Background
Debridement plays a crucial role in the management of orbital mucormycosis, a severe fungal infection that often involves the sinuses and orbit, and can rapidly progress to threaten life and vision. Mucormycosis, primarily caused by fungi from the order Mucorales, can lead to aggressive tissue necrosis, particularly in immunocompromised individuals, such as those with uncontrolled diabetes or those recovering from COVID-19. The infection typically starts in the sinuses and spreads to the orbit, causing inflammation, necrosis, and potential loss of vision.
Traditionally, the treatment of orbital mucormycosis involves a combination of antifungal therapy with amphotericin B and surgical interventions, including debridement. The primary goal of debridement is to remove necrotic, infected tissue to halt the progression of the infection and prevent further damage to the eye and surrounding structures. Debridement helps to reduce the fungal burden, improve the penetration of antifungal drugs, and promote tissue healing.
In the past, extensive debridement often involved radical procedures such as orbital exenteration, the removal of the eye and all surrounding tissues, to control the infection. However, this approach can cause significant cosmetic disfigurement and psychological distress. More recent studies and techniques have focused on less invasive debridement methods, such as localized debridement of the infected tissues without removing the entire orbit. These approaches, combined with targeted antifungal therapy (like the instillation of amphotericin B gel directly into the infected area), aim to preserve the eye and vision while effectively managing the infection.
Indications
Post-COVID-19 Rhino-Orbital Mucormycosis: Localized debridement was indicated in cases of rhino-orbital mucormycosis in patients recovering from COVID-19 infection.
Presence of Necrotic Tissue: When MRI imaging and clinical evaluation reveal necrotic tissue in the orbit or surrounding areas, localized debridement is indicated to remove the infected tissue and allow better penetration of antifungal therapy.
Non-Exenteration Candidates: For patients who wish to preserve their eye and avoid the radical procedure of orbital exenteration, localized debridement with targeted antifungal therapy (e.g., amphotericin B gel) is a viable option.
Absence of Orbital Apex Syndrome: In cases where orbital apex syndrome is not present or when the infection is not advancing towards the brain, localized debridement is preferred to manage the infection without resorting to exenteration.

Edema in the left eye
Contraindications
Severe Orbital Apex Syndrome: If the infection has spread to the orbital apex and caused significant neurological deficits (e.g., involvement of the third, fourth, sixth cranial nerves, and optic nerve), localized debridement may not be sufficient, and orbital exenteration might be required to prevent intracranial spread.
Inability to Safely Access Infection Sites: If the infected tissue is located in areas that are difficult to reach through minimally invasive surgical techniques (e.g., deep in the orbital apex or highly advanced spread to the cavernous sinus), localized debridement may not be feasible.
Lack of Adequate Medical Therapy Support: If systemic antifungal therapy (e.g., amphotericin B) is not accessible or effective, localized debridement without appropriate antifungal treatment could be ineffective in controlling the infection, making it contraindicated.
Extensive Disease Involving Both Orbit and Brain: If the disease has extensively spread beyond the orbit into the brain or other vital structures, more aggressive treatment, including orbital exenteration, might be necessary to prevent further complications.
Outcomes
Equipment
Nasal Endoscopy – To evaluate the nasal passages and identify any suspicious crust or black necrotic tissue, which was sent for microbiology testing.
MRI and CT scans – Used to assess the extent of the disease in the orbit and surrounding structures (e.g., sinuses and brain).
Incision Tools:
Transconjunctival inferior orbitotomy
Surgical Instruments:
Injection Syringe and Needle:
Amphotericin B Gel (Lipid-Based, 0.1% w/w) – Applied locally at the site of debridement for fungal treatment.
Patient Preparation
Patient preparation for localized orbital debridement includes a thorough preoperative evaluation with a detailed history, ophthalmic and otolaryngologic examination, and imaging (MRI and CT) to assess the extent of the infection. Blood glucose and haemoglobin A1c levels are monitored, and nasal endoscopy is performed for microbiological evaluation. Informed consent is obtained, explaining the procedure, potential risks, and the option of orbital exenteration. Antifungal treatment, including the use of amphotericin B gel, is planned. The patient is positioned supine with appropriate incisions for accessing the affected orbital areas.
Patient Position
Supine Position: The patient is placed in a supine position on the operating table, with the head stabilized.
Head Tilt: A slight tilt of the head may be employed depending on the site of infection, to enhance access to the orbit.
Eye Exposure: The affected eye is prepared for surgery, and the eyelid is retracted to ensure clear visualization of the orbital structures.
Technique
Step 1-Patient Evaluation and Imaging: Detailed history and clinical evaluation, including systemic conditions such as diabetes, hypertension, or any other comorbidities. Ophthalmic and otorhinolaryngologic evaluations to assess the extent of the disease. Nasal endoscopy to check for suspicious crust or black necrotic tissue, which is then sent for microbiological testing. MRI scans of the orbits, sinuses, and brain (with CT correlation) are performed to localize fungal infection and assess orbital involvement.
Step 2-Preoperative Considerations: Blood glucose levels and glycosylated hemoglobin are checked, as they can affect healing and treatment outcomes. Systemic amphotericin B therapy is started to treat mucormycosis once diagnosed, after a test dose and monitoring for side effects (renal function).
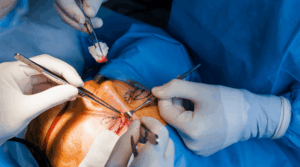
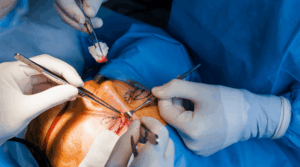
Step 3-Surgical Approach:
Incision: Depending on the location of fungal involvement: A lid crease incision is used for accessing the superomedial and medial parts of the orbit.
An inferior transconjunctival incision is made for accessing the inferior orbit, followed by opening the periorbita to reach the infraorbital fissure.
Debridement: The surgeon carefully removes all necrotic and infected tissue from the involved areas (infraorbital fissure, superomedial region, medial orbit, and the soft tissue around the orbital floor).
Amphotericin B Gel: Lipid-based amphotericin B gel (0.1% w/w) is injected at the site of debridement using a 5-cc syringe and 18-G 1.5-inch needle to ensure direct drug delivery to the infected tissue.
Step 4-Postoperative Care:
Systemic amphotericin B is continued for 3 weeks, followed by a step-down therapy with oral posaconazole for 3 months. Patients are monitored for any signs of complications, such as lid edema or conjunctival chemosis, which are common but typically resolve within 7 days. Post-debridement imaging (MRI) is done at regular intervals (e.g., 3 weeks after surgery) to assess resolution of the infection.
Step 5-Follow-Up: Continuous follow-up for 1–5 months, with regular monitoring for clinical improvement, such as resolution of diplopia, ptosis, and proptosis. In cases of partia
Approach considerations
Localized surgical debridement for orbital mucormycosis aims to remove necrotic tissue while preserving vision and avoiding exenteration. A multidisciplinary approach involving ophthalmology, ENT, and infectious disease specialists is crucial. Preoperative MRI/CT helps define the extent of infection. Surgical access varies based on involvement—transconjunctival, lid crease, or medial orbitotomy approaches are used for targeted debridement. The periorbita is incised, and necrotic fat, muscles, and infected tissues are excised. Intraoperative antifungal instillation (liposomal amphotericin B 0.1%) enhances local control. Postoperatively, IV liposomal amphotericin B followed by oral posaconazole, regular imaging, and renal function monitoring are essential. Exenteration is reserved for extensive disease with intracranial extension or orbital apex involvement. Early intervention improves outcomes and prevents vision loss.
Laboratory tests
KOH Mount & Calcofluor White Stain – Rapid fungal detection.
Fungal Culture & PCR – Identifies Mucorales species.
Histopathology (H&E, PAS, GMS Stains) – Confirms fungal invasion.
CBC – Assesses leukocytosis/neutropenia.
Serum Glucose & HbA1c – Evaluates diabetes control.
Renal (BUN, Creatinine) & Liver Function Tests (LFTs) – Monitors antifungal toxicity.
Inflammatory Markers (CRP, ESR, PCT) – Indicates disease severity.

Debridement plays a crucial role in the management of orbital mucormycosis, a severe fungal infection that often involves the sinuses and orbit, and can rapidly progress to threaten life and vision. Mucormycosis, primarily caused by fungi from the order Mucorales, can lead to aggressive tissue necrosis, particularly in immunocompromised individuals, such as those with uncontrolled diabetes or those recovering from COVID-19. The infection typically starts in the sinuses and spreads to the orbit, causing inflammation, necrosis, and potential loss of vision.
Traditionally, the treatment of orbital mucormycosis involves a combination of antifungal therapy with amphotericin B and surgical interventions, including debridement. The primary goal of debridement is to remove necrotic, infected tissue to halt the progression of the infection and prevent further damage to the eye and surrounding structures. Debridement helps to reduce the fungal burden, improve the penetration of antifungal drugs, and promote tissue healing.
In the past, extensive debridement often involved radical procedures such as orbital exenteration, the removal of the eye and all surrounding tissues, to control the infection. However, this approach can cause significant cosmetic disfigurement and psychological distress. More recent studies and techniques have focused on less invasive debridement methods, such as localized debridement of the infected tissues without removing the entire orbit. These approaches, combined with targeted antifungal therapy (like the instillation of amphotericin B gel directly into the infected area), aim to preserve the eye and vision while effectively managing the infection.
Post-COVID-19 Rhino-Orbital Mucormycosis: Localized debridement was indicated in cases of rhino-orbital mucormycosis in patients recovering from COVID-19 infection.
Presence of Necrotic Tissue: When MRI imaging and clinical evaluation reveal necrotic tissue in the orbit or surrounding areas, localized debridement is indicated to remove the infected tissue and allow better penetration of antifungal therapy.
Non-Exenteration Candidates: For patients who wish to preserve their eye and avoid the radical procedure of orbital exenteration, localized debridement with targeted antifungal therapy (e.g., amphotericin B gel) is a viable option.
Absence of Orbital Apex Syndrome: In cases where orbital apex syndrome is not present or when the infection is not advancing towards the brain, localized debridement is preferred to manage the infection without resorting to exenteration.

Edema in the left eye
Severe Orbital Apex Syndrome: If the infection has spread to the orbital apex and caused significant neurological deficits (e.g., involvement of the third, fourth, sixth cranial nerves, and optic nerve), localized debridement may not be sufficient, and orbital exenteration might be required to prevent intracranial spread.
Inability to Safely Access Infection Sites: If the infected tissue is located in areas that are difficult to reach through minimally invasive surgical techniques (e.g., deep in the orbital apex or highly advanced spread to the cavernous sinus), localized debridement may not be feasible.
Lack of Adequate Medical Therapy Support: If systemic antifungal therapy (e.g., amphotericin B) is not accessible or effective, localized debridement without appropriate antifungal treatment could be ineffective in controlling the infection, making it contraindicated.
Extensive Disease Involving Both Orbit and Brain: If the disease has extensively spread beyond the orbit into the brain or other vital structures, more aggressive treatment, including orbital exenteration, might be necessary to prevent further complications.
Nasal Endoscopy – To evaluate the nasal passages and identify any suspicious crust or black necrotic tissue, which was sent for microbiology testing.
MRI and CT scans – Used to assess the extent of the disease in the orbit and surrounding structures (e.g., sinuses and brain).
Incision Tools:
Transconjunctival inferior orbitotomy
Surgical Instruments:
Injection Syringe and Needle:
Amphotericin B Gel (Lipid-Based, 0.1% w/w) – Applied locally at the site of debridement for fungal treatment.
Patient preparation for localized orbital debridement includes a thorough preoperative evaluation with a detailed history, ophthalmic and otolaryngologic examination, and imaging (MRI and CT) to assess the extent of the infection. Blood glucose and haemoglobin A1c levels are monitored, and nasal endoscopy is performed for microbiological evaluation. Informed consent is obtained, explaining the procedure, potential risks, and the option of orbital exenteration. Antifungal treatment, including the use of amphotericin B gel, is planned. The patient is positioned supine with appropriate incisions for accessing the affected orbital areas.
Supine Position: The patient is placed in a supine position on the operating table, with the head stabilized.
Head Tilt: A slight tilt of the head may be employed depending on the site of infection, to enhance access to the orbit.
Eye Exposure: The affected eye is prepared for surgery, and the eyelid is retracted to ensure clear visualization of the orbital structures.
Step 1-Patient Evaluation and Imaging: Detailed history and clinical evaluation, including systemic conditions such as diabetes, hypertension, or any other comorbidities. Ophthalmic and otorhinolaryngologic evaluations to assess the extent of the disease. Nasal endoscopy to check for suspicious crust or black necrotic tissue, which is then sent for microbiological testing. MRI scans of the orbits, sinuses, and brain (with CT correlation) are performed to localize fungal infection and assess orbital involvement.
Step 2-Preoperative Considerations: Blood glucose levels and glycosylated hemoglobin are checked, as they can affect healing and treatment outcomes. Systemic amphotericin B therapy is started to treat mucormycosis once diagnosed, after a test dose and monitoring for side effects (renal function).
Step 3-Surgical Approach:
Incision: Depending on the location of fungal involvement: A lid crease incision is used for accessing the superomedial and medial parts of the orbit.
An inferior transconjunctival incision is made for accessing the inferior orbit, followed by opening the periorbita to reach the infraorbital fissure.
Debridement: The surgeon carefully removes all necrotic and infected tissue from the involved areas (infraorbital fissure, superomedial region, medial orbit, and the soft tissue around the orbital floor).
Amphotericin B Gel: Lipid-based amphotericin B gel (0.1% w/w) is injected at the site of debridement using a 5-cc syringe and 18-G 1.5-inch needle to ensure direct drug delivery to the infected tissue.
Step 4-Postoperative Care:
Systemic amphotericin B is continued for 3 weeks, followed by a step-down therapy with oral posaconazole for 3 months. Patients are monitored for any signs of complications, such as lid edema or conjunctival chemosis, which are common but typically resolve within 7 days. Post-debridement imaging (MRI) is done at regular intervals (e.g., 3 weeks after surgery) to assess resolution of the infection.
Step 5-Follow-Up: Continuous follow-up for 1–5 months, with regular monitoring for clinical improvement, such as resolution of diplopia, ptosis, and proptosis. In cases of partia
Localized surgical debridement for orbital mucormycosis aims to remove necrotic tissue while preserving vision and avoiding exenteration. A multidisciplinary approach involving ophthalmology, ENT, and infectious disease specialists is crucial. Preoperative MRI/CT helps define the extent of infection. Surgical access varies based on involvement—transconjunctival, lid crease, or medial orbitotomy approaches are used for targeted debridement. The periorbita is incised, and necrotic fat, muscles, and infected tissues are excised. Intraoperative antifungal instillation (liposomal amphotericin B 0.1%) enhances local control. Postoperatively, IV liposomal amphotericin B followed by oral posaconazole, regular imaging, and renal function monitoring are essential. Exenteration is reserved for extensive disease with intracranial extension or orbital apex involvement. Early intervention improves outcomes and prevents vision loss.
Laboratory tests
KOH Mount & Calcofluor White Stain – Rapid fungal detection.
Fungal Culture & PCR – Identifies Mucorales species.
Histopathology (H&E, PAS, GMS Stains) – Confirms fungal invasion.
CBC – Assesses leukocytosis/neutropenia.
Serum Glucose & HbA1c – Evaluates diabetes control.
Renal (BUN, Creatinine) & Liver Function Tests (LFTs) – Monitors antifungal toxicity.
Inflammatory Markers (CRP, ESR, PCT) – Indicates disease severity.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



