Background
Catheter ablation is a minimally invasive procedure. It is used to treat a several kinds of cardiac abnormalities. It includes inserting thin and flexible catheters tubes into the heart via blood arteries.
This procedure is performed by cardiologists and electrophysiologists. They are specialist in heart rhythm abnormalities in an advanced cardiac catheterization laboratory known as a cath lab.
Indications
Atrial Fibrillation (AF): Patients who have symptomatic AF and are not responding to the antiarrhythmic drugs and those who are sensitive to them, catheter ablation may be suggested to those.
Supraventricular Tachycardias: Conditions like atrioventricular nodal reentrant tachycardia (AVNRT) or Wolff-Parkinson-White syndrome, which do not respond to medications, are suggested for catheter ablation.
Ventricular Tachycardia (VT): Patients who have recurrent VT episodes, specifically those who are hemodynamically unstable or not responding to antiarrhythmic drugs or sensitive to them, are suggested for catheter ablation.
Atrial Flutter: It is a condition with abnormal heart rhythm. It is often treated with catheter ablation procedure. It is used specifically in those cases where drugs are not effective or lead to severe side effects.
Accessory Pathways: Patients who have accessory pathways, like those who have Wolff-Parkinson-White syndrome, need to eliminate the abnormal electrical connection between the ventricles and atria with the help of a catheter ablation procedure.
Long QT Syndrome: Some cases of long QT syndrome in which medications are not enough to treat arrhythmias, catheter ablation procedure can be suggested.
Arrhythmias in Structural Heart Disease: Patients who have arrhythmias along with certain structural heart defects or disease like hypertrophic cardiomyopathy, catheter ablation procedure is used to treat arrhythmias.
Contraindications
Presence of Intracardiac Thrombi: The most significant risk of embolization throughout the procedure is the presence of blood clots within the heart.
Severe Uncontrolled Bleeding Disorders: High risk of bleeding complications because of the improper blood coagulation.
Severe Vascular Disease: Difficulty to reach to the heart because of the blocked or restricted blood vessels.
Mechanical Heart Valves: These are not often safe to cross with catheter ablation in most cases.
Outcomes
Equipment
Catheters: There are many types of catheters are used like diagnostic catheters and ablation catheters. Diagnostic catheters are used to map the electrical activity of the heart. Ablation catheters are used to apply energy to produce lesions in the heart tissues.
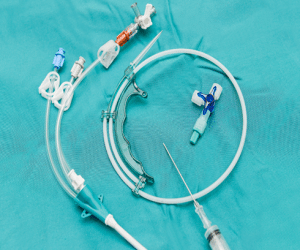
Catheters
Electrophysiology System: This system involves the EP recording systems. It records and displays the electrical signals of the heart. The EP stimulation system sends electrical impulses to heart to cause arrhythmias to diagnose.
Mapping System: This system produces informative map of the electrical activity of heart. This can help to identify the areas which are needed to be ablated.
Radiofrequency Ablation Generator: This device produces high frequency energy on the tip of the ablation catheters. It produces controlled lesion on the heart tissues.
Cryoablation System: Some procedures utilize a cryoablation system instead of RF energy. It generates freezing temperature to produce lesions on the heart tissues.
Navigation System: This system provides direction to catheters in the heart chambers with accuracy with the use of 3D mapping technology.
Anesthesia Equipment: Medications and monitoring devices are used to make sure the comfort and safety of the patients throughout the procedure.
Patient preparation
Pre-procedure Evaluation:
A cardiologist or electrophysiologist operates a thorough comprehensive examination of the patients. It is necessary to confirm the use of catheter ablation and to evaluate the overall health status of the patient.
This examination may include the physical examination, review of medical history, blood tests, echocardiogram, electrocardiogram (ECG), and other imaging tests.
Medication Management:
To reduce the risk of bleeding problems or complications, patient may need to temporarily stop certain medications like blood thinners or antiplatelet medications before the procedure. Other medications which are taken by patients should be reviewed and adjusted as of need.
Fasting:
Fasting is necessary for a specific time, typically overnight fasting before the procedure. This decreases the risk of aspiration during the anesthesia or sedation.
Informed Consent:
Complete information of the operation like risks, advantages, and available options must be provided to patients before taking their consent. They can ask questions regarding this.
Pre-procedure Instructions:
Patients must be given specific instructions about what to do in the days during the procedure and, after that, avoid certain foods and beverages, avoid alcohol or tobacco, and avoid intense activities.
Clothing and Personal Items:
Patients should wear comfortable clothes. They should leave valuable things at home. They should remove jewellery, watches, and metal objects before the procedure.
Approach considerations
2 to 5 electrode catheters are inserted directly through the internal jugular or femoral veins into the left ventricle, right ventricle, or both.
Many catheters are needed to induce and map many tachyarrhythmias before RFCA.
Coronary sinus cannulation may help to map the left-sided auxiliary route and assess the left-sided tachyarrhythmia substrates like atrial fibrillation.
To perform catheterization the left heart, practitioners may select between 2 alternatives:
Atrial fibrillation technique
Step 1: Ablation of AV junction with radiofrequency catheter ablation is the most fundamental procedure for patients who have atrial fibrillation.
Step 2: The standard procedure for catheter ablation of atrial fibrillation for atrial tissue is a large circumferential ablation of the pulmonary veins.
Step 3: The aim is to successfully isolate the fast electrical impulses that originate within the vein or around the entrance of the pulmonary veins and to separate them from the adjacent areas of the left atrium.
Step 4: Catheter ablation is more effective than the antiarrhythmic medication treatment to treat atrial fibrillation. It is used specifically in cases of former has failed earlier.
Step 5: The comprehensive surgical Maze procedure includes the atrial incisions with or without the transmural RF damages has been shown the most effective method. It is useful for atrial fibrillation patients without regard to the duration of condition or presence of structural heart disease.
Ventricular tachycardia
Step 1: Ablation is a viable treatment option for ventricular tachycardia in structural heart disease.
Step 2: In these complex ablations, a 3D electroanatomic mapping is used to find the scar which are responsible for the anatomical that drives re-entry.
Step 3: Pre-procedural imaging using MRI or CT scan is used in some cases. It is used as intracardiac echocardiography during the procedure.
Step 4: The anatomical data which are derived by imaging techniques can be utilized into an electroanatomic map as per need.
Step 5: Certain ventricular tachycardia substrates, specifically those prevalent in nonischemic cardiomyopathy cases, may be undetected by the endocardium.
Step 6: In those cases, ablation and percutaneous epicardial mapping is required.
Wolff-Parkinson-White syndrome
Step 1: Patient who has Wolff-Parkinson-White syndrome, atrial fibrillation may lead to irregular large complex tachycardia. This can be pre-excited and may lead to ventricular fibrillation.
Step 2: This may lead to potential fatal quick anterograde conduction with the accessory circuit.
Step 3: ORP may start in patients with WPW syndrome along with atrial fibrillation.
Step 4: Most patients with WPW syndrome have atrial fibrillation and eliminate ORT by accessory pathway ablation.
Orthodromic reciprocating tachycardia
Step 1: The AV node acts as the anterograde limb in ORP. AV connection acts as the retrograde limb.
Step 2: An accessory pathways is considered as concealed if it is only performed retrogradely. It cannot be detected on an ECG in sinus rhythm.
Step 3: Target the accessory channel as it moves across the annulus of the tricuspid and mitral valves is often useful to treat ORT.
Complications
Bleeding (hematoma): There is a risk of bleeding at the catheter insertion site. This may lead to hematoma formation.
Blood vessel damage: The catheter insertion can damage the blood vessels in rare cases.
Infection: There may be a risk of infection at the site of catheter insertion or within the heart.
Blood clot formation: There may be a risk of blood clot formation in the heart or blood vessels. This may lead to stroke or other complications.
Pulmonary vein stenosis: Pulmonary veins may narrowed after the ablation which can lead to difficulty in breathing in some cases.
Perforation or puncture of the heart: there is a small risk of puncturing or perforating the heart wall during the procedure.

Catheter ablation is a minimally invasive procedure. It is used to treat a several kinds of cardiac abnormalities. It includes inserting thin and flexible catheters tubes into the heart via blood arteries.
This procedure is performed by cardiologists and electrophysiologists. They are specialist in heart rhythm abnormalities in an advanced cardiac catheterization laboratory known as a cath lab.
Atrial Fibrillation (AF): Patients who have symptomatic AF and are not responding to the antiarrhythmic drugs and those who are sensitive to them, catheter ablation may be suggested to those.
Supraventricular Tachycardias: Conditions like atrioventricular nodal reentrant tachycardia (AVNRT) or Wolff-Parkinson-White syndrome, which do not respond to medications, are suggested for catheter ablation.
Ventricular Tachycardia (VT): Patients who have recurrent VT episodes, specifically those who are hemodynamically unstable or not responding to antiarrhythmic drugs or sensitive to them, are suggested for catheter ablation.
Atrial Flutter: It is a condition with abnormal heart rhythm. It is often treated with catheter ablation procedure. It is used specifically in those cases where drugs are not effective or lead to severe side effects.
Accessory Pathways: Patients who have accessory pathways, like those who have Wolff-Parkinson-White syndrome, need to eliminate the abnormal electrical connection between the ventricles and atria with the help of a catheter ablation procedure.
Long QT Syndrome: Some cases of long QT syndrome in which medications are not enough to treat arrhythmias, catheter ablation procedure can be suggested.
Arrhythmias in Structural Heart Disease: Patients who have arrhythmias along with certain structural heart defects or disease like hypertrophic cardiomyopathy, catheter ablation procedure is used to treat arrhythmias.
Presence of Intracardiac Thrombi: The most significant risk of embolization throughout the procedure is the presence of blood clots within the heart.
Severe Uncontrolled Bleeding Disorders: High risk of bleeding complications because of the improper blood coagulation.
Severe Vascular Disease: Difficulty to reach to the heart because of the blocked or restricted blood vessels.
Mechanical Heart Valves: These are not often safe to cross with catheter ablation in most cases.
Catheters: There are many types of catheters are used like diagnostic catheters and ablation catheters. Diagnostic catheters are used to map the electrical activity of the heart. Ablation catheters are used to apply energy to produce lesions in the heart tissues.
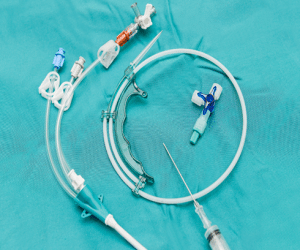
Catheters
Electrophysiology System: This system involves the EP recording systems. It records and displays the electrical signals of the heart. The EP stimulation system sends electrical impulses to heart to cause arrhythmias to diagnose.
Mapping System: This system produces informative map of the electrical activity of heart. This can help to identify the areas which are needed to be ablated.
Radiofrequency Ablation Generator: This device produces high frequency energy on the tip of the ablation catheters. It produces controlled lesion on the heart tissues.
Cryoablation System: Some procedures utilize a cryoablation system instead of RF energy. It generates freezing temperature to produce lesions on the heart tissues.
Navigation System: This system provides direction to catheters in the heart chambers with accuracy with the use of 3D mapping technology.
Anesthesia Equipment: Medications and monitoring devices are used to make sure the comfort and safety of the patients throughout the procedure.
Pre-procedure Evaluation:
A cardiologist or electrophysiologist operates a thorough comprehensive examination of the patients. It is necessary to confirm the use of catheter ablation and to evaluate the overall health status of the patient.
This examination may include the physical examination, review of medical history, blood tests, echocardiogram, electrocardiogram (ECG), and other imaging tests.
Medication Management:
To reduce the risk of bleeding problems or complications, patient may need to temporarily stop certain medications like blood thinners or antiplatelet medications before the procedure. Other medications which are taken by patients should be reviewed and adjusted as of need.
Fasting:
Fasting is necessary for a specific time, typically overnight fasting before the procedure. This decreases the risk of aspiration during the anesthesia or sedation.
Informed Consent:
Complete information of the operation like risks, advantages, and available options must be provided to patients before taking their consent. They can ask questions regarding this.
Pre-procedure Instructions:
Patients must be given specific instructions about what to do in the days during the procedure and, after that, avoid certain foods and beverages, avoid alcohol or tobacco, and avoid intense activities.
Clothing and Personal Items:
Patients should wear comfortable clothes. They should leave valuable things at home. They should remove jewellery, watches, and metal objects before the procedure.
2 to 5 electrode catheters are inserted directly through the internal jugular or femoral veins into the left ventricle, right ventricle, or both.
Many catheters are needed to induce and map many tachyarrhythmias before RFCA.
Coronary sinus cannulation may help to map the left-sided auxiliary route and assess the left-sided tachyarrhythmia substrates like atrial fibrillation.
To perform catheterization the left heart, practitioners may select between 2 alternatives:
Step 1: Ablation of AV junction with radiofrequency catheter ablation is the most fundamental procedure for patients who have atrial fibrillation.
Step 2: The standard procedure for catheter ablation of atrial fibrillation for atrial tissue is a large circumferential ablation of the pulmonary veins.
Step 3: The aim is to successfully isolate the fast electrical impulses that originate within the vein or around the entrance of the pulmonary veins and to separate them from the adjacent areas of the left atrium.
Step 4: Catheter ablation is more effective than the antiarrhythmic medication treatment to treat atrial fibrillation. It is used specifically in cases of former has failed earlier.
Step 5: The comprehensive surgical Maze procedure includes the atrial incisions with or without the transmural RF damages has been shown the most effective method. It is useful for atrial fibrillation patients without regard to the duration of condition or presence of structural heart disease.
Step 1: Ablation is a viable treatment option for ventricular tachycardia in structural heart disease.
Step 2: In these complex ablations, a 3D electroanatomic mapping is used to find the scar which are responsible for the anatomical that drives re-entry.
Step 3: Pre-procedural imaging using MRI or CT scan is used in some cases. It is used as intracardiac echocardiography during the procedure.
Step 4: The anatomical data which are derived by imaging techniques can be utilized into an electroanatomic map as per need.
Step 5: Certain ventricular tachycardia substrates, specifically those prevalent in nonischemic cardiomyopathy cases, may be undetected by the endocardium.
Step 6: In those cases, ablation and percutaneous epicardial mapping is required.
Step 1: Patient who has Wolff-Parkinson-White syndrome, atrial fibrillation may lead to irregular large complex tachycardia. This can be pre-excited and may lead to ventricular fibrillation.
Step 2: This may lead to potential fatal quick anterograde conduction with the accessory circuit.
Step 3: ORP may start in patients with WPW syndrome along with atrial fibrillation.
Step 4: Most patients with WPW syndrome have atrial fibrillation and eliminate ORT by accessory pathway ablation.
Step 1: The AV node acts as the anterograde limb in ORP. AV connection acts as the retrograde limb.
Step 2: An accessory pathways is considered as concealed if it is only performed retrogradely. It cannot be detected on an ECG in sinus rhythm.
Step 3: Target the accessory channel as it moves across the annulus of the tricuspid and mitral valves is often useful to treat ORT.
Bleeding (hematoma): There is a risk of bleeding at the catheter insertion site. This may lead to hematoma formation.
Blood vessel damage: The catheter insertion can damage the blood vessels in rare cases.
Infection: There may be a risk of infection at the site of catheter insertion or within the heart.
Blood clot formation: There may be a risk of blood clot formation in the heart or blood vessels. This may lead to stroke or other complications.
Pulmonary vein stenosis: Pulmonary veins may narrowed after the ablation which can lead to difficulty in breathing in some cases.
Perforation or puncture of the heart: there is a small risk of puncturing or perforating the heart wall during the procedure.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



