Background
Bakri balloon placement, also known as bakri postpartum balloon, is a medical procedure designed to manage postpartum hemorrhage, a potentially life-threatening complication that can occur after childbirth. This technique involves the insertion of a specially designed balloon into the uterus to apply pressure and control bleeding.
Globally, postpartum haemorrhage is a major contributor to maternal morbidity and mortality.When traditional methods like uterine massage, medications, or surgical interventions fail to control excessive bleeding after delivery, bakri balloon placement emerges as an effective option.
Indications
Postpartum hemorrhage:
It is used when conventional methods to control bleeding, such as uterine massage, medications, and surgical interventions like uterine artery embolization or hysterectomy, have failed or are not feasible.
Contraindications
Uterine rupture: If there is a known or suspected uterine rupture, bakri balloon placement may not be suitable as it can exacerbate the condition.
Active pelvic infection: Presence of an active pelvic infection or chorioamnionitis can increase the risk of complications and contraindicate the use of a bakri balloon.
Allergy or sensitivity to balloon materials: The components used to make the bakri balloon may cause allergic responses or sensitivities in certain people. In such cases, alternative interventions should be considered.
Uterine anomalies or abnormalities: Structural abnormalities or anomalies in the uterus may make it difficult or unsafe to insert the bakri balloon.
Uncontrolled coagulopathy or bleeding disorders: If a patient has uncontrolled coagulopathy or is unable to clot blood effectively, bakri balloon placement might not be advisable due to the increased risk of bleeding complications.
Outcomes
Hemorrhage control: The primary goal of bakri balloon placement is to control and reduce postpartum bleeding. When properly inserted and inflated, the balloon applies pressure to the uterine walls, compressing blood vessels and reducing bleeding.
Reduced need for invasive procedures: Bakri balloon placement can often help avoid more invasive surgical interventions, such as hysterectomy, in cases of postpartum hemorrhage. It is considered a less invasive option to manage bleeding, potentially sparing the patient from more extensive surgical procedures.
Stabilization of the patient: By controlling excessive bleeding, the Bakri balloon can contribute to stabilizing the patient’s condition. This stabilization is crucial in preventing severe complications associated with postpartum hemorrhage, such as hypovolemic shock or organ failure.
Successful delivery of other treatments: In some cases, bakri balloon placement allows time for additional treatments or interventions to be administered. This might include blood transfusions, administration of medications to help the uterus contract, or addressing underlying causes of bleeding.
Equipment
Bakri Balloon: The main device consists of a soft, silicone balloon attached to a catheter. The balloon is inflated with sterile saline or water after insertion into the uterus to apply pressure and stop bleeding.
Catheter: A sterile flexible tube that serves as a conduit for inflating the balloon and guiding it into the uterus. It’s usually made of medical-grade material and comes in various sizes.
Speculum: A device used for vaginal examination to visualize the cervix and facilitate the insertion of the catheter into the uterus.
Sterile Gloves and Drapes: To maintain a sterile field during the procedure, healthcare providers use sterile gloves and sterile drapes to cover the patient.
Sterile Solution: Typically, sterile saline or sterile water is used to inflate the bakri balloon. It’s crucial to ensure that the solution used is sterile to prevent infections.
Syringe and Connector: Used to inject the sterile solution into the bakri balloon once it’s properly placed in the uterus. The connector allows for controlled inflation of the balloon.
Patient preparation
Depending on the patient’s condition and the healthcare provider’s discretion, local anesthesia or to reduce discomfort during the treatment, conscious sedation may be used.
Advise the patient to void their intestines and bladder before to the treatment. Position the patient comfortably in the lithotomy position for easier access to the vaginal area.
Technique
After vaginal delivery
Prior to inserting the balloon, it’s crucial to confirm bladder emptiness by utilizing a Foley catheter.
Examine the uterine cavity thoroughly to verify its absence of placental fragments.
Cleanse the vagina & cervix using an antiseptic solution, like povidone iodine.
Secure a cervix using forceps ring, then carefully put a balloon in uterine cavity using ultrasound assistance.
ensuring that a balloon’s whole length goes through the cervical canal on the cervical ostium within.
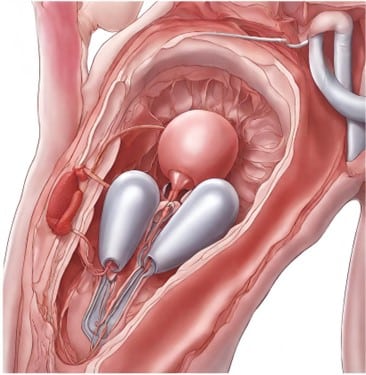
When the accurate positioning is verified, use the provided syringe to fill a balloon with saline sterile solution. It is recommended to stay within the balloon’s 500 mL highest capacity.
To enhance the effectiveness of tamponade, particularly focusing on a bottom uterine section, softly pull on the balloon shaft. To accomplish this, secure the shaft of the balloon to leg of the patient or connect this to the weight, making sure the total weight does not surpass 500 gm.
Attach the drainage outlet to the fluid collection pouch for the purpose of observing hemostasis. Consistently observe the patient for any indications of enhanced uterine cramps & bleeding.
After cesarean section
Pass the catheter’s end through exposed incision uterine towards a cervix, guiding it in the vagina.
Take caution when closing the uterine incision to avoid harm to a balloon with a suturing needle. Inflate a balloon while directly observing the procedure.
Combination with other procedures
Internal tamponade plus external compression
Intrauterine balloon catheters can be used in combination with other surgical interventions to increase effectiveness.
To possibly improve efficacy, balloon catheters intrauterine is utilized in conjunction with additional surgical procedures.
According to one study, to treat uterine atony effectively involves using a bakri balloon intrauterine in addition to a B-Lynch compression suture (uterine).
Laboratory Tests
Complete Blood Count: This test measures different components of blood, including RBC, WBC, & platelets. It helps assess the severity of bleeding and provides information about the patient’s overall blood count.
Blood Chemistry Panel: This test assesses various blood components, including electrolytes, kidney function, liver function, and other metabolic markers. It helps in evaluating the patient’s overall health status and identifying any potential underlying issues.
Blood Gas Analysis: In situations where there is significant bleeding, blood gas analysis can provide information about the patient’s acid-base balance, oxygenation, and overall respiratory status.
The Tamponade Test
When the balloon has inflated and control is established, the test is deemed successful.
Individuals who test negative, that is, continue to bleed even after the balloon is inserted, should move on to more invasive treatment techniques like embolization & laparotomy.
Complications
Uterine Perforation: During insertion, there’s a risk of inadvertently perforating the uterus, which can lead to severe bleeding and injury to surrounding organs and necessitate further surgical intervention.
Infection: Any intrauterine device carries a risk of introducing infection into the uterus, potentially leading to endometritis or systemic infection if not managed properly.
Retention or Expulsion: In some cases, the balloon may fail to remain in place or may be expelled prematurely, compromising its ability to manage hemorrhage effectively.
Allergic Reaction: In rare cases, people may become allergic to the ingredients in the balloon, leading to localized or systemic symptoms.
Ineffective Hemorrhage Control: In certain situations, such as extensive or severe uterine damage, the bakri balloon may not adequately control bleeding, requiring additional interventions or surgical procedures.

Bakri balloon placement, also known as bakri postpartum balloon, is a medical procedure designed to manage postpartum hemorrhage, a potentially life-threatening complication that can occur after childbirth. This technique involves the insertion of a specially designed balloon into the uterus to apply pressure and control bleeding.
Globally, postpartum haemorrhage is a major contributor to maternal morbidity and mortality.When traditional methods like uterine massage, medications, or surgical interventions fail to control excessive bleeding after delivery, bakri balloon placement emerges as an effective option.
Postpartum hemorrhage:
It is used when conventional methods to control bleeding, such as uterine massage, medications, and surgical interventions like uterine artery embolization or hysterectomy, have failed or are not feasible.
Uterine rupture: If there is a known or suspected uterine rupture, bakri balloon placement may not be suitable as it can exacerbate the condition.
Active pelvic infection: Presence of an active pelvic infection or chorioamnionitis can increase the risk of complications and contraindicate the use of a bakri balloon.
Allergy or sensitivity to balloon materials: The components used to make the bakri balloon may cause allergic responses or sensitivities in certain people. In such cases, alternative interventions should be considered.
Uterine anomalies or abnormalities: Structural abnormalities or anomalies in the uterus may make it difficult or unsafe to insert the bakri balloon.
Uncontrolled coagulopathy or bleeding disorders: If a patient has uncontrolled coagulopathy or is unable to clot blood effectively, bakri balloon placement might not be advisable due to the increased risk of bleeding complications.
Hemorrhage control: The primary goal of bakri balloon placement is to control and reduce postpartum bleeding. When properly inserted and inflated, the balloon applies pressure to the uterine walls, compressing blood vessels and reducing bleeding.
Reduced need for invasive procedures: Bakri balloon placement can often help avoid more invasive surgical interventions, such as hysterectomy, in cases of postpartum hemorrhage. It is considered a less invasive option to manage bleeding, potentially sparing the patient from more extensive surgical procedures.
Stabilization of the patient: By controlling excessive bleeding, the Bakri balloon can contribute to stabilizing the patient’s condition. This stabilization is crucial in preventing severe complications associated with postpartum hemorrhage, such as hypovolemic shock or organ failure.
Successful delivery of other treatments: In some cases, bakri balloon placement allows time for additional treatments or interventions to be administered. This might include blood transfusions, administration of medications to help the uterus contract, or addressing underlying causes of bleeding.
Bakri Balloon: The main device consists of a soft, silicone balloon attached to a catheter. The balloon is inflated with sterile saline or water after insertion into the uterus to apply pressure and stop bleeding.
Catheter: A sterile flexible tube that serves as a conduit for inflating the balloon and guiding it into the uterus. It’s usually made of medical-grade material and comes in various sizes.
Speculum: A device used for vaginal examination to visualize the cervix and facilitate the insertion of the catheter into the uterus.
Sterile Gloves and Drapes: To maintain a sterile field during the procedure, healthcare providers use sterile gloves and sterile drapes to cover the patient.
Sterile Solution: Typically, sterile saline or sterile water is used to inflate the bakri balloon. It’s crucial to ensure that the solution used is sterile to prevent infections.
Syringe and Connector: Used to inject the sterile solution into the bakri balloon once it’s properly placed in the uterus. The connector allows for controlled inflation of the balloon.
Depending on the patient’s condition and the healthcare provider’s discretion, local anesthesia or to reduce discomfort during the treatment, conscious sedation may be used.
Advise the patient to void their intestines and bladder before to the treatment. Position the patient comfortably in the lithotomy position for easier access to the vaginal area.
After vaginal delivery
Prior to inserting the balloon, it’s crucial to confirm bladder emptiness by utilizing a Foley catheter.
Examine the uterine cavity thoroughly to verify its absence of placental fragments.
Cleanse the vagina & cervix using an antiseptic solution, like povidone iodine.
Secure a cervix using forceps ring, then carefully put a balloon in uterine cavity using ultrasound assistance.
ensuring that a balloon’s whole length goes through the cervical canal on the cervical ostium within.
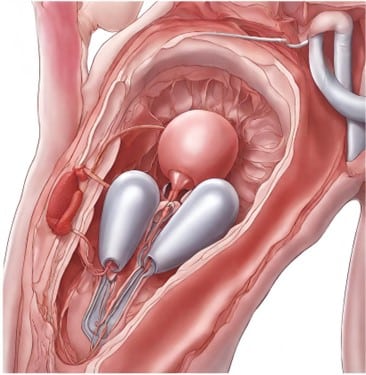
When the accurate positioning is verified, use the provided syringe to fill a balloon with saline sterile solution. It is recommended to stay within the balloon’s 500 mL highest capacity.
To enhance the effectiveness of tamponade, particularly focusing on a bottom uterine section, softly pull on the balloon shaft. To accomplish this, secure the shaft of the balloon to leg of the patient or connect this to the weight, making sure the total weight does not surpass 500 gm.
Attach the drainage outlet to the fluid collection pouch for the purpose of observing hemostasis. Consistently observe the patient for any indications of enhanced uterine cramps & bleeding.
Pass the catheter’s end through exposed incision uterine towards a cervix, guiding it in the vagina.
Take caution when closing the uterine incision to avoid harm to a balloon with a suturing needle. Inflate a balloon while directly observing the procedure.
Internal tamponade plus external compression
Intrauterine balloon catheters can be used in combination with other surgical interventions to increase effectiveness.
To possibly improve efficacy, balloon catheters intrauterine is utilized in conjunction with additional surgical procedures.
According to one study, to treat uterine atony effectively involves using a bakri balloon intrauterine in addition to a B-Lynch compression suture (uterine).
Complete Blood Count: This test measures different components of blood, including RBC, WBC, & platelets. It helps assess the severity of bleeding and provides information about the patient’s overall blood count.
Blood Chemistry Panel: This test assesses various blood components, including electrolytes, kidney function, liver function, and other metabolic markers. It helps in evaluating the patient’s overall health status and identifying any potential underlying issues.
Blood Gas Analysis: In situations where there is significant bleeding, blood gas analysis can provide information about the patient’s acid-base balance, oxygenation, and overall respiratory status.
The Tamponade Test
When the balloon has inflated and control is established, the test is deemed successful.
Individuals who test negative, that is, continue to bleed even after the balloon is inserted, should move on to more invasive treatment techniques like embolization & laparotomy.
Uterine Perforation: During insertion, there’s a risk of inadvertently perforating the uterus, which can lead to severe bleeding and injury to surrounding organs and necessitate further surgical intervention.
Infection: Any intrauterine device carries a risk of introducing infection into the uterus, potentially leading to endometritis or systemic infection if not managed properly.
Retention or Expulsion: In some cases, the balloon may fail to remain in place or may be expelled prematurely, compromising its ability to manage hemorrhage effectively.
Allergic Reaction: In rare cases, people may become allergic to the ingredients in the balloon, leading to localized or systemic symptoms.
Ineffective Hemorrhage Control: In certain situations, such as extensive or severe uterine damage, the bakri balloon may not adequately control bleeding, requiring additional interventions or surgical procedures.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



