Background
Electroconvulsive therapy also known as ECT is a method that is commonly used in handling severe psychiatric illnesses especially for those who have not responded well to other treatments. It incorporates convulsions using electric shocks to the brain for seizure control and even this approach is considered despite its controversial history and stigma it is a conventionally efficient medical practice that can save many lives.
History of Electroconvulsive Therapy
This method has been known in the early part of the 20th century when European psychiatrists noted that there were seemingly positive changes in major psychopathological symptoms in people with epilepsy. ECT is a treatment developed in 1938 with schizophrenic patients by Italian neuropsychiatrist Ugo Cerletti and Lucio Bini but then applied to other psychosexual disorders. ECT has been approved and applied for Depression, Bipolar disorder, and Catatonic schizophrenia in the twentieth century, however in the mid-twentieth century it was considered as barbaric.
Indications
Major Depressive Disorder (MDD)
Bipolar Disorder
Schizophrenia
Catatonia
Acute Agitation
Neurological Conditions
Pregnancy
Contraindications
It is not appropriate to conduct ECT for those patients who suffered from myocardial infarction earlier since the risk of cardiologic complications is rather high.
Any intracranial lesions are absolutely contraindicated for ECT because it actually raises intracranial pressure and also potential neurological problems.
If there are recent history of stroke and severe osteoporosis, as these states could bring about further neurological complications in the course of ECT treatment; contractions and movements during seizures might expose such patients to possible fractures.
ECT is not given at the same time period after a prior treatment to reduce the possibility of adverse effects.
Outcomes
Patient preparation
These include equipment setup and positioning, choice of electrodes, the anesthetic procedure, pharmacological neuromuscular blockade, comorbidity aspects, obtaining consent from patients, and special cases of caring for pregnant women, children, and the elderly when receiving ECT, with the aim of avoiding undesirable outcomes in the treatment process.
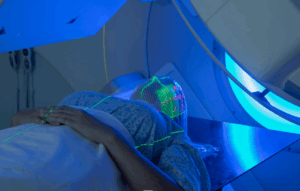
Equipment Setup:
Proper set up of the ECT equipment formulates part of the safety measure of the patient as well as plays a critical role in the treatment process. It should consist of a ECT machine, electrodes for administering the shock, a stimulus parameter controller, monitoring devices and equipment for the emergencies.
Electrode Placement:
The position of electrodes determines the current flow and efficacy of the ECT. Electrode placement, Both A and B In some patients the initial placement is carried out according to certain well-defined protocols with reference to the clinical manifestation of the patient and the goals of treatment.
Anesthesia:
Anesthesia is given for safety and to prevent pain during the process. However, general anaesthesia incorporating muscle relaxation is preferred during the deliberate induction of seizures possibly to prevent physical injury.
Beta Blockade:
The use of beta-adrenergic blockers can be combined with anticholinergic agents, with the approach that this might help to dampen the cardiovascular effect of ECT seizures. Antiarrhythmic drugs like propofol or esmolol may be used to decrease the incidence of heart rate and the systolic blood pressure during ECT decreasing the chance of re-entry, myocardial ischemia and other cardiac consequences.
Informed Consent:
It is one of the procedures used within the framework of the ECT process and consists in informing the patient in detail about all the possible consequences of the treatment and the possible benefits, as well as other available methods within the specialization of the clinic. It is important that the patient, their family members, and the treatment team including the psychiatrist agree on whether the patient should go for ECT or not depending on their perceived goals of treatment.
Electroconvulsive Therapy in pediatrics:
ECT is limited in child and adolescent populations. However, it may be used when the patient has not responded to other therapies or has some contraindication to standard medications. ECT is used rarely in children and adolescents when prescribed. The mental age, cognitive comprehension ability, and voluntary consent capacity of the child should be considered during treatment.
Electroconvulsive Therapy in Pregnancy:
Pregnant patients could also be considered as candidates for ECT in the event of severe psychiatric illness; nonetheless, this must be done while taking into the risks that might affect the fetus as well as the benefits for the mother. The choice of giving ECT when the patient is pregnant should, therefore, involve a risk-benefit analysis that considers factors such as the nature of the illness that the woman is suffering from, the dangers of leaving the psychiatric illness untreated, and the various risks associated with ECT.
Electroconvulsive Therapy
Technique of electroconvulsive therapy
Step:1-Seizure Quality: An induced seizure in ECT can possess a certain quality, which has a direct activity on the effectiveness of the treatment process. A tonic clonic seizure, which is a convulsion seizure that includes stiffening of muscles and temporary loss of consciousness, has been reported to have a favourable prognosis. The seizure threshold is the minimum stimulus intensity needed to elicit a seizure, it also differs among different patients and may be affected by some variables such as age, sex, medical condition and the co administration of other drugs. During each ECT administration procedure, clinical parameters as well as EEG and motor seizure evaluation is conducted to ensure that an appropriate seizure is generated for treatment.
Step:2-Frequency of Treatments: ECT is typically administered during a specific course, and the number of treatments depends on patients’ specific conditions, goals, or plan of further treatment. Typically, ECT is given on a two to three times weekly basis during the initial phase of the treatment to attain the intended effect of alleviating the symptoms. The number of frequency per session may be altered depending on the patient’s progress thus some may need more therapy to achieve maximum results. If there is enough improvement, the ECT sessions also become less frequent and are given on a weekly or biweekly basis for continuation/maintenance treatment to lessen relapse.
Step:3-Total Number of ECT Treatments: To carry out the electric shock treatment, the patient may be given several treatments based on the condition or illness that they are suffering from and its severity, and the plan of treatment to be taken for their specific case of illness. Evaluations of acute phase of ECT commonly are delivered in the range of six to twelve sessions; however, some patients might need less or more session depending on the severity of their condition. Maintenance ECT can be defined as a continuation and augmentation of the treatment course to consolidate the therapeutic outcome and avoid relapse, which may require delivering the treatments at a lesser frequency but for a longer duration. ECT is conducted repeatedly in a course of maintenance in patients with high risk for relapse, untreated earlier, and those experiencing psychiatric symptoms at present. Since the indications for ECT depend upon the initial responsiveness of the patient to treatment and the degree of symptom severity, the two need to be assessed on a regular basis to determine whether ECT should be continued or not.
Step 4: Continuation and Maintenance Electroconvulsive Therapy:
Therapy, continuation, and maintenance ECT are critical parameters of the long-term management of patients with recurrent/chronic psychiatric disorders. Maintenance ECT, on the other hand, entails the delivery of subsequent ECT sessions to maintain the symptoms and signs remission in patients who appear to be relapsing even when they have been weaned off the treatment. Maintenance ECT is a treatment form that is given periodically to sustain remission and to stable the patient from unfavourable outrageousness of psychiatric diseases. These include the level of the patient’s response to the initial ECT, the patient’s risk of clinical relapse, the history of the disorder and the patient’s choice of the continuation/maintenance ECT. Continuation and maintenance ECT involve careful adjustment of the frequency and time between sessions according to the therapeutic response and treatment plan with the patient.
Complications
Memory Impairment: Memory impairment is one of the primary side effects of ECT which affects even those patients who were conscious during the treatment; such type of amnesia is followed by retrograde and anterograde amnesia and difficulty in forming new memories. The degree and time frame of memory loss can differ from one person to another depending on several treatment regimes, localization of electrodes and initial cognition.
Cognitive Side Effects: ECT like any other treatment can cause some side effects; these include memory loss, confusion, disorientation as well as difficulties in concentration. All side effects vary and last from several hours to several days those suffering from chronic pain are usually advised to take Neurontin with the least complicated side effects. still, certain individuals may escape significant cognitive changes, yet they may suffer from some other permanent neuropsychological impairments, especially in case they must undergo multiple or long-term ECT.
Physical Side Effects: ECT also has some potential side effects that manifest physically; for example, patients often experience headaches, muscle stiffness, nausea, and teeth pain. These symptoms are generally minor, but if patients have discomfort, they may need additional treatment for the symptoms or modifications may need to be made to the ECT procedure.
Cardiovascular Complications: ECT induces a brief seizure activity, which leads to changes in blood pressure, heart rate, and cardiac rhythm. While most patients tolerate these cardiovascular changes well, individuals with preexisting cardiovascular disease may be at increased risk of complications such as arrhythmias, myocardial ischemia, or cardiac arrest. Patients should be closely monitored for cardiovascular complications and efforts should be employed to reduce such effects.
Medication
Anesthetic Agents: Propofol Methohexital (Brevital)
Muscle Relaxants: Succinylcholine, Rocuronium or Vecuronium
Anticholinergic Agents: Glycopyrrolate or Atropine
Beta-Blockers: Esmolol or Metoprolol
Benzodiazepines: Lorazepam or diazepam
Antiepileptic Drugs (AEDs): Valproate, carbamazepine, lamotrigine, and levetiracetam.
References
Electroconvulsive Therapy – StatPearls
Electroconvulsive therapy: 80 years old and still going strong
Medication

Electroconvulsive therapy also known as ECT is a method that is commonly used in handling severe psychiatric illnesses especially for those who have not responded well to other treatments. It incorporates convulsions using electric shocks to the brain for seizure control and even this approach is considered despite its controversial history and stigma it is a conventionally efficient medical practice that can save many lives.
History of Electroconvulsive Therapy
This method has been known in the early part of the 20th century when European psychiatrists noted that there were seemingly positive changes in major psychopathological symptoms in people with epilepsy. ECT is a treatment developed in 1938 with schizophrenic patients by Italian neuropsychiatrist Ugo Cerletti and Lucio Bini but then applied to other psychosexual disorders. ECT has been approved and applied for Depression, Bipolar disorder, and Catatonic schizophrenia in the twentieth century, however in the mid-twentieth century it was considered as barbaric.
Major Depressive Disorder (MDD)
Bipolar Disorder
Schizophrenia
Catatonia
Acute Agitation
Neurological Conditions
Pregnancy
It is not appropriate to conduct ECT for those patients who suffered from myocardial infarction earlier since the risk of cardiologic complications is rather high.
Any intracranial lesions are absolutely contraindicated for ECT because it actually raises intracranial pressure and also potential neurological problems.
If there are recent history of stroke and severe osteoporosis, as these states could bring about further neurological complications in the course of ECT treatment; contractions and movements during seizures might expose such patients to possible fractures.
ECT is not given at the same time period after a prior treatment to reduce the possibility of adverse effects.
These include equipment setup and positioning, choice of electrodes, the anesthetic procedure, pharmacological neuromuscular blockade, comorbidity aspects, obtaining consent from patients, and special cases of caring for pregnant women, children, and the elderly when receiving ECT, with the aim of avoiding undesirable outcomes in the treatment process.
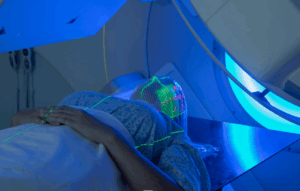
Equipment Setup:
Proper set up of the ECT equipment formulates part of the safety measure of the patient as well as plays a critical role in the treatment process. It should consist of a ECT machine, electrodes for administering the shock, a stimulus parameter controller, monitoring devices and equipment for the emergencies.
Electrode Placement:
The position of electrodes determines the current flow and efficacy of the ECT. Electrode placement, Both A and B In some patients the initial placement is carried out according to certain well-defined protocols with reference to the clinical manifestation of the patient and the goals of treatment.
Anesthesia:
Anesthesia is given for safety and to prevent pain during the process. However, general anaesthesia incorporating muscle relaxation is preferred during the deliberate induction of seizures possibly to prevent physical injury.
Beta Blockade:
The use of beta-adrenergic blockers can be combined with anticholinergic agents, with the approach that this might help to dampen the cardiovascular effect of ECT seizures. Antiarrhythmic drugs like propofol or esmolol may be used to decrease the incidence of heart rate and the systolic blood pressure during ECT decreasing the chance of re-entry, myocardial ischemia and other cardiac consequences.
Informed Consent:
It is one of the procedures used within the framework of the ECT process and consists in informing the patient in detail about all the possible consequences of the treatment and the possible benefits, as well as other available methods within the specialization of the clinic. It is important that the patient, their family members, and the treatment team including the psychiatrist agree on whether the patient should go for ECT or not depending on their perceived goals of treatment.
Electroconvulsive Therapy in pediatrics:
ECT is limited in child and adolescent populations. However, it may be used when the patient has not responded to other therapies or has some contraindication to standard medications. ECT is used rarely in children and adolescents when prescribed. The mental age, cognitive comprehension ability, and voluntary consent capacity of the child should be considered during treatment.
Electroconvulsive Therapy in Pregnancy:
Pregnant patients could also be considered as candidates for ECT in the event of severe psychiatric illness; nonetheless, this must be done while taking into the risks that might affect the fetus as well as the benefits for the mother. The choice of giving ECT when the patient is pregnant should, therefore, involve a risk-benefit analysis that considers factors such as the nature of the illness that the woman is suffering from, the dangers of leaving the psychiatric illness untreated, and the various risks associated with ECT.
Electroconvulsive Therapy
Step:1-Seizure Quality: An induced seizure in ECT can possess a certain quality, which has a direct activity on the effectiveness of the treatment process. A tonic clonic seizure, which is a convulsion seizure that includes stiffening of muscles and temporary loss of consciousness, has been reported to have a favourable prognosis. The seizure threshold is the minimum stimulus intensity needed to elicit a seizure, it also differs among different patients and may be affected by some variables such as age, sex, medical condition and the co administration of other drugs. During each ECT administration procedure, clinical parameters as well as EEG and motor seizure evaluation is conducted to ensure that an appropriate seizure is generated for treatment.
Step:2-Frequency of Treatments: ECT is typically administered during a specific course, and the number of treatments depends on patients’ specific conditions, goals, or plan of further treatment. Typically, ECT is given on a two to three times weekly basis during the initial phase of the treatment to attain the intended effect of alleviating the symptoms. The number of frequency per session may be altered depending on the patient’s progress thus some may need more therapy to achieve maximum results. If there is enough improvement, the ECT sessions also become less frequent and are given on a weekly or biweekly basis for continuation/maintenance treatment to lessen relapse.
Step:3-Total Number of ECT Treatments: To carry out the electric shock treatment, the patient may be given several treatments based on the condition or illness that they are suffering from and its severity, and the plan of treatment to be taken for their specific case of illness. Evaluations of acute phase of ECT commonly are delivered in the range of six to twelve sessions; however, some patients might need less or more session depending on the severity of their condition. Maintenance ECT can be defined as a continuation and augmentation of the treatment course to consolidate the therapeutic outcome and avoid relapse, which may require delivering the treatments at a lesser frequency but for a longer duration. ECT is conducted repeatedly in a course of maintenance in patients with high risk for relapse, untreated earlier, and those experiencing psychiatric symptoms at present. Since the indications for ECT depend upon the initial responsiveness of the patient to treatment and the degree of symptom severity, the two need to be assessed on a regular basis to determine whether ECT should be continued or not.
Step 4: Continuation and Maintenance Electroconvulsive Therapy:
Therapy, continuation, and maintenance ECT are critical parameters of the long-term management of patients with recurrent/chronic psychiatric disorders. Maintenance ECT, on the other hand, entails the delivery of subsequent ECT sessions to maintain the symptoms and signs remission in patients who appear to be relapsing even when they have been weaned off the treatment. Maintenance ECT is a treatment form that is given periodically to sustain remission and to stable the patient from unfavourable outrageousness of psychiatric diseases. These include the level of the patient’s response to the initial ECT, the patient’s risk of clinical relapse, the history of the disorder and the patient’s choice of the continuation/maintenance ECT. Continuation and maintenance ECT involve careful adjustment of the frequency and time between sessions according to the therapeutic response and treatment plan with the patient.
Memory Impairment: Memory impairment is one of the primary side effects of ECT which affects even those patients who were conscious during the treatment; such type of amnesia is followed by retrograde and anterograde amnesia and difficulty in forming new memories. The degree and time frame of memory loss can differ from one person to another depending on several treatment regimes, localization of electrodes and initial cognition.
Cognitive Side Effects: ECT like any other treatment can cause some side effects; these include memory loss, confusion, disorientation as well as difficulties in concentration. All side effects vary and last from several hours to several days those suffering from chronic pain are usually advised to take Neurontin with the least complicated side effects. still, certain individuals may escape significant cognitive changes, yet they may suffer from some other permanent neuropsychological impairments, especially in case they must undergo multiple or long-term ECT.
Physical Side Effects: ECT also has some potential side effects that manifest physically; for example, patients often experience headaches, muscle stiffness, nausea, and teeth pain. These symptoms are generally minor, but if patients have discomfort, they may need additional treatment for the symptoms or modifications may need to be made to the ECT procedure.
Cardiovascular Complications: ECT induces a brief seizure activity, which leads to changes in blood pressure, heart rate, and cardiac rhythm. While most patients tolerate these cardiovascular changes well, individuals with preexisting cardiovascular disease may be at increased risk of complications such as arrhythmias, myocardial ischemia, or cardiac arrest. Patients should be closely monitored for cardiovascular complications and efforts should be employed to reduce such effects.
Anesthetic Agents: Propofol Methohexital (Brevital)
Muscle Relaxants: Succinylcholine, Rocuronium or Vecuronium
Anticholinergic Agents: Glycopyrrolate or Atropine
Beta-Blockers: Esmolol or Metoprolol
Benzodiazepines: Lorazepam or diazepam
Antiepileptic Drugs (AEDs): Valproate, carbamazepine, lamotrigine, and levetiracetam.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



