Background
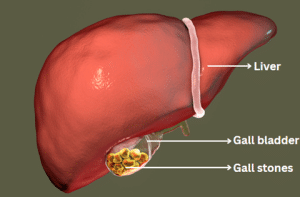
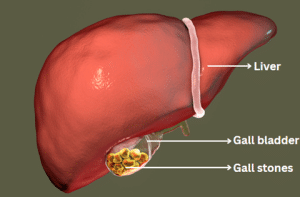
Cholecystectomy is procedure to remove the gallbladder. Gallbladder is a pear-shaped organ and it is located beneath the liver. It stores bile. Cholecystectomy is a common procedure which is performed to treat the gallbladder related conditions line inflammation, infection, or gallstones. This procedure can be performed using the traditional open surgery or minimally invasive technique like laparoscopic cholecystectomy.
Cholecystectomy has a long history, which began in the 19th century. The first successful cholecystectomy procedure was performed in 1882 by a German surgeon, Carl Langenbuch. He has performed the procedure on a 43-year-old female with symptomatic gallstones. This technique involved an open surgical approach and established the foundation for the modern cholecystectomy procedure.
Development in surgical technology and techniques have improved the cholecystectomy results and decreased the risks which are associated with the procedure over the time. The laparoscopic cholecystectomy procedure was introduced in late 1980. It has revolutionized the gallbladder surgery. This minimally invasive technique utilizes small incisions and a camera to see the surgical area and, resulting in a quick recovery time and less post-operative pain than the open surgery.
Cholecystectomy has become one of the most performed surgical procedure globally. It is a safe and effective procedure for gallbladder disease with a low risk of complications. Cholecystectomy has also some risks like bleeding, infection or injury to the nearby organs like other surgery. These risks are low, and many patients can recover after the surgery.
Cholecystectomy is now one of the most performed surgical procedures worldwide. It is regarded a safe and effective procedure for gallbladder disease, with a low risk of complications. However, like any surgical procedure, cholecystectomy carries some risks which include bleeding, infection, and injury to surrounding organs. These risks are low, and most patients recover well after surgery.
Cholecystectomy (gallbladder removal)
Indications
Gallstones: Cholecystectomy is suggested for symptomatic gallstones, specifically if they lead to recurrence episodes of pain (biliary colic), complications like pancreatitis, or inflammation (cholecystitis).
Acute Cholecystitis: Inflammation of the gallbladder because of the gallstones, which can cause severe abdominal pain, infection, and pain. Cholecystectomy is performed in cases of acute cholecystitis, specifically if the disease is recurrent or severe.
Chronic Cholecystitis: Prolonged inflammation of the gallbladder, which may be a result of repeated episodes of acute cholecystitis. Cholecystectomy is suggested to prevent ongoing inflammation and complications.
Gallbladder Polyps: Small lesions or growth in the gallbladder wall known as gallbladder polyps. Most polyps are benign. Large polyps or those with some specific symptoms may need cholecystectomy because of the risk of malignancy.
Gallbladder Dyskinesia: Gallbladder Dyskinesia is a condition with the symptoms of abnormal gallbladder emptying. It can lead to symptoms which are like gallstones. Cholecystectomy is suggested if the symptoms are severe and do not respond to the any other treatment.
Porcelain Gallbladder: Porcelain Gallbladder is a condition where the gallbladder wall becomes calcified and is associated with chronic inflammation. Cholecystectomy is suggested because of the elevated risk of gallbladder cancer.
Gallbladder Cancer: Cholecystectomy is the primary procedure for early-stage gallbladder cancer. Other additional treatments like chemotherapy and radiation therapy can be needed in some cases.
Choledocholithiasis: Choledocholithiasis is a condition where gallstones are present in the bile duct. This can lead to complications like pancreatitis or obstructive jaundice. Cholecystectomy may be suggested with the other procedures to extract the stones from the bile duct.
Contraindications
Severe Cardiovascular Disease: Patients who have severe cardiovascular disease like unstable angina, decompensated heart failure, or recent myocardial infarction can be at increased risk during the surgery. In such cases, the advantages of cholecystectomy must be properly balanced with the risks.
Severe Pulmonary Disease: Patients who have severe chronic obstructive pulmonary disease (COPD), severe asthma, or other severe lung diseases may have an elevated risk of complications during the procedure and anesthesia.
Severe Coagulopathy: Patients who have severe bleeding disorders or have an anticoagulant treatment that is not safely terminated may be at risk of bleeding during the procedure.
Pregnancy: Cholecystectomy is avoided during the pregnancy, specifically in the first trimester. It is because of the potential risks to the fetus. If the surgery is necessary, then it is delayed until the delivery, if possible, in some cases.
Acute Pancreatitis: Cholecystectomy may be delayed in cases of acute pancreatitis since pancreatitis has been resolved to lower the risk of complications.
Severe Systemic Infection: Patients who have severe systemic infections may be at elevated risk of complications from procedure and anesthesia.
Unstable Patient Condition: Patients who have other severe medical diseases or are medically unstable, which can make the procedure unsafe, may not be performed on those patients.
Outcomes
Symptom Relief: Cholecystectomy is a highly effective procedure that can relieve the symptoms which are associated with gallbladder disease, like nausea, vomiting, and abdominal pain, specifically in cases of chronic cholecystitis or gallstones.
Prevention of Complications: The risk of complications which are linked with gallstones like choledocholithiasis (stones in the bile ducts), pancreatitis, and cholecystitis (inflammation of the gallbladder) reduced by removing the gallbladder.
Improved Quality of Life: Patients who undergo the cholecystectomy procedure may experience an improvement in their life because of the relief of symptoms and ability to do the normal activities without any fear of gallstone related complications
Low Rate of Complications: Cholecystectomy is linked with a rate of complications like bleeding, bile duct injury, infection, and bile leakage, specifically performed laparoscopically by experienced surgeons.
Short Hospital Stay: Most patients who undergo laparoscopic cholecystectomy procedure can be discharged from the hospital within a day or two days of surgery. It can lead to quicker recovery than open surgery.
Low Rate of Recurrence: Cholecystectomy is an ultimate treatment for gallstones, with a low rate of recurrence after surgery.
Improved Long-Term Outcomes: Studies have shown that cholecystectomy may lead to improved long-term results, including a lowered risk of developing gallbladder cancer, specifically in patients who have a history of gallstones.
Equipment
Laparoscope: A laparoscope is a thin and lighted tube with a camera which enables the surgeon to see the inside the abdomen during laparoscopic cholecystectomy. It is inserted via a small incision in the abdomen and gives a magnified view of the gallbladder and other structures.
Trocar: Trocars are long and hollow tubes which are inserted into the small incisions in the abdomen to give access for surgical instruments during the laparoscopic cholecystectomy. They function as ports for the laparoscope and other equipment.
Grasping Forceps: Grasping forceps are used to manipulate and grasp tissues during the procedure. Grasping forceps are inserted via trocars and allow the surgeon to hold and move the gallbladder and other structures as per the need.
Dissecting Instruments: Dissecting instruments like graspers, dissectors, and scissors are used to separate the gallbladder from the liver and surrounding tissues. This equipment is inserted via trocars and used to dissect and free the gallbladder to remove.
Clip Applier: Clip appliers are used to ligate and secure the artery and cystic duct which are blood vessels which supply the blood to gallbladder. Clips are used to prevent bleeding and make sure that the ducts are sealed off before the removal of gallbladder.
Electrocautery Device: An electrocautery device is used to cut and coagulate the tissues during the procedure. It helps to control bleeding and make sure a clean dissection of the gallbladder from the liver.
Suction Irrigation System: A suction irrigation system is used to remove the excess debris and fluid from the surgical sites and provide better visibility to the surgeon and reduce the risk of infection.
Specimen Retrieval Bag: The gallbladder is removed intact via one of the trocar incisions in laparoscopic cholecystectomy. A specimen retrieval bag is used to place the gallbladder during removal and reduce the risk of spillage and contamination.
Retractors: Retractors are used to hold back the tissues and organs to provide good access and visibility during the procedure. It comes in different shapes and sizes. It can be used to retract the liver, bile duct, and ither structures as per the need.
Surgical Drapes and Sterile Supplies: Sterile surgical drapes and supplies are used to keep a sterile filed during the procedure and lower the risk of infection.
Patient preparation
Pre-operative Assessment: The patient goes for a comprehensive pre-operative assessment before the procedure. This includes current medications, review of medical history, allergies, and any other relevant imaging studies or laboratory tests.
Education and Informed Consent: The patient is given a detailed information about the procedure which include purpose. Risk, benefit. And alternative. They have an opportunity to ask question and give informed consent for the procedure.
Fasting: Patient are instructed to not eat or drink for a specific period of time before the procedure. Fasting requires at least 6 to 8 hours before the procedure to lower the risk of aspiration during anesthesia.
Medication Management: Medications of patients may need to be adjusted before the procedure, specifically those which are taken for blood thinning or other medication which can increase the risk of bleeding during the procedure. The healthcare provider will give specific instructions on medications to discontinue or continue before the procedure.
Bowel Preparation: The patient can be instructed to go for bowel preparation to empty the intestines in some cases, specifically for open cholecystectomy or if any concern about bowel obstruction. This can include taking laxatives or enemas as prescribed by healthcare providers.
Anesthesia Evaluation: The patient goes for an assessment by an anesthesiologist to assess anesthesia for the procedure. This can include regional or general anesthesia like spinal or epidural anesthesia.
Pre-operative Skin Preparation: The patient can be asked to shower using an antiseptic soap to lower the risk of surgical area infections on the day of procedure.
Intravenous (IV) Access: IV access is determined to administer medication and fluid during the procedure. This can allow to deliver anesthesia. Antibiotics, and other medications as per the need.
Patient Positioning: To make sure the comfort and safety of patient during the procedure, they are positioned on the operating table to provide maximum and best access to the surgical site.
Pre-operative Monitoring: The vital signs of a patient, like blood pressure, oxygen saturation, and heart rate, are monitored closely to make sure they are stable before the procedure starts.
Open cholecystectomy
Step 1 – Patient Preparation: General anesthesia is given when the patient is lying supine on the operating table. The abdomen is prepped and covered in a sterile cover to reduce the risk of infection.
Step 2 – Incision: The surgeon makes a skin incision in the upper abdomen, specifically below the right costal margin or in the midline. It is dependent on the anatomy pf patient and preference of the surgeon. This incision can vary in length but is typically around 10 to 15 cm.
Step 3 – Exploration of the Abdominal Cavity: After making the incision, the surgeon carefully dissects via layers of tissue to access the abdominal cavity. Then, the surgeon uses retractors to provide proper exposure to the surgical field.
Step 4 – Identification of the Gallbladder: The surgeon first identifies the gallbladder and then seperate it from the surrounding structures carefully which include liver, common liver duct, and duodenum. This can include dissecting adhesions and ligating small blood vessels.
Step 5 – Dissection of the Cystic Duct and Artery: The artery and cystic duct are connected to the gallbladder to the hepatic artery and common bile duct, respectively. They are isolated and ligated. This step is important to make sure the complete removal of the gallbladder without any damage to the nearby structures.
Step 6 – Gallbladder Removal: The surgeon dissects the gallbladder away from the liver bed with the cystic duct and artery ligated. Surgical clips or electrocautery can be used to control the bleeding during this process. Through the incision, the gallbladder is removed from the abdomen.
Step 7 – Closure: The surgeon closes the incision the layers, once the hemostasis confirms and there is no bile leaks. The fascia and abdominal muscles are closed with absorbable sutures. The skin can be closed with staples, sutures, or adhesive strips.
Step 8 – Drains (Optional): A drain can be placed near the surgical area to remove any blood or fluid that accumulates after the operation. The decision to place a drain depends on the preference of surgeon and circumstance of patient.
Step 9 – Dressing and Post-operative Care: A sterile covering is applied to the wound after the incision is closed. The patient is transferred to the recovery area. Post-operative care is given, like pain management, monitoring the complications like bile leakage or infection, and early mobilization to prevent any complications like deep vein thrombosis.
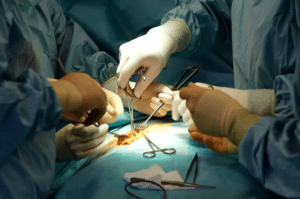
Open cholecystectomy
Laparoscopic cholecystectomy
Step 1 – Patient Preparation: The patient is placed supine on the operating table. General anesthesia is given. CO2 gas is utilized to inflate the abdomen, create a space for the surgical instruments, and provide better visualization of the surgical field.
Step 2 – Placement of Trocars: The surgeon makes many small incisions of 5 to 10 mm in length in the abdominal wall. Trocars are hollow tubes with valves inserted via these incisions to give access for surgical instruments and camera.
Step 3 – Creation of Pneumoperitoneum: CO2 gas is pumped into the abdomen via one of the trocars to create a pneumoperitoneum. This can lift the abdominal wall away from the internal organs and allow better visuals and manipulation.
Step 4 – Insertion of Laparoscope: A laparoscope is inserted via one of the trocars. The camera provides a magnified view of the abdominal cavity on the monitor. This allows the surgeon to see inside the body without a large incision.
Step 5 – Identification of Anatomy: The surgeon identified the anatomical structures in the abdomen which includes liver, gallbladder, cystic duct, common bile duct, and blood vessels. This step is important to make sure the effective and safe removal of gallbladder without any damage to the nearby structures.
Step 6 – Dissection of Cystic Duct and Artery: The surgeon dissects and clips the artery and cystic duct by using the specialized instruments which are inserted via the remaining trocars. This step isolates the gallbladder from the blood supply and biliary tree.
Step 7 – Gallbladder Mobilization and Extraction: The surgeon continues to dissect and separate the gallbladder from the liver bed by using the ultrasonic energy or electrocautery. Once freed, the gallbladder is carefully removed via one of the trocar incisions. Sometimes retrieval bags are used to minimize the spillage of debris and bile.
Step 8 – Inspection and Hemostasis: The surgeon inspects the surgical site for any bile leakage of bleeding after the removal of gallbladder. Any bleeding vessels are clipped or cauterized to gain hemostasis and the area is thoroughly irrigated with saline to remove any bile or debris.
Step 9 – Closure of Incisions: Once the hemostasis is gain and surgical site is clean, the trocars are removed, and incisions are sealed with absorbable sutures or surgical glue. A single incision can be used from the removal of gallbladder which can result in a smaller scar in some cases.
Step 10 – Dressing and Post-operative Care: A sterile dressing is applied to the incision areas. The patient is transferred to the recovery area. Post-operative care is given to manage the pain, early mobilization, and to monitor any complications like bile leakage or infection.
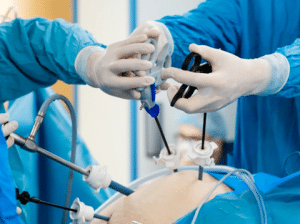
Laparoscopic cholecystectomy
Complications
Bleeding: There is a risk of bleeding during the procedure, specifically if the blood vessels are accidentally injured during dissection or clipping of the artery and cystic duct. Bleeding can be controlled by clips or electrocautery in some cases. In severe bleeding, it may require the switch to an open procedure or transfusion.
Bile Duct Injury: Any damage to the bile ducts which can occur during the manipulation or dissection of the gallbladder or nearby structures is a serious complication of laparoscopic cholecystectomy. Bile ducts injuries may result in infection, bile leakage, bile duct strictures, and other intervention.
Bile Leak: If the cystic duct stump or common bile duct is not properly sealed or if an accidental injury to the bile ducts occurred during the surgery, the bile leak can occur. This can lead to infection. Abdominal pain, and peritonitis and this may need drainage and repair procedures.
Biliary Colic: Some patients can experience recurrent episodes of biliary colic with the symptoms of abdominal pain and discomfort after the laparoscopic cholecystectomy. This can happen if the gallstones are present in the common bile duct or if the sphincter or Oddie becomes dysfunctional after the surgery.
Infection: Infections with the abdominal cavity or at the surgical area is a potential complication of surgery. Proper sterile techniques and pre-operative antibiotics can reduce the risk of infection. Though, it can occur and need treatment with antibiotics or drainage procedures.
Wound Complications: Complications which are linked to the incision sites are infection, seroma, hematoma, or delayed wound healing may happen after the laparoscopic cholecystectomy. Proper wound care and monitoring the patient is important to prevent and manage the complications.
Pneumoperitoneum-related Complications: The pneumoperitoneum during laparoscopic surgery may lead to complications like pneumomediastinum, pneumothorax, or subcutaneous emphysema. These complications are rare but if they occur, specifically patients who have lung disease or compromised respiratory function.
Cardiopulmonary Complications: Laparoscopic cholecystectomy is linked with a lower risk of cardiopulmonary complications than open surgery. Patients who have cardiac or respiratory conditions may be at elevated risk for complications like arrhythmias, pulmonary embolism, or myocardial infarction.
Rare Complications: Rare complications of laparoscopic cholecystectomy are injury to adjacent organs (like the liver, intestines, or pancreas), retained stones in the bile ducts, post-cholecystectomy syndrome, and anesthesia-related complications.

Cholecystectomy is procedure to remove the gallbladder. Gallbladder is a pear-shaped organ and it is located beneath the liver. It stores bile. Cholecystectomy is a common procedure which is performed to treat the gallbladder related conditions line inflammation, infection, or gallstones. This procedure can be performed using the traditional open surgery or minimally invasive technique like laparoscopic cholecystectomy.
Cholecystectomy has a long history, which began in the 19th century. The first successful cholecystectomy procedure was performed in 1882 by a German surgeon, Carl Langenbuch. He has performed the procedure on a 43-year-old female with symptomatic gallstones. This technique involved an open surgical approach and established the foundation for the modern cholecystectomy procedure.
Development in surgical technology and techniques have improved the cholecystectomy results and decreased the risks which are associated with the procedure over the time. The laparoscopic cholecystectomy procedure was introduced in late 1980. It has revolutionized the gallbladder surgery. This minimally invasive technique utilizes small incisions and a camera to see the surgical area and, resulting in a quick recovery time and less post-operative pain than the open surgery.
Cholecystectomy has become one of the most performed surgical procedure globally. It is a safe and effective procedure for gallbladder disease with a low risk of complications. Cholecystectomy has also some risks like bleeding, infection or injury to the nearby organs like other surgery. These risks are low, and many patients can recover after the surgery.
Cholecystectomy is now one of the most performed surgical procedures worldwide. It is regarded a safe and effective procedure for gallbladder disease, with a low risk of complications. However, like any surgical procedure, cholecystectomy carries some risks which include bleeding, infection, and injury to surrounding organs. These risks are low, and most patients recover well after surgery.
Cholecystectomy (gallbladder removal)
Gallstones: Cholecystectomy is suggested for symptomatic gallstones, specifically if they lead to recurrence episodes of pain (biliary colic), complications like pancreatitis, or inflammation (cholecystitis).
Acute Cholecystitis: Inflammation of the gallbladder because of the gallstones, which can cause severe abdominal pain, infection, and pain. Cholecystectomy is performed in cases of acute cholecystitis, specifically if the disease is recurrent or severe.
Chronic Cholecystitis: Prolonged inflammation of the gallbladder, which may be a result of repeated episodes of acute cholecystitis. Cholecystectomy is suggested to prevent ongoing inflammation and complications.
Gallbladder Polyps: Small lesions or growth in the gallbladder wall known as gallbladder polyps. Most polyps are benign. Large polyps or those with some specific symptoms may need cholecystectomy because of the risk of malignancy.
Gallbladder Dyskinesia: Gallbladder Dyskinesia is a condition with the symptoms of abnormal gallbladder emptying. It can lead to symptoms which are like gallstones. Cholecystectomy is suggested if the symptoms are severe and do not respond to the any other treatment.
Porcelain Gallbladder: Porcelain Gallbladder is a condition where the gallbladder wall becomes calcified and is associated with chronic inflammation. Cholecystectomy is suggested because of the elevated risk of gallbladder cancer.
Gallbladder Cancer: Cholecystectomy is the primary procedure for early-stage gallbladder cancer. Other additional treatments like chemotherapy and radiation therapy can be needed in some cases.
Choledocholithiasis: Choledocholithiasis is a condition where gallstones are present in the bile duct. This can lead to complications like pancreatitis or obstructive jaundice. Cholecystectomy may be suggested with the other procedures to extract the stones from the bile duct.
Severe Cardiovascular Disease: Patients who have severe cardiovascular disease like unstable angina, decompensated heart failure, or recent myocardial infarction can be at increased risk during the surgery. In such cases, the advantages of cholecystectomy must be properly balanced with the risks.
Severe Pulmonary Disease: Patients who have severe chronic obstructive pulmonary disease (COPD), severe asthma, or other severe lung diseases may have an elevated risk of complications during the procedure and anesthesia.
Severe Coagulopathy: Patients who have severe bleeding disorders or have an anticoagulant treatment that is not safely terminated may be at risk of bleeding during the procedure.
Pregnancy: Cholecystectomy is avoided during the pregnancy, specifically in the first trimester. It is because of the potential risks to the fetus. If the surgery is necessary, then it is delayed until the delivery, if possible, in some cases.
Acute Pancreatitis: Cholecystectomy may be delayed in cases of acute pancreatitis since pancreatitis has been resolved to lower the risk of complications.
Severe Systemic Infection: Patients who have severe systemic infections may be at elevated risk of complications from procedure and anesthesia.
Unstable Patient Condition: Patients who have other severe medical diseases or are medically unstable, which can make the procedure unsafe, may not be performed on those patients.
Symptom Relief: Cholecystectomy is a highly effective procedure that can relieve the symptoms which are associated with gallbladder disease, like nausea, vomiting, and abdominal pain, specifically in cases of chronic cholecystitis or gallstones.
Prevention of Complications: The risk of complications which are linked with gallstones like choledocholithiasis (stones in the bile ducts), pancreatitis, and cholecystitis (inflammation of the gallbladder) reduced by removing the gallbladder.
Improved Quality of Life: Patients who undergo the cholecystectomy procedure may experience an improvement in their life because of the relief of symptoms and ability to do the normal activities without any fear of gallstone related complications
Low Rate of Complications: Cholecystectomy is linked with a rate of complications like bleeding, bile duct injury, infection, and bile leakage, specifically performed laparoscopically by experienced surgeons.
Short Hospital Stay: Most patients who undergo laparoscopic cholecystectomy procedure can be discharged from the hospital within a day or two days of surgery. It can lead to quicker recovery than open surgery.
Low Rate of Recurrence: Cholecystectomy is an ultimate treatment for gallstones, with a low rate of recurrence after surgery.
Improved Long-Term Outcomes: Studies have shown that cholecystectomy may lead to improved long-term results, including a lowered risk of developing gallbladder cancer, specifically in patients who have a history of gallstones.
Laparoscope: A laparoscope is a thin and lighted tube with a camera which enables the surgeon to see the inside the abdomen during laparoscopic cholecystectomy. It is inserted via a small incision in the abdomen and gives a magnified view of the gallbladder and other structures.
Trocar: Trocars are long and hollow tubes which are inserted into the small incisions in the abdomen to give access for surgical instruments during the laparoscopic cholecystectomy. They function as ports for the laparoscope and other equipment.
Grasping Forceps: Grasping forceps are used to manipulate and grasp tissues during the procedure. Grasping forceps are inserted via trocars and allow the surgeon to hold and move the gallbladder and other structures as per the need.
Dissecting Instruments: Dissecting instruments like graspers, dissectors, and scissors are used to separate the gallbladder from the liver and surrounding tissues. This equipment is inserted via trocars and used to dissect and free the gallbladder to remove.
Clip Applier: Clip appliers are used to ligate and secure the artery and cystic duct which are blood vessels which supply the blood to gallbladder. Clips are used to prevent bleeding and make sure that the ducts are sealed off before the removal of gallbladder.
Electrocautery Device: An electrocautery device is used to cut and coagulate the tissues during the procedure. It helps to control bleeding and make sure a clean dissection of the gallbladder from the liver.
Suction Irrigation System: A suction irrigation system is used to remove the excess debris and fluid from the surgical sites and provide better visibility to the surgeon and reduce the risk of infection.
Specimen Retrieval Bag: The gallbladder is removed intact via one of the trocar incisions in laparoscopic cholecystectomy. A specimen retrieval bag is used to place the gallbladder during removal and reduce the risk of spillage and contamination.
Retractors: Retractors are used to hold back the tissues and organs to provide good access and visibility during the procedure. It comes in different shapes and sizes. It can be used to retract the liver, bile duct, and ither structures as per the need.
Surgical Drapes and Sterile Supplies: Sterile surgical drapes and supplies are used to keep a sterile filed during the procedure and lower the risk of infection.
Pre-operative Assessment: The patient goes for a comprehensive pre-operative assessment before the procedure. This includes current medications, review of medical history, allergies, and any other relevant imaging studies or laboratory tests.
Education and Informed Consent: The patient is given a detailed information about the procedure which include purpose. Risk, benefit. And alternative. They have an opportunity to ask question and give informed consent for the procedure.
Fasting: Patient are instructed to not eat or drink for a specific period of time before the procedure. Fasting requires at least 6 to 8 hours before the procedure to lower the risk of aspiration during anesthesia.
Medication Management: Medications of patients may need to be adjusted before the procedure, specifically those which are taken for blood thinning or other medication which can increase the risk of bleeding during the procedure. The healthcare provider will give specific instructions on medications to discontinue or continue before the procedure.
Bowel Preparation: The patient can be instructed to go for bowel preparation to empty the intestines in some cases, specifically for open cholecystectomy or if any concern about bowel obstruction. This can include taking laxatives or enemas as prescribed by healthcare providers.
Anesthesia Evaluation: The patient goes for an assessment by an anesthesiologist to assess anesthesia for the procedure. This can include regional or general anesthesia like spinal or epidural anesthesia.
Pre-operative Skin Preparation: The patient can be asked to shower using an antiseptic soap to lower the risk of surgical area infections on the day of procedure.
Intravenous (IV) Access: IV access is determined to administer medication and fluid during the procedure. This can allow to deliver anesthesia. Antibiotics, and other medications as per the need.
Patient Positioning: To make sure the comfort and safety of patient during the procedure, they are positioned on the operating table to provide maximum and best access to the surgical site.
Pre-operative Monitoring: The vital signs of a patient, like blood pressure, oxygen saturation, and heart rate, are monitored closely to make sure they are stable before the procedure starts.
Step 1 – Patient Preparation: General anesthesia is given when the patient is lying supine on the operating table. The abdomen is prepped and covered in a sterile cover to reduce the risk of infection.
Step 2 – Incision: The surgeon makes a skin incision in the upper abdomen, specifically below the right costal margin or in the midline. It is dependent on the anatomy pf patient and preference of the surgeon. This incision can vary in length but is typically around 10 to 15 cm.
Step 3 – Exploration of the Abdominal Cavity: After making the incision, the surgeon carefully dissects via layers of tissue to access the abdominal cavity. Then, the surgeon uses retractors to provide proper exposure to the surgical field.
Step 4 – Identification of the Gallbladder: The surgeon first identifies the gallbladder and then seperate it from the surrounding structures carefully which include liver, common liver duct, and duodenum. This can include dissecting adhesions and ligating small blood vessels.
Step 5 – Dissection of the Cystic Duct and Artery: The artery and cystic duct are connected to the gallbladder to the hepatic artery and common bile duct, respectively. They are isolated and ligated. This step is important to make sure the complete removal of the gallbladder without any damage to the nearby structures.
Step 6 – Gallbladder Removal: The surgeon dissects the gallbladder away from the liver bed with the cystic duct and artery ligated. Surgical clips or electrocautery can be used to control the bleeding during this process. Through the incision, the gallbladder is removed from the abdomen.
Step 7 – Closure: The surgeon closes the incision the layers, once the hemostasis confirms and there is no bile leaks. The fascia and abdominal muscles are closed with absorbable sutures. The skin can be closed with staples, sutures, or adhesive strips.
Step 8 – Drains (Optional): A drain can be placed near the surgical area to remove any blood or fluid that accumulates after the operation. The decision to place a drain depends on the preference of surgeon and circumstance of patient.
Step 9 – Dressing and Post-operative Care: A sterile covering is applied to the wound after the incision is closed. The patient is transferred to the recovery area. Post-operative care is given, like pain management, monitoring the complications like bile leakage or infection, and early mobilization to prevent any complications like deep vein thrombosis.
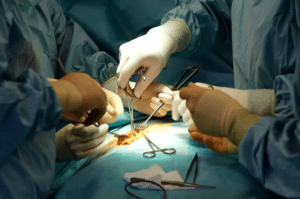
Open cholecystectomy
Step 1 – Patient Preparation: The patient is placed supine on the operating table. General anesthesia is given. CO2 gas is utilized to inflate the abdomen, create a space for the surgical instruments, and provide better visualization of the surgical field.
Step 2 – Placement of Trocars: The surgeon makes many small incisions of 5 to 10 mm in length in the abdominal wall. Trocars are hollow tubes with valves inserted via these incisions to give access for surgical instruments and camera.
Step 3 – Creation of Pneumoperitoneum: CO2 gas is pumped into the abdomen via one of the trocars to create a pneumoperitoneum. This can lift the abdominal wall away from the internal organs and allow better visuals and manipulation.
Step 4 – Insertion of Laparoscope: A laparoscope is inserted via one of the trocars. The camera provides a magnified view of the abdominal cavity on the monitor. This allows the surgeon to see inside the body without a large incision.
Step 5 – Identification of Anatomy: The surgeon identified the anatomical structures in the abdomen which includes liver, gallbladder, cystic duct, common bile duct, and blood vessels. This step is important to make sure the effective and safe removal of gallbladder without any damage to the nearby structures.
Step 6 – Dissection of Cystic Duct and Artery: The surgeon dissects and clips the artery and cystic duct by using the specialized instruments which are inserted via the remaining trocars. This step isolates the gallbladder from the blood supply and biliary tree.
Step 7 – Gallbladder Mobilization and Extraction: The surgeon continues to dissect and separate the gallbladder from the liver bed by using the ultrasonic energy or electrocautery. Once freed, the gallbladder is carefully removed via one of the trocar incisions. Sometimes retrieval bags are used to minimize the spillage of debris and bile.
Step 8 – Inspection and Hemostasis: The surgeon inspects the surgical site for any bile leakage of bleeding after the removal of gallbladder. Any bleeding vessels are clipped or cauterized to gain hemostasis and the area is thoroughly irrigated with saline to remove any bile or debris.
Step 9 – Closure of Incisions: Once the hemostasis is gain and surgical site is clean, the trocars are removed, and incisions are sealed with absorbable sutures or surgical glue. A single incision can be used from the removal of gallbladder which can result in a smaller scar in some cases.
Step 10 – Dressing and Post-operative Care: A sterile dressing is applied to the incision areas. The patient is transferred to the recovery area. Post-operative care is given to manage the pain, early mobilization, and to monitor any complications like bile leakage or infection.
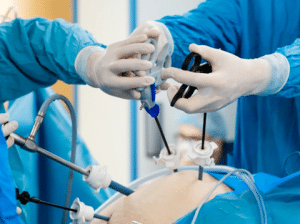
Laparoscopic cholecystectomy
Bleeding: There is a risk of bleeding during the procedure, specifically if the blood vessels are accidentally injured during dissection or clipping of the artery and cystic duct. Bleeding can be controlled by clips or electrocautery in some cases. In severe bleeding, it may require the switch to an open procedure or transfusion.
Bile Duct Injury: Any damage to the bile ducts which can occur during the manipulation or dissection of the gallbladder or nearby structures is a serious complication of laparoscopic cholecystectomy. Bile ducts injuries may result in infection, bile leakage, bile duct strictures, and other intervention.
Bile Leak: If the cystic duct stump or common bile duct is not properly sealed or if an accidental injury to the bile ducts occurred during the surgery, the bile leak can occur. This can lead to infection. Abdominal pain, and peritonitis and this may need drainage and repair procedures.
Biliary Colic: Some patients can experience recurrent episodes of biliary colic with the symptoms of abdominal pain and discomfort after the laparoscopic cholecystectomy. This can happen if the gallstones are present in the common bile duct or if the sphincter or Oddie becomes dysfunctional after the surgery.
Infection: Infections with the abdominal cavity or at the surgical area is a potential complication of surgery. Proper sterile techniques and pre-operative antibiotics can reduce the risk of infection. Though, it can occur and need treatment with antibiotics or drainage procedures.
Wound Complications: Complications which are linked to the incision sites are infection, seroma, hematoma, or delayed wound healing may happen after the laparoscopic cholecystectomy. Proper wound care and monitoring the patient is important to prevent and manage the complications.
Pneumoperitoneum-related Complications: The pneumoperitoneum during laparoscopic surgery may lead to complications like pneumomediastinum, pneumothorax, or subcutaneous emphysema. These complications are rare but if they occur, specifically patients who have lung disease or compromised respiratory function.
Cardiopulmonary Complications: Laparoscopic cholecystectomy is linked with a lower risk of cardiopulmonary complications than open surgery. Patients who have cardiac or respiratory conditions may be at elevated risk for complications like arrhythmias, pulmonary embolism, or myocardial infarction.
Rare Complications: Rare complications of laparoscopic cholecystectomy are injury to adjacent organs (like the liver, intestines, or pancreas), retained stones in the bile ducts, post-cholecystectomy syndrome, and anesthesia-related complications.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



