Background
Carotid endarterectomy (CEA) is a surgical procedure carried out to clear plaque out of the carotid arteries. These are the major blood vessels that lie in the neck, connecting the neck to the brain and providing the later with oxygen-rich blood. This is one of the surgical measures used in patients who suffer a high degree of blockage in their carotid arteries (carotid artery stenosis), which predisposes them to stroke attacks.
Carotid Endarterectomy
CEA is frequently done to prevent a stroke in patients who suffer from TIAs or minor strokes and who also have the carotid artery with more blockages known through diagnostic tests, like carotid ultrasound or MRA.
Indications
Contraindications
Outcomes
Equipment
Patient preparation
The patient’s health is considered by comprehensive blood tests, EKG, and other assessment tests to determine the patient’s plans for surgery appropriateness.
Patients must discuss the risks, advantages, and alternatives and obtain consent.
An anesthesia consultation is necessary to discuss with the surgeon; general and local anesthesia can be used.
Patient position
The preferred position is the supine position.
Conventional Carotid Endarterectomy
Step 1: Patient Preparation:
The patient will be placed on an operating table which will often require an individual to lie facing up marking his or her back.
Anesthesia is administered to the patients, usually the general anesthesia.
Site of operation, often neck, undergoes a surgical cleansing and preparing of the site.
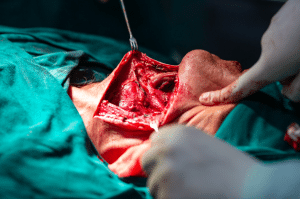
Step 2: Incision:
The surgeon makes the incision frontally on neck, either on the affected side or on the side where the stenosis is manifested.
Usually, the incision is done vertically along the skin’s natural lines, which promotes faster wound healing and reduces scarring.
Step 3: Exposing the Carotid Artery
Therefore, when the incision is made, the surgeon uses delicate action to part the tissue, skin after skin, and other exposed muscles to expose the carotid artery.
During the bypass procedure, specialized surgical instruments and retractors ensure that the tissues don’t prevent clear access to the artery.
Step 4: Temporary Clamping:
To stop the blood flow during the process and provide a clear surgical field, the surgeon simply presses on the carotid artery both below (closer to the heart) and upstream (away from the heart) of the narrowed region.
Step 5: Incision of the Artery
After clamping, the surgeon carefully makes a small incision in the carotid artery directly above the plaque buildup, taking care to minimise bleeding and prevent damage to the arterial walls.
Step 6: Plaque Removal:
Using specialized, appropriate tools, the surgeon meticulously removes the plaque deposited on the inner margin of the carotid arteries.
There are different methods of removing the plaque, including scraping (endarterectomy), cutting (endarterectomy with patch angioplasty), and eversion.
Step 7: Closure:
Then, the plaque is covered, and the carotid artery is incised. Sutures are used to close the wounds under sterilized conditions.
It is even possible to patch the artery, which will decrease the risk of restenosis.
Step 8: Postoperative Care:
The patient is usually observed continuously in the recovery room for any signals of complications like bleeding or nerve function.
Aftercare instructions for pain management and preventing complications are provided, e.g., blood clots or infections.
Eversion Endarterectomy
Step 1: Anesthesia and incision:
A general anesthesia is set to numb the area and works against the patient´s pain during surgery.
To expose the carotid artery, perform a small horizontal incision in the neck just beneath the jawline.
Step 2: Arterial exposure and clamping:
Taking all precautions, the surgeon proceeds into the skin and muscles and separates the artery bifurcated ends into the internal and external carotid arteries.
To block blood flow through the common carotid artery (CCA), ICA, and ECA, temporary clamps are placed on these blood arteries.
Step 3: ICA Transection and Plaque Eversion
In contrast to the traditional endarterectomy, the eversion technique slices the ICA diagonally at the bifurcation, incorporating a bit of the CCA. This creates a “fish mouth” opening at the ICA.
With the ICA being cut the plaque build-up on the inside wall is also exposed.
The surgeon uses the forceps to gradually pull out the arterial layer that is on the outside of ICA. As if this arterial layer is everting itself, it is over on the plaque. This allows for the visual Plaque removal from ICA and CCA:
Keeping the same position, the surgeon is precise as tears off ICA plaques with the tip of the forceps.
Whether gradually or rapidly, the CCA is stretched to the extent that the extension of the arteriotomy sometimes allows plaque to be entirely removed from the vessel.
Step 4: Closure and blood flow restoration:
Ultimately, after the CCA has been entirely separated from the ICA, both blood vessels are included, the everted ICA is joined with the opposite end of the CCA (the ICA is placed on the inside of the CCA).
In case of performing CCA arteriotomy (opening the hole in the large artery through which blood flows from the heart to the brain), the same cut will be made on ICA anastomosis (connection of an artery/blood vessel).
The clamps are removed temporarily to let blood flow in the carotid arteries overcome the irregularity.
The area is rinsed using the heparinized saline solution to dislodge clots in blood.
Then the wound is concealed one layer after another with stitches.
Step 5: Shunt considerations
Sometimes, a temporary graft (shunt) is used to bypass the artery during the procedure to keep blood flow to the brain while the plaque is being removed from the carotid artery.
The main reason for choosing a shunt is based on factors such as the patient’s medical history, the degree of carotid artery stenosis (narrowing), and whether the blood flow can be interrupted for a long time.
Laboratory tests
Complications

Carotid endarterectomy (CEA) is a surgical procedure carried out to clear plaque out of the carotid arteries. These are the major blood vessels that lie in the neck, connecting the neck to the brain and providing the later with oxygen-rich blood. This is one of the surgical measures used in patients who suffer a high degree of blockage in their carotid arteries (carotid artery stenosis), which predisposes them to stroke attacks.
Carotid Endarterectomy
CEA is frequently done to prevent a stroke in patients who suffer from TIAs or minor strokes and who also have the carotid artery with more blockages known through diagnostic tests, like carotid ultrasound or MRA.
The patient’s health is considered by comprehensive blood tests, EKG, and other assessment tests to determine the patient’s plans for surgery appropriateness.
Patients must discuss the risks, advantages, and alternatives and obtain consent.
An anesthesia consultation is necessary to discuss with the surgeon; general and local anesthesia can be used.
Patient position
The preferred position is the supine position.
Step 1: Patient Preparation:
The patient will be placed on an operating table which will often require an individual to lie facing up marking his or her back.
Anesthesia is administered to the patients, usually the general anesthesia.
Site of operation, often neck, undergoes a surgical cleansing and preparing of the site.
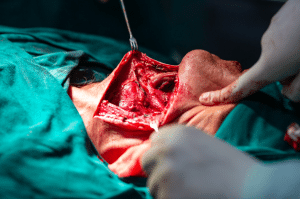
Step 2: Incision:
The surgeon makes the incision frontally on neck, either on the affected side or on the side where the stenosis is manifested.
Usually, the incision is done vertically along the skin’s natural lines, which promotes faster wound healing and reduces scarring.
Step 3: Exposing the Carotid Artery
Therefore, when the incision is made, the surgeon uses delicate action to part the tissue, skin after skin, and other exposed muscles to expose the carotid artery.
During the bypass procedure, specialized surgical instruments and retractors ensure that the tissues don’t prevent clear access to the artery.
Step 4: Temporary Clamping:
To stop the blood flow during the process and provide a clear surgical field, the surgeon simply presses on the carotid artery both below (closer to the heart) and upstream (away from the heart) of the narrowed region.
Step 5: Incision of the Artery
After clamping, the surgeon carefully makes a small incision in the carotid artery directly above the plaque buildup, taking care to minimise bleeding and prevent damage to the arterial walls.
Step 6: Plaque Removal:
Using specialized, appropriate tools, the surgeon meticulously removes the plaque deposited on the inner margin of the carotid arteries.
There are different methods of removing the plaque, including scraping (endarterectomy), cutting (endarterectomy with patch angioplasty), and eversion.
Step 7: Closure:
Then, the plaque is covered, and the carotid artery is incised. Sutures are used to close the wounds under sterilized conditions.
It is even possible to patch the artery, which will decrease the risk of restenosis.
Step 8: Postoperative Care:
The patient is usually observed continuously in the recovery room for any signals of complications like bleeding or nerve function.
Aftercare instructions for pain management and preventing complications are provided, e.g., blood clots or infections.
Step 1: Anesthesia and incision:
A general anesthesia is set to numb the area and works against the patient´s pain during surgery.
To expose the carotid artery, perform a small horizontal incision in the neck just beneath the jawline.
Step 2: Arterial exposure and clamping:
Taking all precautions, the surgeon proceeds into the skin and muscles and separates the artery bifurcated ends into the internal and external carotid arteries.
To block blood flow through the common carotid artery (CCA), ICA, and ECA, temporary clamps are placed on these blood arteries.
Step 3: ICA Transection and Plaque Eversion
In contrast to the traditional endarterectomy, the eversion technique slices the ICA diagonally at the bifurcation, incorporating a bit of the CCA. This creates a “fish mouth” opening at the ICA.
With the ICA being cut the plaque build-up on the inside wall is also exposed.
The surgeon uses the forceps to gradually pull out the arterial layer that is on the outside of ICA. As if this arterial layer is everting itself, it is over on the plaque. This allows for the visual Plaque removal from ICA and CCA:
Keeping the same position, the surgeon is precise as tears off ICA plaques with the tip of the forceps.
Whether gradually or rapidly, the CCA is stretched to the extent that the extension of the arteriotomy sometimes allows plaque to be entirely removed from the vessel.
Step 4: Closure and blood flow restoration:
Ultimately, after the CCA has been entirely separated from the ICA, both blood vessels are included, the everted ICA is joined with the opposite end of the CCA (the ICA is placed on the inside of the CCA).
In case of performing CCA arteriotomy (opening the hole in the large artery through which blood flows from the heart to the brain), the same cut will be made on ICA anastomosis (connection of an artery/blood vessel).
The clamps are removed temporarily to let blood flow in the carotid arteries overcome the irregularity.
The area is rinsed using the heparinized saline solution to dislodge clots in blood.
Then the wound is concealed one layer after another with stitches.
Step 5: Shunt considerations
Sometimes, a temporary graft (shunt) is used to bypass the artery during the procedure to keep blood flow to the brain while the plaque is being removed from the carotid artery.
The main reason for choosing a shunt is based on factors such as the patient’s medical history, the degree of carotid artery stenosis (narrowing), and whether the blood flow can be interrupted for a long time.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



