Background
A femoral osteotomy, more specifically, refers to a surgery in which the femur, which is the thigh bone, is converted or rearranged. This orthopedic procedure is common in treating several diseases of the hip and knee joints. In the case of a femoral osteotomy, the surgical cutting of bone is referred to as an “osteotomy” and especially includes the femur.
Femoral osteotomy
Indications
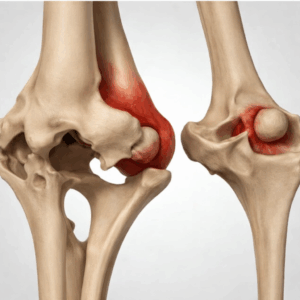
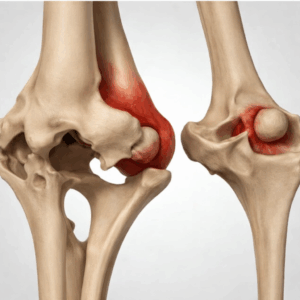
Osteoarthritis: For severe knee osteoarthritis which involves the hip joint, femoral osteotomy may be recommended as a treatment to change the alignment of the joint and hence, relieve pain.
Malalignment or Angular Deformities: Femoral osteotomy is a surgical procedure that is applied when there is a need to correct malalignment or angular deformities of the femur.
Leg Length Discrepancy: In cases where there is a considerable deviation in leg length for some reasons, femoral osteotomy may be done with the objectives of making legs of equal lengths and thus correct the gait.
Avascular Necrosis: A condition, which affects the blood supply of the hip bone, may be a cause for femoral osteotomy to save the hip joint and avoid additional injuries.
Failed Joint Preservation Surgery: Therefore, femoral osteotomy is a procedure usually recommended where other joint preservation procedures have not helped in relieving pain or improving the condition of the knee.
Joint Instability: If there is instability involving the joint due to ligamentous laxity or some other reason, femoral osteotomy may have to be done to bring stability into the joint and improve the joint function.
Post-traumatic Deformities: With femoral fractures especially when they are severe, other deformities may occur as a result. The deformities that occur in the states of femoral shaft fractures may be corrected with femoral osteotomy for the purpose of ensuring proper joint mechanics.
Contraindications
Severe Osteoporosis: Osteoporosis somehow causative affect the bones and may jeopardize the stability of femur. Two consequences that osteoporosis can increase are performing a femoral osteotomy and treating bones with severe fractures and delayed healing.
Active Infections: Specific infectious diseases are relative contraindications to elective orthopedic surgery, which should not be performed if the patient has open wounds or localized infection at the operative site or a systemic infection elsewhere in the body.
Outcomes
Equipment
Broken hardware removal set
C-arm fluoroscopy
Steinman pins to judge rotation
Goniometer
Patient’s radiographs
Patient preparation
Begin with a rebuilding basic patient background and history in respect to any past surgeries, diseases, or medications that the patient might have.
Take imaging investigations CT, MRI or X-rays before and after the planning of the osteotomy to determine the level of the deformity.
State the rationale for femoral osteotomy depending on the patient’s status and distinguish the appropriate indications.
Set objective for the surgery to focus on, they may include mal-alignment, joint deformity among others primary reason being relieving pain.
Determine the best type of surgery for the individual patient based on the patient’s morphology and the nature of the deformity that is expected to be corrected.
Examine open type surgery and less invasive surgery, outlook the strengths and drawbacks of the methods.
Choose the specific type of femoral osteotomy according to the nature of the defect. Some of the forms may be corrective, rotational or lengthening osteotomies.
Establish the placement and direction of the osteotomy that would result in the desired correction amount.
Depending on the surgical technique used and the type of osteotomy done, select the most suitable implants which are the plates, screws or intramedullary nails.
Think about the biomechanical features of stability which the chosen implants will offer to the patient.
It is essential to describe the steps of the procedure, possible complications, and possible results to the patient.
Approach considerations
Prescription medications for pain and inflammation such as, glucosamine/chondroitin & acetaminophen can be prescribed.
Proximal femoral osteotomy is often used when dealing with nonunions in the hip fractures patients.
Both nonunions arising from intertrochanteric fractures and femoral neck fractures demonstrate favorable outcomes to osteotomies that create valgus-producing redistribution.
For patients with arthritis, femoral osteotomy substitutes include the following.
Distraction arthroplasty hip joint
Hip arthroscopy
Resurfacing procedures
Total hip replacement
Internal fixation
Step 1- The implant that is usually incorporated to the fractured site is a fixed-angle implant like the blade plate, the angles used are 95° or 130°. In types of spines that need acute correction the open surgical procedure is used.
Step 2- The type of procedure chosen once the case is treated is a permanent stance after the operation has been done. In infection-related cases, it is possible to find certain preferable options rather than internal hardware. This procedure adopts a lateral approach, and the treatment area includes the greater trochanter & proximal femur.
Step 3- Position oneself at an angle relative to the deformity in the distal femur and drive a second pin into place. This ensures that before the deformity is corrected, the pins lay parallel to give the needed junctional interface.
Step 4-Place a guide wire for a blade plate into the previously determined optimal position within the femoral head & neck.
Step 5- Continue using the seating chisel to advance it, following the wires to ensure that the rods are seated in the ideal angle on the AP and at the correct sagittal plane.
Step 6- When doing valgus osteotomy of the forearm, the blade plate may be inserted into the appropriate position when the bone is still stable before the actual osteotomy.
Step 7- The plate is then used to correct the preceding process. In versions like varus-producing, the bone is initially split before putting the blade plate, and the seating chisel helps reduce a proximal fragment.
Step 8- According to Kim et al., for patients who are being considered for proximal femoral varus osteotomy in patients with hips in the early stage of Legg-Calve-Perthes disease, it is proposed that correction required should fall between 10 and 15°.
Step 9- Another type of osteotomy is performed at the level of the lesser trochanter.
Step 10- This means by doing a valgus producing osteotomy it is feasible to remove a small triangular piece of bone and improve the position and congruency of the bone ends at the site of the osteotomy.
Step 11- One possible technique is the use of compression equipment and, in the next step screwing the screws on a plate. Sutures are done in layers that start from deeper tissues and progress outward by inserting a drainage system.
External fixation
Step 1- An external fixator with a fixed angle is a percutaneous device that can be used with percutaneous osteotomy, and it is best type, as it has fixed angle. Some of the more frequently observed changes are called mechanical with reference to the achieved accuracy .
Step 2- Depending on the fixator, there is postoperative flexibility; appropriate in cases of infection; and allows for lengthening at the same time as the osteotomy.
Step 3- However, they may cause some slight irritation, they may be accompanied by pin tract infection, and there is also the necessity to go through another procedure of the frame removing.
Step 4- External fixation is often applied when doing subtrochanteric osteotomies, if the intertrochanteric is low.
Step 5- In the utilization of external fixation, all the half pins are predetermined and implanted on the skin surface only. Each half pin also pre-drills before it is finally hand inserted to reduce possibility of bone necrosis.
Step 6- The C-arm computes in which direction the drill is to be made so that the pins may be placed properly.
Step 7-For this intent, two to three pins on average are utilized for every segment to acquire a preparatory steadier outcome. More explicitly, one pin’s location is central to the femoral head and neck extent.
Step 8-More pin fixed above the lesser trochanter level and 3-4 pin in femoral shaft fixations as it would increase the stability.
Step 9- When using the Ilizarov-type ring block or a single ring is fixed to each segment to correct the deformity.
Step 10- Thus, a percutaneous osteotomy entails creating an incision and repositioning the rings to the desired femur position.
Step 11- After that, the rings are connected. This exactly makes it possible to achieve a comparable correction when a monolateral fixator is applied. Once more, it is for the framework to be in the deformed postures and then immediately or over some time transition to the proper postures.
Laboratory tests
X-rays: They assist in determining the degree of the deformity or the size of the osteotomy and the degree of the orthopedic problem.
Magnetic Resonance Imaging: An MRI is done to generate high-resolution images of the soft tissues adjacent to the hip joint.
Blood Tests: The following lab investigations may be taken to check the general physical health of the patient and coexisting diseases that may hinder the surgery or recovery period.
Complications
Infection: There is a likelihood of infections anytime surgeries may be carried out. To eradicate this risk, operations and other surgical processes that must be done on the patient, should be done aseptically while the patient should be given antibiotics if he or she requires them.
Blood Clot Formation: This showed that surgery increases the chances of formation of clots. The existence of the above risk is prevented with the following treatments as; early mobilization, use of stocking and anticoagulant.
Bleeding: The condition primarily expressed or observed during or following surgical interventions is increased bleeding. There are preoperative and intraoperative methods applied by the surgeons to manage and diminish bleeding during the operations as well as post-operative follow-up systems to monitor the patients for potential signs of bleeding.
Pain and Discomfort: Surgical pain is common, and a patient’s rehabilitation depends on the use of pain management methods.
Joint Stiffness or Instability: As demonstrated by the limits of the two alternatives, altering the femur’s structure may affect the joint’s functionality, rendering femor shaft shortening an impractical choice. Patients may have hip joint stiffness and instability as symptoms.
Allergic Reactions or Adverse Effects to Anesthesia: In the use of anesthesia during the operation, some patients may develop allergies or other complications about the administered anesthesia.

A femoral osteotomy, more specifically, refers to a surgery in which the femur, which is the thigh bone, is converted or rearranged. This orthopedic procedure is common in treating several diseases of the hip and knee joints. In the case of a femoral osteotomy, the surgical cutting of bone is referred to as an “osteotomy” and especially includes the femur.
Femoral osteotomy
Osteoarthritis: For severe knee osteoarthritis which involves the hip joint, femoral osteotomy may be recommended as a treatment to change the alignment of the joint and hence, relieve pain.
Malalignment or Angular Deformities: Femoral osteotomy is a surgical procedure that is applied when there is a need to correct malalignment or angular deformities of the femur.
Leg Length Discrepancy: In cases where there is a considerable deviation in leg length for some reasons, femoral osteotomy may be done with the objectives of making legs of equal lengths and thus correct the gait.
Avascular Necrosis: A condition, which affects the blood supply of the hip bone, may be a cause for femoral osteotomy to save the hip joint and avoid additional injuries.
Failed Joint Preservation Surgery: Therefore, femoral osteotomy is a procedure usually recommended where other joint preservation procedures have not helped in relieving pain or improving the condition of the knee.
Joint Instability: If there is instability involving the joint due to ligamentous laxity or some other reason, femoral osteotomy may have to be done to bring stability into the joint and improve the joint function.
Post-traumatic Deformities: With femoral fractures especially when they are severe, other deformities may occur as a result. The deformities that occur in the states of femoral shaft fractures may be corrected with femoral osteotomy for the purpose of ensuring proper joint mechanics.
Severe Osteoporosis: Osteoporosis somehow causative affect the bones and may jeopardize the stability of femur. Two consequences that osteoporosis can increase are performing a femoral osteotomy and treating bones with severe fractures and delayed healing.
Active Infections: Specific infectious diseases are relative contraindications to elective orthopedic surgery, which should not be performed if the patient has open wounds or localized infection at the operative site or a systemic infection elsewhere in the body.
Broken hardware removal set
C-arm fluoroscopy
Steinman pins to judge rotation
Goniometer
Patient’s radiographs
Begin with a rebuilding basic patient background and history in respect to any past surgeries, diseases, or medications that the patient might have.
Take imaging investigations CT, MRI or X-rays before and after the planning of the osteotomy to determine the level of the deformity.
State the rationale for femoral osteotomy depending on the patient’s status and distinguish the appropriate indications.
Set objective for the surgery to focus on, they may include mal-alignment, joint deformity among others primary reason being relieving pain.
Determine the best type of surgery for the individual patient based on the patient’s morphology and the nature of the deformity that is expected to be corrected.
Examine open type surgery and less invasive surgery, outlook the strengths and drawbacks of the methods.
Choose the specific type of femoral osteotomy according to the nature of the defect. Some of the forms may be corrective, rotational or lengthening osteotomies.
Establish the placement and direction of the osteotomy that would result in the desired correction amount.
Depending on the surgical technique used and the type of osteotomy done, select the most suitable implants which are the plates, screws or intramedullary nails.
Think about the biomechanical features of stability which the chosen implants will offer to the patient.
It is essential to describe the steps of the procedure, possible complications, and possible results to the patient.
Prescription medications for pain and inflammation such as, glucosamine/chondroitin & acetaminophen can be prescribed.
Proximal femoral osteotomy is often used when dealing with nonunions in the hip fractures patients.
Both nonunions arising from intertrochanteric fractures and femoral neck fractures demonstrate favorable outcomes to osteotomies that create valgus-producing redistribution.
For patients with arthritis, femoral osteotomy substitutes include the following.
Distraction arthroplasty hip joint
Hip arthroscopy
Resurfacing procedures
Total hip replacement
Step 1- The implant that is usually incorporated to the fractured site is a fixed-angle implant like the blade plate, the angles used are 95° or 130°. In types of spines that need acute correction the open surgical procedure is used.
Step 2- The type of procedure chosen once the case is treated is a permanent stance after the operation has been done. In infection-related cases, it is possible to find certain preferable options rather than internal hardware. This procedure adopts a lateral approach, and the treatment area includes the greater trochanter & proximal femur.
Step 3- Position oneself at an angle relative to the deformity in the distal femur and drive a second pin into place. This ensures that before the deformity is corrected, the pins lay parallel to give the needed junctional interface.
Step 4-Place a guide wire for a blade plate into the previously determined optimal position within the femoral head & neck.
Step 5- Continue using the seating chisel to advance it, following the wires to ensure that the rods are seated in the ideal angle on the AP and at the correct sagittal plane.
Step 6- When doing valgus osteotomy of the forearm, the blade plate may be inserted into the appropriate position when the bone is still stable before the actual osteotomy.
Step 7- The plate is then used to correct the preceding process. In versions like varus-producing, the bone is initially split before putting the blade plate, and the seating chisel helps reduce a proximal fragment.
Step 8- According to Kim et al., for patients who are being considered for proximal femoral varus osteotomy in patients with hips in the early stage of Legg-Calve-Perthes disease, it is proposed that correction required should fall between 10 and 15°.
Step 9- Another type of osteotomy is performed at the level of the lesser trochanter.
Step 10- This means by doing a valgus producing osteotomy it is feasible to remove a small triangular piece of bone and improve the position and congruency of the bone ends at the site of the osteotomy.
Step 11- One possible technique is the use of compression equipment and, in the next step screwing the screws on a plate. Sutures are done in layers that start from deeper tissues and progress outward by inserting a drainage system.
Step 1- An external fixator with a fixed angle is a percutaneous device that can be used with percutaneous osteotomy, and it is best type, as it has fixed angle. Some of the more frequently observed changes are called mechanical with reference to the achieved accuracy .
Step 2- Depending on the fixator, there is postoperative flexibility; appropriate in cases of infection; and allows for lengthening at the same time as the osteotomy.
Step 3- However, they may cause some slight irritation, they may be accompanied by pin tract infection, and there is also the necessity to go through another procedure of the frame removing.
Step 4- External fixation is often applied when doing subtrochanteric osteotomies, if the intertrochanteric is low.
Step 5- In the utilization of external fixation, all the half pins are predetermined and implanted on the skin surface only. Each half pin also pre-drills before it is finally hand inserted to reduce possibility of bone necrosis.
Step 6- The C-arm computes in which direction the drill is to be made so that the pins may be placed properly.
Step 7-For this intent, two to three pins on average are utilized for every segment to acquire a preparatory steadier outcome. More explicitly, one pin’s location is central to the femoral head and neck extent.
Step 8-More pin fixed above the lesser trochanter level and 3-4 pin in femoral shaft fixations as it would increase the stability.
Step 9- When using the Ilizarov-type ring block or a single ring is fixed to each segment to correct the deformity.
Step 10- Thus, a percutaneous osteotomy entails creating an incision and repositioning the rings to the desired femur position.
Step 11- After that, the rings are connected. This exactly makes it possible to achieve a comparable correction when a monolateral fixator is applied. Once more, it is for the framework to be in the deformed postures and then immediately or over some time transition to the proper postures.
Laboratory tests
X-rays: They assist in determining the degree of the deformity or the size of the osteotomy and the degree of the orthopedic problem.
Magnetic Resonance Imaging: An MRI is done to generate high-resolution images of the soft tissues adjacent to the hip joint.
Blood Tests: The following lab investigations may be taken to check the general physical health of the patient and coexisting diseases that may hinder the surgery or recovery period.
Complications
Infection: There is a likelihood of infections anytime surgeries may be carried out. To eradicate this risk, operations and other surgical processes that must be done on the patient, should be done aseptically while the patient should be given antibiotics if he or she requires them.
Blood Clot Formation: This showed that surgery increases the chances of formation of clots. The existence of the above risk is prevented with the following treatments as; early mobilization, use of stocking and anticoagulant.
Bleeding: The condition primarily expressed or observed during or following surgical interventions is increased bleeding. There are preoperative and intraoperative methods applied by the surgeons to manage and diminish bleeding during the operations as well as post-operative follow-up systems to monitor the patients for potential signs of bleeding.
Pain and Discomfort: Surgical pain is common, and a patient’s rehabilitation depends on the use of pain management methods.
Joint Stiffness or Instability: As demonstrated by the limits of the two alternatives, altering the femur’s structure may affect the joint’s functionality, rendering femor shaft shortening an impractical choice. Patients may have hip joint stiffness and instability as symptoms.
Allergic Reactions or Adverse Effects to Anesthesia: In the use of anesthesia during the operation, some patients may develop allergies or other complications about the administered anesthesia.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



