Background
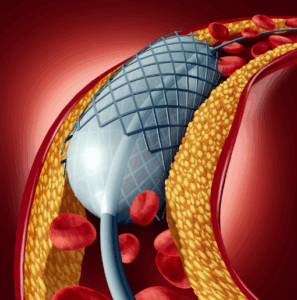
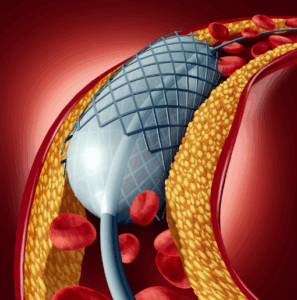
Carotid Artery Stenting (CAS) is a minimally invasive procedure used to treat carotid artery disease, these conditions include the narrowing and/or obstruction of the carotid artery, usually by blockages by plaques, and commonly called atherosclerosis. These arteries are situated on each side of neck and the blood which is supplied to the brain through these passes. Stenosis of the carotids raises the risk of a stroke simply because less blood is getting through the brain or because a blood clot can occur and block the blood supply to the brain. In the CAS procedure, a small, temporary tube stent is implanted within the carotid artery to ensure that the artery is opened and kept open as a way of facilitating proper circulation of blood. This is done by passing a thin tube called catheter through a small cut which is often made in the groin up into the carotid arterial system. The stent is then used to support the artery to avoid the likelihood of its narrowing over again. Any plaque that become mobilized during the procedure could cause an embolism and thus using a filter device can help capture this plaque.
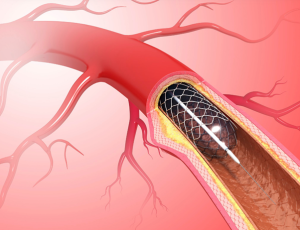
Carotid artery stent
Indications
Symptomatic Carotid Stenosis
High-grade stenosis (70–99%): in patients who have experienced symptoms such as:
Transient ischemic attacks (TIA) or Minor stroke
Amaurosis fugax is a sudden attack of blindness in one eye (monocular transient ischemic attack).
Symptomatic patients with moderate stenosis (50-69%) and additional risk factors when stenting is believed to be more appropriate than medical treatment.
Asymptomatic Carotid Stenosis
CEA candidates with asymptomatic high-grade stenosis (> 80%) of carotid artery and clinical contraindication for surgery, and those with life expectancy of more than five years.
As an alternative to CEA in patients who are at high surgical risk due to comorbidities, such as: Severe cardiac disease, pulmonary disease or other medical illnesses predisposing an individual to experience surgical complications.
Contraindications with respect to anatomical characteristics of the patient or the disease for CEA.
Medical conditions that elevate surgical risk: Severe coronary artery disease. Congestive heart failure Chronic obstructive pulmonary disease (COPD) refers to a family of progressive lung diseases characterized by airflow obstruction that is not fully reversible.
Restenosis: For patients with restenosis after prior CEA, especially if the restenosis is symptomatic, stenting may be preferred to avoid repeated surgical intervention.
Contraindications
Severe Allergies to Stent Materials or Contrast Agents: Hypersensitivity to the content of the contrast media or to the stent material, such as nickel.
Severe Atherosclerosis of Aortic Arch or Proximal Carotid: The technical factor that could result from an excessive plaque burden involved an increased chance of developing an embolic during the procedure.
Active Bleeding or High Bleeding Risk: Such patients cannot use dual antiplatelet therapy because of increased risk of bleedings.
Severe Renal Dysfunction: Those patients with impaired renal profile have contraindicated imaging with contrast agents as this worsens the renal compaction.
Acute Stroke Symptoms: Symptoms seen in the days immediately preceding a planned stent procedure (usually <48 hours), because the risk of procedure-related stroke will rise.
Outcomes
Periprocedural care
Equipment
Imaging Equipment
Fluoroscopy Unit
Ultrasound Doppler
Intracranial and Cervical Angiography
Access Equipment
Guide Catheter
Sheaths
Microcatheters
Protection Devices
Distal Embolic Protection Device
Carotid Stent System
Self-Expanding Stent
Balloon Catheter
Monitoring Equipment
Intravascular Ultrasound (IVUS)
Hemodynamic Monitoring
Patient preparation
Pre-Procedure Assessment
History and Physical Exam: Take a brief history about cardiovascular, cerebrovascular and peripheral vascular disease.
Imaging: Compliance of the location and severity of stenosis with that seen on ultrasound, CT angiograms or MR angiograms.
Risk Assessment: Assess patient’s risk of adverse outcomes; age, co-morbidity and symptoms; for example, a recent transient ischemic attack.
Medications Review: Optimise doses anticoagulants, antiplatelets and other related factors.
Medication Preparation
Antiplatelet Therapy: Preoperatively, give DAPT for 3-5 days comprising aspirin and ideally clopidogrel since they minimise thromboembolic. risks.
Anticoagulation Management: Conduction of such therapies including the use of anticoagulants should in consultation with the patients’ risk status particularly if the patient has other medical conditions requiring the drugs for long term usage.
Statins: The patient may benefit from a statin for the perioperative period and to decrease complications.
Laboratory Tests
Blood Tests: Routine laboratories include the complete blood count, coagulation profile including prothrombin time/international normalised ratio (PT/INR) & activated partial thromboplastin time (aPTT), and basic renal function as estimated by serum creatinine. Other Tests: In some cases, the level of electrolytes, glucose, blood sugar, or/and other parameters should be evaluated according to the patient’s condition.
Informed Consent: Outline the risk factors, the benefits and disadvantages, such as stroke risk, restenosis rates, and complications of procedure.
Procedure Overview: Enumerate the procedures involved, potential findings, and the rationale for compliance with stenting directions before, during and after the procedure.
Post-Procedure Care: Follow up after the procedure and what the patient should expect concerning the recovery process restrictions in activities and adherence to medications.
Patient position
Supine Position: The patient is mostly kept in a supine position; the patient lies on their back on the operating table. It enables establishing an access to the femoral artery, it is one of the most preferred vessels for vascular access.
Head Positioning: The patient’s head is inclined forward and rotated slightly to the opposite side of the neck. This positioning helps have a better view of the clinician during the procedure and thus can be adopted.
Pre-procedure Preparation
Patient Assessment:
Medical history and physical examination: Carotid Doppler ultrasound, Computerized tomographic angiography.
Antiplatelet Therapy: Inpatients are often started and continued antiplatelet drugs (aspirin and clopidogrel) as a prophylaxis against thromboembolic events.
Consent: However, the informed consent is given after all the risk earlier discussed and the benefits have been understood.
Step 2-Anesthesia: A local anaesthesia is employed frequently in this procedure, but sedation may also be used.
Step 3-Access Site: Catheter is mostly placed through the femoral artery at the groins or sometimes through the radial artery.
Step 4-Catheterization: An over-the-wire catheter is introduced through the arterial system up to the carotid artery.
Step 5-Angiography: Further, contrast dye is introduced to determine the degree of stenosis of the carotid arteries.
Step 6-Balloon Angioplasty: A balloon catheter is placed on the location of the stenosis and inflated to widen the artery.
Step 7-Stent Placement: This is followed by implantation of stent at the site of blockage, to have the arterial opening persistently patent. The stent is frequently a self-expanding mesh made from a metallic material which gives support to the structure.
Step 8-Post-Procedure Imaging: Subsequent angiography can be done to assess stent position and blood flow.
Step 9-Sheath Removal: The sheath is then withdrawn, and haemostasis is obtained, often with direct pressure or by using a closure mechanism.
Step 10-Post-Procedure Care:
Monitoring:
Patients are observed in a recovery area for some hours to look for complications like stroke, excessive bleeding or vascular complications.
Antiplatelet Therapy: Continuation of antiplatelet medications to reduce the risk of thrombus formation in the stent.
Follow-Up: To follow up as outpatient for carotid Doppler ultrasounds and optimum control of risk factors such as hypertension, hyperlipidemia among others.
Complications
Stroke: There is a risk of stroke during or shortly after the procedure, often due to embolism of plaque material or blood clots.
Transient Ischemic Attack (TIA): Mild neurological signs may manifest, symptoms which usually last up to 24 hours.
Hemorrhage: This may be at the access site most commonly in the groin or in the brain.
Stent-related complications: These include stent movement out of the intended location, or re-coiling of the stent, or clot formation within the stent.
Vascular complications: Complications affecting the artery or surrounding structures include dissection, tearing of the artery wall or perforation.
Nerve injury: There is a potential risk of damaging nearby nerves, which may result in complications such as hoarseness, difficulty swallowing, or facial weakness.
Allergic reactions: A patient might develop an allergy to the agents used in the procedure such as the contrast media.
Infection: Although such incidence is rare, there is always a possibility of developing an infection at the site of catheterization or at a more profound level in the vascular tree.

Carotid Artery Stenting (CAS) is a minimally invasive procedure used to treat carotid artery disease, these conditions include the narrowing and/or obstruction of the carotid artery, usually by blockages by plaques, and commonly called atherosclerosis. These arteries are situated on each side of neck and the blood which is supplied to the brain through these passes. Stenosis of the carotids raises the risk of a stroke simply because less blood is getting through the brain or because a blood clot can occur and block the blood supply to the brain. In the CAS procedure, a small, temporary tube stent is implanted within the carotid artery to ensure that the artery is opened and kept open as a way of facilitating proper circulation of blood. This is done by passing a thin tube called catheter through a small cut which is often made in the groin up into the carotid arterial system. The stent is then used to support the artery to avoid the likelihood of its narrowing over again. Any plaque that become mobilized during the procedure could cause an embolism and thus using a filter device can help capture this plaque.
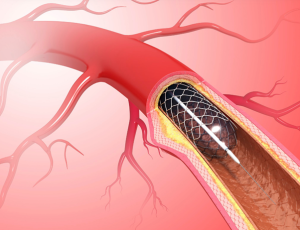
Carotid artery stent
Symptomatic Carotid Stenosis
High-grade stenosis (70–99%): in patients who have experienced symptoms such as:
Transient ischemic attacks (TIA) or Minor stroke
Amaurosis fugax is a sudden attack of blindness in one eye (monocular transient ischemic attack).
Symptomatic patients with moderate stenosis (50-69%) and additional risk factors when stenting is believed to be more appropriate than medical treatment.
Asymptomatic Carotid Stenosis
CEA candidates with asymptomatic high-grade stenosis (> 80%) of carotid artery and clinical contraindication for surgery, and those with life expectancy of more than five years.
As an alternative to CEA in patients who are at high surgical risk due to comorbidities, such as: Severe cardiac disease, pulmonary disease or other medical illnesses predisposing an individual to experience surgical complications.
Contraindications with respect to anatomical characteristics of the patient or the disease for CEA.
Medical conditions that elevate surgical risk: Severe coronary artery disease. Congestive heart failure Chronic obstructive pulmonary disease (COPD) refers to a family of progressive lung diseases characterized by airflow obstruction that is not fully reversible.
Restenosis: For patients with restenosis after prior CEA, especially if the restenosis is symptomatic, stenting may be preferred to avoid repeated surgical intervention.
Severe Allergies to Stent Materials or Contrast Agents: Hypersensitivity to the content of the contrast media or to the stent material, such as nickel.
Severe Atherosclerosis of Aortic Arch or Proximal Carotid: The technical factor that could result from an excessive plaque burden involved an increased chance of developing an embolic during the procedure.
Active Bleeding or High Bleeding Risk: Such patients cannot use dual antiplatelet therapy because of increased risk of bleedings.
Severe Renal Dysfunction: Those patients with impaired renal profile have contraindicated imaging with contrast agents as this worsens the renal compaction.
Acute Stroke Symptoms: Symptoms seen in the days immediately preceding a planned stent procedure (usually <48 hours), because the risk of procedure-related stroke will rise.
Equipment
Imaging Equipment
Fluoroscopy Unit
Ultrasound Doppler
Intracranial and Cervical Angiography
Access Equipment
Guide Catheter
Sheaths
Microcatheters
Protection Devices
Distal Embolic Protection Device
Carotid Stent System
Self-Expanding Stent
Balloon Catheter
Monitoring Equipment
Intravascular Ultrasound (IVUS)
Hemodynamic Monitoring
Patient preparation
Pre-Procedure Assessment
History and Physical Exam: Take a brief history about cardiovascular, cerebrovascular and peripheral vascular disease.
Imaging: Compliance of the location and severity of stenosis with that seen on ultrasound, CT angiograms or MR angiograms.
Risk Assessment: Assess patient’s risk of adverse outcomes; age, co-morbidity and symptoms; for example, a recent transient ischemic attack.
Medications Review: Optimise doses anticoagulants, antiplatelets and other related factors.
Medication Preparation
Antiplatelet Therapy: Preoperatively, give DAPT for 3-5 days comprising aspirin and ideally clopidogrel since they minimise thromboembolic. risks.
Anticoagulation Management: Conduction of such therapies including the use of anticoagulants should in consultation with the patients’ risk status particularly if the patient has other medical conditions requiring the drugs for long term usage.
Statins: The patient may benefit from a statin for the perioperative period and to decrease complications.
Laboratory Tests
Blood Tests: Routine laboratories include the complete blood count, coagulation profile including prothrombin time/international normalised ratio (PT/INR) & activated partial thromboplastin time (aPTT), and basic renal function as estimated by serum creatinine. Other Tests: In some cases, the level of electrolytes, glucose, blood sugar, or/and other parameters should be evaluated according to the patient’s condition.
Informed Consent: Outline the risk factors, the benefits and disadvantages, such as stroke risk, restenosis rates, and complications of procedure.
Procedure Overview: Enumerate the procedures involved, potential findings, and the rationale for compliance with stenting directions before, during and after the procedure.
Post-Procedure Care: Follow up after the procedure and what the patient should expect concerning the recovery process restrictions in activities and adherence to medications.
Patient position
Supine Position: The patient is mostly kept in a supine position; the patient lies on their back on the operating table. It enables establishing an access to the femoral artery, it is one of the most preferred vessels for vascular access.
Head Positioning: The patient’s head is inclined forward and rotated slightly to the opposite side of the neck. This positioning helps have a better view of the clinician during the procedure and thus can be adopted.
Patient Assessment:
Medical history and physical examination: Carotid Doppler ultrasound, Computerized tomographic angiography.
Antiplatelet Therapy: Inpatients are often started and continued antiplatelet drugs (aspirin and clopidogrel) as a prophylaxis against thromboembolic events.
Consent: However, the informed consent is given after all the risk earlier discussed and the benefits have been understood.
Step 2-Anesthesia: A local anaesthesia is employed frequently in this procedure, but sedation may also be used.
Step 3-Access Site: Catheter is mostly placed through the femoral artery at the groins or sometimes through the radial artery.
Step 4-Catheterization: An over-the-wire catheter is introduced through the arterial system up to the carotid artery.
Step 5-Angiography: Further, contrast dye is introduced to determine the degree of stenosis of the carotid arteries.
Step 6-Balloon Angioplasty: A balloon catheter is placed on the location of the stenosis and inflated to widen the artery.
Step 7-Stent Placement: This is followed by implantation of stent at the site of blockage, to have the arterial opening persistently patent. The stent is frequently a self-expanding mesh made from a metallic material which gives support to the structure.
Step 8-Post-Procedure Imaging: Subsequent angiography can be done to assess stent position and blood flow.
Step 9-Sheath Removal: The sheath is then withdrawn, and haemostasis is obtained, often with direct pressure or by using a closure mechanism.
Step 10-Post-Procedure Care:
Monitoring:
Patients are observed in a recovery area for some hours to look for complications like stroke, excessive bleeding or vascular complications.
Antiplatelet Therapy: Continuation of antiplatelet medications to reduce the risk of thrombus formation in the stent.
Follow-Up: To follow up as outpatient for carotid Doppler ultrasounds and optimum control of risk factors such as hypertension, hyperlipidemia among others.
Complications
Stroke: There is a risk of stroke during or shortly after the procedure, often due to embolism of plaque material or blood clots.
Transient Ischemic Attack (TIA): Mild neurological signs may manifest, symptoms which usually last up to 24 hours.
Hemorrhage: This may be at the access site most commonly in the groin or in the brain.
Stent-related complications: These include stent movement out of the intended location, or re-coiling of the stent, or clot formation within the stent.
Vascular complications: Complications affecting the artery or surrounding structures include dissection, tearing of the artery wall or perforation.
Nerve injury: There is a potential risk of damaging nearby nerves, which may result in complications such as hoarseness, difficulty swallowing, or facial weakness.
Allergic reactions: A patient might develop an allergy to the agents used in the procedure such as the contrast media.
Infection: Although such incidence is rare, there is always a possibility of developing an infection at the site of catheterization or at a more profound level in the vascular tree.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



