleeding disorders
Poor distal target vessels
Prior chest surgery or radiation
Severe pulmonary disease
Outcomes
In a retrospective investigation, Levin et al. (N = 3261) evaluated the results of aortofemoral bypass (AoFB; n = 2825) against axillofemoral bypass (AxFB; n = 436) for intermittent claudication.
The AxFB group’s patients needed more perioperative ipsilateral major amputations even though they had shorter postoperative lengths of stay and less perioperative pulmonary and renal problems.
Six patients were lost to follow-up after the first month. A 5-year primary patency rate of 88.6%, a primary-assisted patency rate of 94.3%, and a secondary patency rate of 94.3% were recorded.
Equipment
Polytetrafluoroethylene (PTFE) or Dacron-based aortic grafts (6-10 mm)
Doppler ultrasonography (US) device
Standard vascular clamps and instruments
Tunneling device
Patient Preparation
To confirm tissue loss, rest discomfort, and ischemia-related claudication, a preoperative workup is necessary. The ankle-brachial index (ABI) should be the first step in screening.
Patients should have a cardiopulmonary evaluation prior to surgery; if peripheral arterial disease is progressive and symptomatic, it probably indicates underlying cardiovascular disease.
To detect any issues with the axillary or subclavian arteries, bilateral brachial blood pressure readings should be taken before surgery to check bypass inflow.
It is recommended to use the axillary artery on the side with the higher blood pressure if the limbs’ systolic pressures differ by 10 mm Hg or more.
Due to the potential for discomfort during axillary artery exploration and the graft’s proximal tunnelling from the chest to the distal femoral landing site, axillofemoral bypass surgery is often performed under general anaesthesia.
Patient Positioning
The patient should be positioned in supine position. A sterile area should be set up from the neck to the anterior thigh including the chest, flank, and belly.
When tunnelling the graft, place a wrapped towel below the ipsilateral torso to provide clear view of the lateral chest wall.
After axillary anastomosis, prepare the donor arm sterilely so that intraoperative limb abduction may be performed to determine the graft lie.
Technique
Step 1: Exposure of axillary artery
Cut the infraclavicular ligament transversely i.e., about two fingerbreadths below the clavicle. Fibers are divided superiorly and inferiorly, exposing the pectoralis muscle.
The access to the artery requires inferior mobilization of the axillary vein, which is located anterior to the artery.
Isolating an artery that is 3 to 4 cm long necessitates the ligation or management of certain branching arteries.
Step 2: Exposure of femoral artery
As per requirement for revascularization, get either unilateral or bilateral femoral artery exposures. To expose the femur, make oblique or longitudinal groin incisions.
At the level of the common femoral artery, make the incision along the femoral pulse. Cut through the subcutaneous tissues to enter inside the femoral sheath.
The femoral vein is placed lateral to the artery. By using vascular loops to regulate the common, superficial, and deep femoral arteries.
Step 3: Tunneling of graft
Subcutaneous tunnelling should be done prior to systemic heparinization. Create a midaxillary tunnel from the axillary incision to the femoral incision using a graft tunnelling tool, above the abdominal fascia and lateral to the nipple.
Make sure there are no kinks or twists while using the device to pass the PTFE or Dacron graft through the tube.
Step 4: Axillary anastomosis
Give intravenous heparin before vascular control is established to create anastomosis. Start with the proximal axillary anastomosis.
It is important to avoid treating the axillary and subclavian arteries aggressively since they are much more delicate than the femoral arteries. The axillary artery can be controlled both proximally and distally by using angled clamps.
Conduct a longitudinal arteriotomy and create a hood for the Dacron/PTFE graft. As the arm is abducted, check the distal axillary artery outflow and graft input to make sure the anastomosis is not under any strain.
Step 5: Femoral anastomosis
Make the distal femorofemoral anastomosis first, then land on the distal axillary graft on the ipsilateral portion of the femorofemoral graft if a bifemoral arrangement is needed.
A longitudinal arteriotomy should be performed once the femoral vessels have been managed properly. An acceptable branch of the common femoral artery should be the end-to-side location of the distal femoral anastomosis.
The deep femoral artery should be included in the anastomosis, if the superficial femoral artery is seriously weak. Significant disease on the distal target vessel may necessary a concurrent femoral artery endarterectomy.

Femoral arteries in groin area for bypass
Complications
Graft thrombosis
Brachial plexus injury
Graft infection
Axillary pullout syndrome
Early graft thrombosis and delayed pseudoaneurysm of the graft

When patients with aortoiliac occlusive disease have no endovascular alternative or are unable to undergo an aortofemoral reconstruction then axillofemoral bypass surgery is indicated as a surgical revascularization technique.
For sufficient blood flow to the ipsilateral arm and one or both legs, the bypass relies on a healthy axillary artery.
One of the possibilities for treating patients who arrive with infected aortic grafts or aortoenteric fistulae is this extra-anatomic reconstructive technique. Next five years, bypass patency rates have been estimated between 40-80%.
Clinical variables affect patency rates and patients with claudicants have better patency than those with critical limb-threatening ischemia (CLTI).
The first successful examples shows that it was possible to bypass blocked sections of the aortoiliac arteries and create a conduit from the axillary artery in the chest to the femoral artery in the groin.
Individuals who have no endovascular choices for treating their ischemia symptoms
Symptomatic lower-extremity ischemia, acute or chronic
Patients who are at high risk and have serious comorbidities that prevent inline repair using aortic inflow
Infected aortic grafts or prosthetics
Aortoenteric fistulae
Aortic coarctation
Diseased axillary or subclavian arteries
Extreme medical risks for surgery
Active systemic infection or sepsis
Uncontrolled coagulopathy or bleeding disorders
Poor distal target vessels
Prior chest surgery or radiation
Severe pulmonary disease
In a retrospective investigation, Levin et al. (N = 3261) evaluated the results of aortofemoral bypass (AoFB; n = 2825) against axillofemoral bypass (AxFB; n = 436) for intermittent claudication.
The AxFB group’s patients needed more perioperative ipsilateral major amputations even though they had shorter postoperative lengths of stay and less perioperative pulmonary and renal problems.
Six patients were lost to follow-up after the first month. A 5-year primary patency rate of 88.6%, a primary-assisted patency rate of 94.3%, and a secondary patency rate of 94.3% were recorded.
Polytetrafluoroethylene (PTFE) or Dacron-based aortic grafts (6-10 mm)
Doppler ultrasonography (US) device
Standard vascular clamps and instruments
Tunneling device
To confirm tissue loss, rest discomfort, and ischemia-related claudication, a preoperative workup is necessary. The ankle-brachial index (ABI) should be the first step in screening.
Patients should have a cardiopulmonary evaluation prior to surgery; if peripheral arterial disease is progressive and symptomatic, it probably indicates underlying cardiovascular disease.
To detect any issues with the axillary or subclavian arteries, bilateral brachial blood pressure readings should be taken before surgery to check bypass inflow.
It is recommended to use the axillary artery on the side with the higher blood pressure if the limbs’ systolic pressures differ by 10 mm Hg or more.
Due to the potential for discomfort during axillary artery exploration and the graft’s proximal tunnelling from the chest to the distal femoral landing site, axillofemoral bypass surgery is often performed under general anaesthesia.
The patient should be positioned in supine position. A sterile area should be set up from the neck to the anterior thigh including the chest, flank, and belly.
When tunnelling the graft, place a wrapped towel below the ipsilateral torso to provide clear view of the lateral chest wall.
After axillary anastomosis, prepare the donor arm sterilely so that intraoperative limb abduction may be performed to determine the graft lie.
Step 1: Exposure of axillary artery
Cut the infraclavicular ligament transversely i.e., about two fingerbreadths below the clavicle. Fibers are divided superiorly and inferiorly, exposing the pectoralis muscle.
The access to the artery requires inferior mobilization of the axillary vein, which is located anterior to the artery.
Isolating an artery that is 3 to 4 cm long necessitates the ligation or management of certain branching arteries.
Step 2: Exposure of femoral artery
As per requirement for revascularization, get either unilateral or bilateral femoral artery exposures. To expose the femur, make oblique or longitudinal groin incisions.
At the level of the common femoral artery, make the incision along the femoral pulse. Cut through the subcutaneous tissues to enter inside the femoral sheath.
The femoral vein is placed lateral to the artery. By using vascular loops to regulate the common, superficial, and deep femoral arteries.
Step 3: Tunneling of graft
Subcutaneous tunnelling should be done prior to systemic heparinization. Create a midaxillary tunnel from the axillary incision to the femoral incision using a graft tunnelling tool, above the abdominal fascia and lateral to the nipple.
Make sure there are no kinks or twists while using the device to pass the PTFE or Dacron graft through the tube.
Step 4: Axillary anastomosis
Give intravenous heparin before vascular control is established to create anastomosis. Start with the proximal axillary anastomosis.
It is important to avoid treating the axillary and subclavian arteries aggressively since they are much more delicate than the femoral arteries. The axillary artery can be controlled both proximally and distally by using angled clamps.
Conduct a longitudinal arteriotomy and create a hood for the Dacron/PTFE graft. As the arm is abducted, check the distal axillary artery outflow and graft input to make sure the anastomosis is not under any strain.
Step 5: Femoral anastomosis
Make the distal femorofemoral anastomosis first, then land on the distal axillary graft on the ipsilateral portion of the femorofemoral graft if a bifemoral arrangement is needed.
A longitudinal arteriotomy should be performed once the femoral vessels have been managed properly. An acceptable branch of the common femoral artery should be the end-to-side location of the distal femoral anastomosis.
The deep femoral artery should be included in the anastomosis, if the superficial femoral artery is seriously weak. Significant disease on the distal target vessel may necessary a concurrent femoral artery endarterectomy.

Femoral arteries in groin area for bypass
Graft thrombosis
Brachial plexus injury
Graft infection
Axillary pullout syndrome
Early graft thrombosis and delayed pseudoaneurysm of the graft
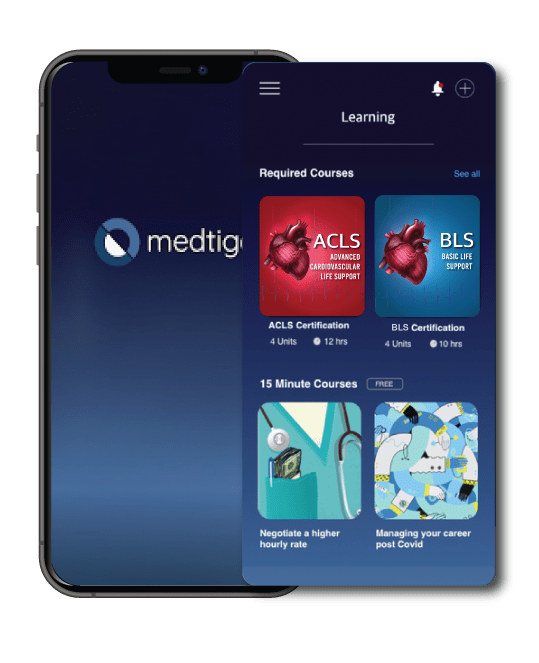
Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.
On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.
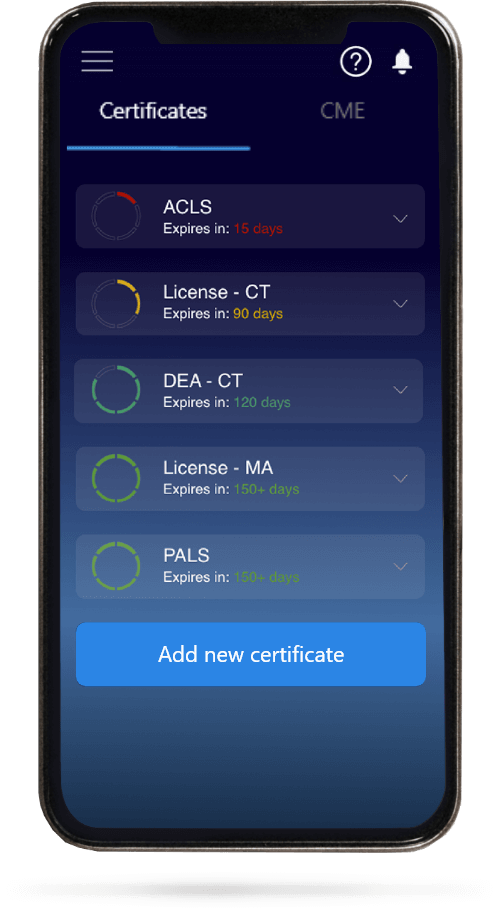
When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.