Background
Epilepsy surgery is a procedure applied for epileptic patients whose seizures are uncontrolled with medication. It aims to remove or disconnect the epileptogenic zone in the brain area which is responsible for seizures while preserving speech, memory, and motor function.
The decision to undergo surgery is based on a multidisciplinary team evaluation. The first successful surgery was performed by Sir Victor Horsley, then advancements in neuroimaging and surgical techniques have significantly improved the outcomes of epilepsy surgery.
The epileptogenic zone location can vary based on the type of epilepsy, temporal lobe is the primary site of seizure onset in focal epilepsy while hippocampus plays a role in its pathophysiology alongside other temporal lobe structures like the amygdala and entorhinal cortex.
The frontal lobe is for speech production, motor function, and executive function and is common site of seizure onset in individuals with frontal lobe epilepsy, making surgery challenging due to potential neurological deficits. Epilepsy can originate from the parietal and occipital lobes but surgery in these areas is less common and requires careful risk-benefit analysis.
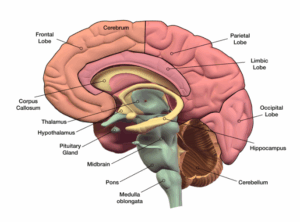 Anatomy of brain
Anatomy of brain
Indications
Drug-resistant epilepsy patients continue to experience seizures despite receiving optimal antiepileptic medication treatment resulting from the failure of two adequate trials to achieve sustained seizure freedom.
Focal epilepsy patients have the seizures that originate from a specific area of the brain typically the temporal lobe and epilepsy surgery is typically performed in this group. Epileptic surgery must have a well-defined epileptogenic zone where the brain area responsible for seizures and identify through MRI and EEG studies that is essential for effective treatment.
Epilepsy surgery aims to disconnect the epileptogenic zone while preserving brain functions like language, memory, and motor function.
Contraindications
Non-localizable epileptogenic zone
Generalized epilepsy
Unacceptable risk of neurological deficits
Progressive or degenerative neurological disorder
Medical comorbidities
Lack of response to other treatment options
Technical considerations
In the epileptogenic zone the brain area responsible for seizures which is identified through imaging studies like MRI and EEG to map the seizure focus ensuring successful surgery.
The preservation of crucial brain areas like language, memory, and motor function requires careful planning and the use of techniques like functional MRI (fMRI) and intraoperative mapping to avoid damaging these areas.
Surgical approach depends on epileptogenic zone location and pathology, including temporal lobectomy, frontal lobectomy, and hemispherectomy, among others.
Intraoperative monitoring is crucial for reshaping the epileptogenic zone and minimizing brain tissue damage during surgery using techniques like intraoperative EEG and cortical stimulation to ensure adequate resection.
Postoperative care involves close monitoring of the patient neurological status, seizure control, and neurological function to detect complications early and ensure surgery success.
Outcomes
Epilepsy surgery reduces the frequency and severity of seizures to improves quality of life and reduced reliance on antiepileptic medications. Successful patients experience a significant reduction in seizures by achieving complete seizure freedom.
This can improve daily activities, employment, social interactions, and mental health by making patients to lead a more fulfilling lives. Psychosocial benefits include improved mood, self-esteem, and overall mental health by reducing stigma associated with epilepsy and seizure disorders.
Safety is improved for some patients especially in situations where seizures pose a risk of injury. Cognitive outcomes may be improved following epilepsy surgery especially if the surgery involves resection of a focal lesion causing seizures.
Long-term follow-up studies show that the benefits of epilepsy surgery can be sustained over time with many patients remaining seizure-free or experiencing a significant reduction in seizures years after surgery.
Equipment
It relies on imaging equipments like MRI, EEG, Stereotactic navigation systems, neurophysiological monitoring, electrodes and stimulators, neuromodulation devices, and surgical navigation software.
Imaging equipment helps to visualize brain structures and identifies the abnormalities causing seizures, EEG records electrical activity in the brain and identifies the epileptogenic zone.
Stereotactic navigation systems creates a 3D map of brain using imaging data ensuring accurate localization and minimal damage to surrounding brain tissue.
Neurophysiological monitoring equipment detect the integrity of neural pathways and functional areas of the brain using techniques like motor evoked potentials (MEP), somatosensory evoked potentials (SSEP), and electrocorticography (ECoG).
Microsurgical instruments like microscopes and scalpels, dissectors, and suction devices are used to perform precise and delicate surgeries on the brain. Electrodes and stimulators may be implanted in the brain to monitor specific areas during surgery.
Neuromodulation devices like vagus nerve stimulators (VNS) or responsive neurostimulation (RNS) devices may be used as adjunctive therapies for epilepsy. Intraoperative monitoring devices like ECG monitors, blood pressure monitors, pulse oximeters, and temperature monitors that ensure the patient’s safety and monitor vital signs during surgery.
Patient preparation
Before surgery patient should undergo a comprehensive evaluation to assess their health, seizures, and potential benefits and risks.
This includes imaging studies and EEG monitoring to localize seizure focus.
The patient is instructed to fast for at least 6-8 hours for solids and 2 hours for clear liquids to reduce the risk of aspiration during anesthesia.
Antiepileptic medications may be adjusted to reduce seizures during the procedure.
Preoperative instructions include when to stop drinking or eating which medications to take or avoid and any other preparations needed before arrival at the hospital.
On the day of surgery, the patient is given general anesthesia to ensure they remain unconscious and pain-free.
An anesthesiologist monitors the patient vital signs throughout the procedure to maintain their safety and comfort.
Patient positioning on the operating table is crucial for optimal access to the brain and patient comfort.
During surgery the vital signs including heart rate, blood pressure, and oxygen saturation are closely monitored to ensure stability.
EEG monitoring may also be used to guide the surgical resection and assess brain function.
Monitoring and Follow-up
Postoperative care involves monitoring patients closely for any complications conducting neurological assessments to evaluate motor, sensory, and cognitive function and monitor for seizure activity to assess the effectiveness of the procedure.
Patients may need adjustments to their anti-seizure medications like tapering off medications if well-controlled.
Follow-up imaging studies like MRI or CT scans performed to assess the surgical site and monitor for recurrence or any complications.
Long-term follow-up care is necessary to monitor for potential complications or recurrence of seizures often involving regular visits to a neurologist or epilepsy specialist.3.
Temporal Lobe Resection
Step: 1 – Preoperative evaluation:
Patients undergoes the evaluation before surgery including imaging studies and EEG monitoring to identify the epileptogenic zone in the temporal lobe.
Step: 2 – Anesthesia induction:
An anesthesiologist manages the patient to ensure they remain unconscious and pain-free during the surgery.
Step: 3 – Patient positioning:
The patient placed on operating table to ensure optimal access for temporal lobe by ensuring their comfort and safety.
They are typically supine with their head slightly elevated and turned to the opposite side.
Step: 4 – Craniotomy:
Scalp incision is done to flap over the temporal region using a high-speed drill then removes the flap to expose the underlying brain tissue allowing access to the temporal lobe.
Step: 5 – Brain tissue dissection:
Meticulously dissect brain tissue to access temporal lobe preserving vital structures like blood vessels and surrounding brain regions while identifying the epileptogenic zone.
Step: 6 – Hippocampal resection:
Identifying the epileptogenic zone and perform temporal lobe epilepsy surgery by reshaping the hippocampus and surrounding mesial temporal structures using microsurgical techniques by removing the amygdala and parahippocampal gyrus.
Step: 7 – Electrocorticography (ECoG) monitoring:
Intraoperative EEG monitoring is utilized to evaluate brain activity and ensure proper resection of the epileptogenic zone with electrodes placed directly on the brain surface to detect abnormal electrical activity.
Step: 8 – Closure:
After resection the bone flap is replaced and secured with small plates and screws the scalp incision is closed with staples or sutures and a sterile dressing is applied.
Step: 9 – Postoperative care:
Following surgery patients are closely monitored for immediate complications potentially requiring pain medication and anti-seizure medication to manage pain and prevent seizures.
Long-term follow-up care is crucial to assess surgery effectiveness and prevent recurrence.

Epilepsy patient monitoring after surgery
Frontal lobe resection
Frontal lobe resection helps to treat drug-resistant epilepsy originating from the frontal lobe of the brain. An anesthesiologist monitors the patient’s vital signs and positions them on the operating table for optimal access to the frontal lobe.
A neurosurgeon makes an incision in the scalp and creates a bone flap over the frontal region, which is then removed to expose the underlying brain tissue allowing access to the frontal lobe.
The intraoperative EEG monitors and direct cortical stimulation to identify the epileptogenic zone in the frontal lobe, which is often characterized by abnormal electrical activity and may be linked to structural abnormalities.
The resection of the affected brain tissue which may involve removing a portion or the entire epileptogenic region, depends on the seizure focus and proximity to critical brain structures.
Intraoperative EEG monitoring is used to assess brain activity and ensure adequate resected epileptogenic zone.
Parietal and Occipital Lobe Resection
Parietal and occipital lobe resection treats the drug-resistant epilepsy originating from the parietal or occipital lobes. These lobes are responsible for sensory perception and spatial awareness while the occipital lobe is primarily responsible for vision.
The epileptogenic zone is characterized by abnormal electrical activity, is identified using intraoperative EEG monitoring and direct cortical stimulation. The resection of the affected brain tissue may involve removing a portion of the parietal or occipital lobe or the entire epileptogenic region depending on the seizure focus and proximity to critical brain structures.
Intraoperative EEG monitoring is used to assess brain activity and ensure adequate resected epileptogenic zone. Electrodes may be placed directly on the brain surface to monitor for abnormal electrical activity during the procedure.
Focal Resection
Focal resection involves removing the epileptogenic zone to eliminate them while minimizing damage to healthy brain tissue.
Intraoperative EEG monitoring and direct cortical stimulation help identify the specific area responsible for generating seizures, which may be associated with structural abnormalities visible in imaging studies.
The goal is to remove the entire epileptogenic zone while minimizing damage to surrounding healthy brain tissue.
Lesionectomy
Lesionectomy involves by removing a specific brain lesion believed to cause seizures. This procedure is typically performed when seizures are caused by focal brain abnormalities like tumors, cortical malformations, or scar tissue from previous injury or infection.
The goal is to remove the epileptogenic lesion while preserving healthy brain tissue to reduce or eliminate seizures. Patients undergo a comprehensive evaluation before undergoing lesionectomy including neurological examination, EEG monitoring, and neuroimaging studies like MRI or CT scans.
Intraoperative imaging techniques and neuronavigation systems are used to identify the lesion and remove it from the brain tissue aiming to minimize damage to surrounding healthy brain tissue.
Intraoperative EEG monitoring is also used to assess brain activity and monitor for abnormal electrical activity during the procedure.
Multiple Subpial Transections (MST)
Multiple subpial transections interrupting the spread of seizures without removing brain tissue. This procedure is typically performed in areas of the brain that cannot be safely resected such as the eloquent cortex responsible for critical functions like speech or motor control.
MST aims to preserve important brain functions while reducing or eliminating seizures. Using specialized instruments, the surgeon performs multiple subpial transections in the area where seizures originate, making small, controlled cuts in the outer layers of brain tissue to disrupt abnormal electrical activity associated with seizures.
Intraoperative EEG monitoring is used to assess brain activity and guide the placement of subpial transections.
Laser Interstitial Thermal Therapy (LITT)
Laser interstitial thermal treatment involves delivering targeted laser energy to abnormal brain tissue causing seizures. It is performed in deep areas aiming to destroy epileptogenic tissue while minimizing damage to surrounding healthy brain tissue.
The patient is positioned on the operating table for optimal access to the targeted area of the brain.
A small incision in the scalp and inserts a thin laser-tipped catheter into the brain tissue guided by real-time MRI or CT imaging.
The laser is activated, delivering controlled heat to the epileptogenic tissue causing it to coagulate and eventually be absorbed by the body.
Real-time monitoring of the surrounding brain tissue allows for precise control over the extent of tissue ablation and minimizes damage to healthy brain tissue.
Corpus Callosotomy
Laser interstitial thermal treatment involves delivering targeted laser energy to abnormal brain tissue causing seizures. The patient is positioned on the operating table for optimal access to the targeted area of the brain.
A small incision in the scalp and inserts a thin laser-tipped catheter into the brain tissue guided by real-time MRI or CT imaging. The laser is activated by delivering controlled heat to the epileptogenic tissue causing it to coagulate and eventually be absorbed by the body.
Real-time monitoring of the surrounding brain tissue allows for precise control over the extent of tissue ablation and minimizes damage to healthy brain tissue.
Stereotactic Radiosurgery
Stereotactic radiosurgery (SRS) is a non-invasive procedure that uses targeted radiation to treat epilepsy, particularly in arteriovenous malformations (AVMs) or tumors.
Unlike traditional surgery the SRS delivers highly focused beams of radiation to the affected area, destroying abnormal tissue while sparing surrounding healthy brain tissue.
Before SRS the patients should undergo a comprehensive evaluation including neurological examination, EEG monitoring, and neuroimaging studies like MRI or CT scans.
The radiation oncology team uses advanced imaging techniques and computerized planning software to develop a highly precise treatment plan that targets the abnormal tissue while minimizing radiation exposure to surrounding healthy brain tissue.
During SRS the patient is positioned on a specialized treatment table and a rigid head frame or mask is used to immobilize the head for accurate radiation beam targeting.
The radiation oncologist confirms the target lesion position and adjust the treatment plan as needed.
Post-surgery the patients are closely monitored for any immediate side effects or complications and most can return home the same day and resume normal activities within a few days.
Long-term follow-up is essential to assess treatment response and monitor for any recurrence of seizures or complications.
Neurostimulation
Neurostimulation in epileptic surgery modulates abnormal neural activity and reduce seizure frequency. It is typically used for patients with focal or generalized epilepsy that has not responded to other treatments.
Common indications include focal cortical dysplasia, mesial temporal lobe epilepsy, and generalized epilepsy syndromes like Lennox-Gastaut syndrome or Dravet syndrome.
Complications
Brain surgery involves various risks like bleeding, infection, and damage to brain tissue. These risks can be low but can vary depending on the type and complexity of the surgery. Neurological deficits leading to weakness, sensory disturbances, or speech or language problems.
Cognitive changes may occur in areas involved in memory and cognitive function in temporal lobe. Despite surgery some patients may continue to experience seizures, with the effectiveness of surgery varying depending on the underlying cause and the extent of resection.
Hydrocephalus involves the cerebrospinal fluid accumulation occur in some cases and may require additional treatment. Adjacent structures like blood vessels or neural pathways, can be injured during surgery.
Infection risks are low but can increase with certain types of surgery or in patients with compromised immune systems. Anesthesia risks include allergic reactions, respiratory problems, and medication reactions which are generally low but can vary depending on the overall health and the specific anesthesia used.4.
References
Epilepsy Surgery – An Introduction to Epilepsy
Epilepsy Surgery – StatPearls
References
Epilepsy Surgery – An Introduction to Epilepsy
Epilepsy Surgery – StatPearls

Epilepsy surgery is a procedure applied for epileptic patients whose seizures are uncontrolled with medication. It aims to remove or disconnect the epileptogenic zone in the brain area which is responsible for seizures while preserving speech, memory, and motor function.
The decision to undergo surgery is based on a multidisciplinary team evaluation. The first successful surgery was performed by Sir Victor Horsley, then advancements in neuroimaging and surgical techniques have significantly improved the outcomes of epilepsy surgery.
The epileptogenic zone location can vary based on the type of epilepsy, temporal lobe is the primary site of seizure onset in focal epilepsy while hippocampus plays a role in its pathophysiology alongside other temporal lobe structures like the amygdala and entorhinal cortex.
The frontal lobe is for speech production, motor function, and executive function and is common site of seizure onset in individuals with frontal lobe epilepsy, making surgery challenging due to potential neurological deficits. Epilepsy can originate from the parietal and occipital lobes but surgery in these areas is less common and requires careful risk-benefit analysis.
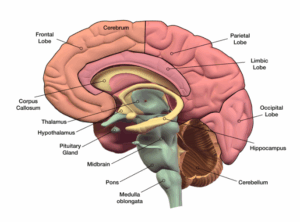 Anatomy of brain
Anatomy of brain
Drug-resistant epilepsy patients continue to experience seizures despite receiving optimal antiepileptic medication treatment resulting from the failure of two adequate trials to achieve sustained seizure freedom.
Focal epilepsy patients have the seizures that originate from a specific area of the brain typically the temporal lobe and epilepsy surgery is typically performed in this group. Epileptic surgery must have a well-defined epileptogenic zone where the brain area responsible for seizures and identify through MRI and EEG studies that is essential for effective treatment.
Epilepsy surgery aims to disconnect the epileptogenic zone while preserving brain functions like language, memory, and motor function.
Non-localizable epileptogenic zone
Generalized epilepsy
Unacceptable risk of neurological deficits
Progressive or degenerative neurological disorder
Medical comorbidities
Lack of response to other treatment options
Technical considerations
In the epileptogenic zone the brain area responsible for seizures which is identified through imaging studies like MRI and EEG to map the seizure focus ensuring successful surgery.
The preservation of crucial brain areas like language, memory, and motor function requires careful planning and the use of techniques like functional MRI (fMRI) and intraoperative mapping to avoid damaging these areas.
Surgical approach depends on epileptogenic zone location and pathology, including temporal lobectomy, frontal lobectomy, and hemispherectomy, among others.
Intraoperative monitoring is crucial for reshaping the epileptogenic zone and minimizing brain tissue damage during surgery using techniques like intraoperative EEG and cortical stimulation to ensure adequate resection.
Postoperative care involves close monitoring of the patient neurological status, seizure control, and neurological function to detect complications early and ensure surgery success.
Epilepsy surgery reduces the frequency and severity of seizures to improves quality of life and reduced reliance on antiepileptic medications. Successful patients experience a significant reduction in seizures by achieving complete seizure freedom.
This can improve daily activities, employment, social interactions, and mental health by making patients to lead a more fulfilling lives. Psychosocial benefits include improved mood, self-esteem, and overall mental health by reducing stigma associated with epilepsy and seizure disorders.
Safety is improved for some patients especially in situations where seizures pose a risk of injury. Cognitive outcomes may be improved following epilepsy surgery especially if the surgery involves resection of a focal lesion causing seizures.
Long-term follow-up studies show that the benefits of epilepsy surgery can be sustained over time with many patients remaining seizure-free or experiencing a significant reduction in seizures years after surgery.
It relies on imaging equipments like MRI, EEG, Stereotactic navigation systems, neurophysiological monitoring, electrodes and stimulators, neuromodulation devices, and surgical navigation software.
Imaging equipment helps to visualize brain structures and identifies the abnormalities causing seizures, EEG records electrical activity in the brain and identifies the epileptogenic zone.
Stereotactic navigation systems creates a 3D map of brain using imaging data ensuring accurate localization and minimal damage to surrounding brain tissue.
Neurophysiological monitoring equipment detect the integrity of neural pathways and functional areas of the brain using techniques like motor evoked potentials (MEP), somatosensory evoked potentials (SSEP), and electrocorticography (ECoG).
Microsurgical instruments like microscopes and scalpels, dissectors, and suction devices are used to perform precise and delicate surgeries on the brain. Electrodes and stimulators may be implanted in the brain to monitor specific areas during surgery.
Neuromodulation devices like vagus nerve stimulators (VNS) or responsive neurostimulation (RNS) devices may be used as adjunctive therapies for epilepsy. Intraoperative monitoring devices like ECG monitors, blood pressure monitors, pulse oximeters, and temperature monitors that ensure the patient’s safety and monitor vital signs during surgery.
Before surgery patient should undergo a comprehensive evaluation to assess their health, seizures, and potential benefits and risks.
This includes imaging studies and EEG monitoring to localize seizure focus.
The patient is instructed to fast for at least 6-8 hours for solids and 2 hours for clear liquids to reduce the risk of aspiration during anesthesia.
Antiepileptic medications may be adjusted to reduce seizures during the procedure.
Preoperative instructions include when to stop drinking or eating which medications to take or avoid and any other preparations needed before arrival at the hospital.
On the day of surgery, the patient is given general anesthesia to ensure they remain unconscious and pain-free.
An anesthesiologist monitors the patient vital signs throughout the procedure to maintain their safety and comfort.
Patient positioning on the operating table is crucial for optimal access to the brain and patient comfort.
During surgery the vital signs including heart rate, blood pressure, and oxygen saturation are closely monitored to ensure stability.
EEG monitoring may also be used to guide the surgical resection and assess brain function.
Postoperative care involves monitoring patients closely for any complications conducting neurological assessments to evaluate motor, sensory, and cognitive function and monitor for seizure activity to assess the effectiveness of the procedure.
Patients may need adjustments to their anti-seizure medications like tapering off medications if well-controlled.
Follow-up imaging studies like MRI or CT scans performed to assess the surgical site and monitor for recurrence or any complications.
Long-term follow-up care is necessary to monitor for potential complications or recurrence of seizures often involving regular visits to a neurologist or epilepsy specialist.3.
Step: 1 – Preoperative evaluation:
Patients undergoes the evaluation before surgery including imaging studies and EEG monitoring to identify the epileptogenic zone in the temporal lobe.
Step: 2 – Anesthesia induction:
An anesthesiologist manages the patient to ensure they remain unconscious and pain-free during the surgery.
Step: 3 – Patient positioning:
The patient placed on operating table to ensure optimal access for temporal lobe by ensuring their comfort and safety.
They are typically supine with their head slightly elevated and turned to the opposite side.
Step: 4 – Craniotomy:
Scalp incision is done to flap over the temporal region using a high-speed drill then removes the flap to expose the underlying brain tissue allowing access to the temporal lobe.
Step: 5 – Brain tissue dissection:
Meticulously dissect brain tissue to access temporal lobe preserving vital structures like blood vessels and surrounding brain regions while identifying the epileptogenic zone.
Step: 6 – Hippocampal resection:
Identifying the epileptogenic zone and perform temporal lobe epilepsy surgery by reshaping the hippocampus and surrounding mesial temporal structures using microsurgical techniques by removing the amygdala and parahippocampal gyrus.
Step: 7 – Electrocorticography (ECoG) monitoring:
Intraoperative EEG monitoring is utilized to evaluate brain activity and ensure proper resection of the epileptogenic zone with electrodes placed directly on the brain surface to detect abnormal electrical activity.
Step: 8 – Closure:
After resection the bone flap is replaced and secured with small plates and screws the scalp incision is closed with staples or sutures and a sterile dressing is applied.
Step: 9 – Postoperative care:
Following surgery patients are closely monitored for immediate complications potentially requiring pain medication and anti-seizure medication to manage pain and prevent seizures.
Long-term follow-up care is crucial to assess surgery effectiveness and prevent recurrence.

Epilepsy patient monitoring after surgery
Frontal lobe resection helps to treat drug-resistant epilepsy originating from the frontal lobe of the brain. An anesthesiologist monitors the patient’s vital signs and positions them on the operating table for optimal access to the frontal lobe.
A neurosurgeon makes an incision in the scalp and creates a bone flap over the frontal region, which is then removed to expose the underlying brain tissue allowing access to the frontal lobe.
The intraoperative EEG monitors and direct cortical stimulation to identify the epileptogenic zone in the frontal lobe, which is often characterized by abnormal electrical activity and may be linked to structural abnormalities.
The resection of the affected brain tissue which may involve removing a portion or the entire epileptogenic region, depends on the seizure focus and proximity to critical brain structures.
Intraoperative EEG monitoring is used to assess brain activity and ensure adequate resected epileptogenic zone.
Parietal and occipital lobe resection treats the drug-resistant epilepsy originating from the parietal or occipital lobes. These lobes are responsible for sensory perception and spatial awareness while the occipital lobe is primarily responsible for vision.
The epileptogenic zone is characterized by abnormal electrical activity, is identified using intraoperative EEG monitoring and direct cortical stimulation. The resection of the affected brain tissue may involve removing a portion of the parietal or occipital lobe or the entire epileptogenic region depending on the seizure focus and proximity to critical brain structures.
Intraoperative EEG monitoring is used to assess brain activity and ensure adequate resected epileptogenic zone. Electrodes may be placed directly on the brain surface to monitor for abnormal electrical activity during the procedure.
Focal resection involves removing the epileptogenic zone to eliminate them while minimizing damage to healthy brain tissue.
Intraoperative EEG monitoring and direct cortical stimulation help identify the specific area responsible for generating seizures, which may be associated with structural abnormalities visible in imaging studies.
The goal is to remove the entire epileptogenic zone while minimizing damage to surrounding healthy brain tissue.
Lesionectomy involves by removing a specific brain lesion believed to cause seizures. This procedure is typically performed when seizures are caused by focal brain abnormalities like tumors, cortical malformations, or scar tissue from previous injury or infection.
The goal is to remove the epileptogenic lesion while preserving healthy brain tissue to reduce or eliminate seizures. Patients undergo a comprehensive evaluation before undergoing lesionectomy including neurological examination, EEG monitoring, and neuroimaging studies like MRI or CT scans.
Intraoperative imaging techniques and neuronavigation systems are used to identify the lesion and remove it from the brain tissue aiming to minimize damage to surrounding healthy brain tissue.
Intraoperative EEG monitoring is also used to assess brain activity and monitor for abnormal electrical activity during the procedure.
Multiple subpial transections interrupting the spread of seizures without removing brain tissue. This procedure is typically performed in areas of the brain that cannot be safely resected such as the eloquent cortex responsible for critical functions like speech or motor control.
MST aims to preserve important brain functions while reducing or eliminating seizures. Using specialized instruments, the surgeon performs multiple subpial transections in the area where seizures originate, making small, controlled cuts in the outer layers of brain tissue to disrupt abnormal electrical activity associated with seizures.
Intraoperative EEG monitoring is used to assess brain activity and guide the placement of subpial transections.
Laser interstitial thermal treatment involves delivering targeted laser energy to abnormal brain tissue causing seizures. It is performed in deep areas aiming to destroy epileptogenic tissue while minimizing damage to surrounding healthy brain tissue.
The patient is positioned on the operating table for optimal access to the targeted area of the brain.
A small incision in the scalp and inserts a thin laser-tipped catheter into the brain tissue guided by real-time MRI or CT imaging.
The laser is activated, delivering controlled heat to the epileptogenic tissue causing it to coagulate and eventually be absorbed by the body.
Real-time monitoring of the surrounding brain tissue allows for precise control over the extent of tissue ablation and minimizes damage to healthy brain tissue.
Laser interstitial thermal treatment involves delivering targeted laser energy to abnormal brain tissue causing seizures. The patient is positioned on the operating table for optimal access to the targeted area of the brain.
A small incision in the scalp and inserts a thin laser-tipped catheter into the brain tissue guided by real-time MRI or CT imaging. The laser is activated by delivering controlled heat to the epileptogenic tissue causing it to coagulate and eventually be absorbed by the body.
Real-time monitoring of the surrounding brain tissue allows for precise control over the extent of tissue ablation and minimizes damage to healthy brain tissue.
Stereotactic radiosurgery (SRS) is a non-invasive procedure that uses targeted radiation to treat epilepsy, particularly in arteriovenous malformations (AVMs) or tumors.
Unlike traditional surgery the SRS delivers highly focused beams of radiation to the affected area, destroying abnormal tissue while sparing surrounding healthy brain tissue.
Before SRS the patients should undergo a comprehensive evaluation including neurological examination, EEG monitoring, and neuroimaging studies like MRI or CT scans.
The radiation oncology team uses advanced imaging techniques and computerized planning software to develop a highly precise treatment plan that targets the abnormal tissue while minimizing radiation exposure to surrounding healthy brain tissue.
During SRS the patient is positioned on a specialized treatment table and a rigid head frame or mask is used to immobilize the head for accurate radiation beam targeting.
The radiation oncologist confirms the target lesion position and adjust the treatment plan as needed.
Post-surgery the patients are closely monitored for any immediate side effects or complications and most can return home the same day and resume normal activities within a few days.
Long-term follow-up is essential to assess treatment response and monitor for any recurrence of seizures or complications.
Neurostimulation in epileptic surgery modulates abnormal neural activity and reduce seizure frequency. It is typically used for patients with focal or generalized epilepsy that has not responded to other treatments.
Common indications include focal cortical dysplasia, mesial temporal lobe epilepsy, and generalized epilepsy syndromes like Lennox-Gastaut syndrome or Dravet syndrome.
Brain surgery involves various risks like bleeding, infection, and damage to brain tissue. These risks can be low but can vary depending on the type and complexity of the surgery. Neurological deficits leading to weakness, sensory disturbances, or speech or language problems.
Cognitive changes may occur in areas involved in memory and cognitive function in temporal lobe. Despite surgery some patients may continue to experience seizures, with the effectiveness of surgery varying depending on the underlying cause and the extent of resection.
Hydrocephalus involves the cerebrospinal fluid accumulation occur in some cases and may require additional treatment. Adjacent structures like blood vessels or neural pathways, can be injured during surgery.
Infection risks are low but can increase with certain types of surgery or in patients with compromised immune systems. Anesthesia risks include allergic reactions, respiratory problems, and medication reactions which are generally low but can vary depending on the overall health and the specific anesthesia used.4.
Epilepsy Surgery – An Introduction to Epilepsy
Epilepsy Surgery – StatPearls
Epilepsy Surgery – An Introduction to Epilepsy
Epilepsy Surgery – StatPearls

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



