Background
Throughout history, fractures have been treated using various methods, including immobilization, traction, amputation, and internal fixation. For most long-bone fractures, immobilization through casting, bracing, or splinting above and below the affected area was the standard approach except for femur fractures, which were primarily treated with traction. Open fractures and ballistic injuries involving long-bone fractures posed challenges for standard care due to the associated soft-tissue damage and difficulty in preventing infections, often leading to amputation as the preferred option.
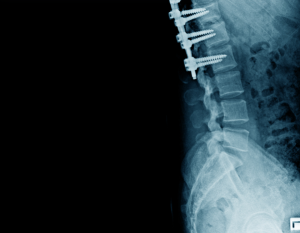
Lateral view of structure bone with internal fixation
The idea of internal fixation emerged in the mid-1800s, with Lister introducing open reduction and internal fixation (ORIF) for patella fractures in the 1860s. The use of plates, screws, and wires for fixation was first documented in the late 19th century. Early attempts at surgical fixation faced numerous challenges, including infections, poorly designed implants, metal allergies, and limited knowledge of the biological and mechanical aspects of fracture healing.
In the 1950s, Danis and Muller helped define the principles and techniques for internal fixation. Since then, significant advancements in biological and mechanical science have refined these methods, leading to the modern approaches used in fracture fixation today.
Fracture Repair Biology
Inflammatory Phase (0-7 days)
Hemostasis: Immediately after a fracture, blood vessels are damaged, leading to bleeding. Platelets aggregate and form a clot to prevent further blood loss.
Inflammation: Inflammatory cells, including neutrophils, macrophages, and lymphocytes, invade the fracture site. Macrophages play a crucial role by clearing debris and secreting growth factors that stimulate healing.
Cytokine Release: Pro-inflammatory cytokines like interleukins and TNF-alpha are released to promote healing and attract mesenchymal stem cells (MSCs) to the site.
Soft Callus Formation (1-3 weeks)
Chondrogenesis: MSCs differentiate into chondrocytes (cartilage-forming cells). These cells create a fibrocartilaginous callus at the fracture site, stabilizing the bone ends.
Angiogenesis: New blood vessels begin to form to supply oxygen and nutrients to the healing tissue.
Collagen Deposition: Fibroblasts and osteoblasts secrete collagen, which forms a scaffold for the formation of soft callus.
Hard Callus Formation (3-12 weeks)
Ossification: Osteoblasts begin to convert the soft callus (made of cartilage) into bone tissue through a process called endochondral ossification.
Bone Formation: The cartilage is replaced with woven bone, a type of immature bone that is less dense but provides structural support.
Mineralization: Calcium and phosphate are deposited into the woven bone, solidifying the fracture repair.
Remodeling Phase (months to years)
Bone Remodeling: The newly formed bone is gradually replaced by mature, lamellar bone through the action of osteoclasts (which resorb bone) and osteoblasts (which form bone). This process restores the bone to its original shape and strength.
Restoration of Bone Architecture: The bone gradually regains its original strength and form, with the remodeling process continuing for months to years after the initial fracture.
Pins, Wires, and Screws

X ray image of ankle joint showing surgical treatment through internal fixation with plate and screw
Pins:
Purpose: Pins, also known as Kirschner wires (K-wires), are thin metal rods used to stabilize bone fragments during fracture healing. They are commonly used in situations where less rigid fixation is needed, such as in small bone fractures or in pediatric fractures.
Material: Typically made of stainless steel or titanium.
Insertion: Pins are inserted through the skin or directly into the bone using a percutaneous (through the skin) technique. In some cases, they may be inserted under general or regional anesthesia.
Use: They are particularly useful in fractures of the hands, feet, and wrist, and are often used in conjunction with other devices or after reduction (realignment) of the bone.
Wires
Purpose: Wires, particularly cerclage wires, are used to encircle or loop around bone fragments to hold them together. They are commonly used in long bone fractures or in pelvic fractures.
Material: Cerclage wires are usually made from stainless steel or titanium. They are flexible, allowing them to conform to the bone’s shape.
Types:
Single Wire Cerclage: One wire is passed around the bone, holding fragments together.
Figure-of-Eight Wires: Two wires used in an “X” pattern for better fixation.
Insertion: The wire is threaded through drilled holes in the bone or around the bone fragments. It is tightened to hold the bone in place.
Screws
Purpose: Screws are widely used in orthopedics for stabilizing fractures or securing bone fragments together. They are the most rigid and stable form of fixation.
Material: Commonly made of stainless steel, titanium, or other bio-compatible alloys.
Types:
Cortical Screws: Used for fixing bone to bone, typically in denser bone.
Cancellous Screws: Designed for use in spongy (cancellous) bone, providing a better grip due to their wider threads.
Self-tapping vs. Non-tapping Screws: Self-tapping screws can create their own threads as they are inserted into bone.
Locking Screws: These screws lock into place within a plate, providing additional stability.
Insertion: Screws are inserted using a drill to create pilot holes followed by screw insertion, often with the use of a plate for added support.
Plates
Plates are orthopedic implants used for internal fixation of fractures. They stabilize and support fractured bones by acting as a scaffold, allowing proper alignment and facilitating healing. Plates are typically made from materials like stainless steel or titanium to ensure strength, biocompatibility, and corrosion resistance.
They come in various types, each designed for specific fracture patterns and anatomical locations.
Dynamic Compression Plates (DCP): These are engineered to create compression at the fracture site, enhancing stability and promoting healing through their oval-shaped holes that allow screw angulation.
Locking Compression Plates (LCP): These combine the benefits of compression and locking mechanisms, providing superior stability even in osteoporotic or poor-quality bone by allowing screws to lock into the plate, reducing micromotion.
Neutralization Plates: These are used to protect fracture fixation achieved by screws, redistributing stress across the plate and preventing further damage. For fractures near joints or with significant shear forces.
Buttress Plates: These are essential, supporting bone fragments and preventing displacement under axial loads. In cases of comminuted fractures where anatomical reconstruction is challenging.
Bridge Plates: These span the fracture without directly compressing the fragments, preserving the periosteal blood supply and encouraging natural callus formation.
Tension-Band Principle:
The Tension-Band Principle is a biomechanical concept used in orthopedic surgery to convert tensile forces (pulling forces) acting on one side of a bone into compressive forces (pushing forces) on the opposite side. This principle enhances fracture stability and promotes healing by ensuring that the fracture site remains under compression, which is conducive to bone repair.
Key Elements of the Tension-Band Principle:
Tensile Forces: Many bones, especially in curved regions like the patella (kneecap) or olecranon (elbow), experience tensile forces on one side during movement or weight-bearing.
Conversion to Compression: By applying tension-band fixation, tensile forces are neutralized and redirected as compressive forces at the fracture site.
Compression for Healing: Compressive forces encourage direct bone healing by promoting stability and reducing micromotion at the fracture line.
Application of the Tension-Band Principle:
Devices Used:
Kirschner Wires (K-wires): Provide structural support and alignment.
Cerclage Wire or Stainless-Steel Loop: Acts as the tension band by wrapping around the bone and converting tensile forces.
Surgical Technique:
The K-wires are inserted to hold the bone fragments in place.
A flexible wire is looped in a figure-of-eight configuration around the bone fragments, anchored to the K-wires.
When the muscles or tendons apply tensile force during movement, the wire compresses the fracture site instead of pulling it apart.
Intramedullary Nails:
Intramedullary (IM) nails are orthopedic devices used for internal fixation of long bone fractures. These nails are inserted into the medullary canal (the hollow center of long bones) to provide stability and alignment, promoting healing while allowing early mobilization. IM nails are commonly used for fractures of the femur, tibia, humerus, and other long bones.
Types of Intramedullary Nails
Standard IM Nails:
Used for long bone fractures.
Provide basic stabilization and alignment.
Reconstruction Nails:
Designed for fractures involving both the shaft and adjacent joints (e.g., femoral neck fractures combined with femoral shaft fractures).
Interlocking Nails:
Include holes for screws at both ends to secure the nail in place, preventing rotation and shortening of the fracture.
Expandable Nails:
Expand once inside the bone, allowing fixation without the need for interlocking screws.
Proximal or Distal Femoral Nails:
Used for fractures closer to the hip or knee, with specific designs to fit these anatomical regions.
Humeral Nails:
Specifically designed for humeral shaft fractures, often shorter and narrower than femoral or tibial nails.
Tibial Nails:
Designed for tibial shaft fractures, with locking options to accommodate different fracture patterns.
Indications
Indications for IM Nails
Diaphyseal Fractures: Fractures along the shaft of long bones, particularly the femur and tibia.
Comminuted Fractures: Where multiple bone fragments need stabilization.
Segmental Fractures: Fractures with separate bone segments.
Pathologic Fractures: Fractures due to bone weakening from conditions like osteoporosis or tumors.
Nonunion and Malunion: To correct or stabilize poorly healed fractures.
Open Fractures: Commonly used due to minimal disruption of soft tissue.
Biodegradable Fixation
Biodegradable fixation refers to the use of implants made from materials that naturally degrade in the body over time. These materials are used to stabilize fractures, osteotomies, or soft tissue injuries during the healing process, after which they are absorbed and eliminated by the body, reducing the need for implant removal surgeries.
Materials Used in Biodegradable Fixation:
Polymers:
Polylactic Acid (PLA): Commonly used, with variants like PLLA (poly-L-lactic acid) for high strength.
Polyglycolic Acid (PGA): Degrades faster than PLA, often used in soft tissue applications.
Polycaprolactone (PCL): Offers slower degradation and flexibility.
Poly (lactic-co-glycolic acid) (PLGA): A combination of PLA and PGA, allowing customizable degradation rates.
Bioceramics:
Calcium Phosphate-Based Materials: Such as hydroxyapatite or tricalcium phosphate, often used in combination with polymers to promote bone regeneration.
Applications of Biodegradable Fixation
Orthopedics:
Fractures in non-load-bearing areas.
Pediatric fractures to avoid complications from implant removal.
Craniofacial Surgery:
Repair of fractures or reconstructive surgeries involving the skull or face.
Sports Medicine:
Tendon or ligament repairs, such as in rotator cuff or ACL surgeries.
Maxillofacial Surgery:
Fixation in jaw fractures or reconstructive procedures.
Contraindications
Outcomes

Throughout history, fractures have been treated using various methods, including immobilization, traction, amputation, and internal fixation. For most long-bone fractures, immobilization through casting, bracing, or splinting above and below the affected area was the standard approach except for femur fractures, which were primarily treated with traction. Open fractures and ballistic injuries involving long-bone fractures posed challenges for standard care due to the associated soft-tissue damage and difficulty in preventing infections, often leading to amputation as the preferred option.
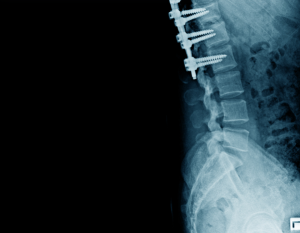
Lateral view of structure bone with internal fixation
The idea of internal fixation emerged in the mid-1800s, with Lister introducing open reduction and internal fixation (ORIF) for patella fractures in the 1860s. The use of plates, screws, and wires for fixation was first documented in the late 19th century. Early attempts at surgical fixation faced numerous challenges, including infections, poorly designed implants, metal allergies, and limited knowledge of the biological and mechanical aspects of fracture healing.
In the 1950s, Danis and Muller helped define the principles and techniques for internal fixation. Since then, significant advancements in biological and mechanical science have refined these methods, leading to the modern approaches used in fracture fixation today.
Fracture Repair Biology
Inflammatory Phase (0-7 days)
Hemostasis: Immediately after a fracture, blood vessels are damaged, leading to bleeding. Platelets aggregate and form a clot to prevent further blood loss.
Inflammation: Inflammatory cells, including neutrophils, macrophages, and lymphocytes, invade the fracture site. Macrophages play a crucial role by clearing debris and secreting growth factors that stimulate healing.
Cytokine Release: Pro-inflammatory cytokines like interleukins and TNF-alpha are released to promote healing and attract mesenchymal stem cells (MSCs) to the site.
Soft Callus Formation (1-3 weeks)
Chondrogenesis: MSCs differentiate into chondrocytes (cartilage-forming cells). These cells create a fibrocartilaginous callus at the fracture site, stabilizing the bone ends.
Angiogenesis: New blood vessels begin to form to supply oxygen and nutrients to the healing tissue.
Collagen Deposition: Fibroblasts and osteoblasts secrete collagen, which forms a scaffold for the formation of soft callus.
Hard Callus Formation (3-12 weeks)
Ossification: Osteoblasts begin to convert the soft callus (made of cartilage) into bone tissue through a process called endochondral ossification.
Bone Formation: The cartilage is replaced with woven bone, a type of immature bone that is less dense but provides structural support.
Mineralization: Calcium and phosphate are deposited into the woven bone, solidifying the fracture repair.
Remodeling Phase (months to years)
Bone Remodeling: The newly formed bone is gradually replaced by mature, lamellar bone through the action of osteoclasts (which resorb bone) and osteoblasts (which form bone). This process restores the bone to its original shape and strength.
Restoration of Bone Architecture: The bone gradually regains its original strength and form, with the remodeling process continuing for months to years after the initial fracture.
Pins, Wires, and Screws

X ray image of ankle joint showing surgical treatment through internal fixation with plate and screw
Pins:
Purpose: Pins, also known as Kirschner wires (K-wires), are thin metal rods used to stabilize bone fragments during fracture healing. They are commonly used in situations where less rigid fixation is needed, such as in small bone fractures or in pediatric fractures.
Material: Typically made of stainless steel or titanium.
Insertion: Pins are inserted through the skin or directly into the bone using a percutaneous (through the skin) technique. In some cases, they may be inserted under general or regional anesthesia.
Use: They are particularly useful in fractures of the hands, feet, and wrist, and are often used in conjunction with other devices or after reduction (realignment) of the bone.
Wires
Purpose: Wires, particularly cerclage wires, are used to encircle or loop around bone fragments to hold them together. They are commonly used in long bone fractures or in pelvic fractures.
Material: Cerclage wires are usually made from stainless steel or titanium. They are flexible, allowing them to conform to the bone’s shape.
Types:
Single Wire Cerclage: One wire is passed around the bone, holding fragments together.
Figure-of-Eight Wires: Two wires used in an “X” pattern for better fixation.
Insertion: The wire is threaded through drilled holes in the bone or around the bone fragments. It is tightened to hold the bone in place.
Screws
Purpose: Screws are widely used in orthopedics for stabilizing fractures or securing bone fragments together. They are the most rigid and stable form of fixation.
Material: Commonly made of stainless steel, titanium, or other bio-compatible alloys.
Types:
Cortical Screws: Used for fixing bone to bone, typically in denser bone.
Cancellous Screws: Designed for use in spongy (cancellous) bone, providing a better grip due to their wider threads.
Self-tapping vs. Non-tapping Screws: Self-tapping screws can create their own threads as they are inserted into bone.
Locking Screws: These screws lock into place within a plate, providing additional stability.
Insertion: Screws are inserted using a drill to create pilot holes followed by screw insertion, often with the use of a plate for added support.
Plates
Plates are orthopedic implants used for internal fixation of fractures. They stabilize and support fractured bones by acting as a scaffold, allowing proper alignment and facilitating healing. Plates are typically made from materials like stainless steel or titanium to ensure strength, biocompatibility, and corrosion resistance.
They come in various types, each designed for specific fracture patterns and anatomical locations.
Dynamic Compression Plates (DCP): These are engineered to create compression at the fracture site, enhancing stability and promoting healing through their oval-shaped holes that allow screw angulation.
Locking Compression Plates (LCP): These combine the benefits of compression and locking mechanisms, providing superior stability even in osteoporotic or poor-quality bone by allowing screws to lock into the plate, reducing micromotion.
Neutralization Plates: These are used to protect fracture fixation achieved by screws, redistributing stress across the plate and preventing further damage. For fractures near joints or with significant shear forces.
Buttress Plates: These are essential, supporting bone fragments and preventing displacement under axial loads. In cases of comminuted fractures where anatomical reconstruction is challenging.
Bridge Plates: These span the fracture without directly compressing the fragments, preserving the periosteal blood supply and encouraging natural callus formation.
Tension-Band Principle:
The Tension-Band Principle is a biomechanical concept used in orthopedic surgery to convert tensile forces (pulling forces) acting on one side of a bone into compressive forces (pushing forces) on the opposite side. This principle enhances fracture stability and promotes healing by ensuring that the fracture site remains under compression, which is conducive to bone repair.
Key Elements of the Tension-Band Principle:
Tensile Forces: Many bones, especially in curved regions like the patella (kneecap) or olecranon (elbow), experience tensile forces on one side during movement or weight-bearing.
Conversion to Compression: By applying tension-band fixation, tensile forces are neutralized and redirected as compressive forces at the fracture site.
Compression for Healing: Compressive forces encourage direct bone healing by promoting stability and reducing micromotion at the fracture line.
Application of the Tension-Band Principle:
Devices Used:
Kirschner Wires (K-wires): Provide structural support and alignment.
Cerclage Wire or Stainless-Steel Loop: Acts as the tension band by wrapping around the bone and converting tensile forces.
Surgical Technique:
The K-wires are inserted to hold the bone fragments in place.
A flexible wire is looped in a figure-of-eight configuration around the bone fragments, anchored to the K-wires.
When the muscles or tendons apply tensile force during movement, the wire compresses the fracture site instead of pulling it apart.
Intramedullary Nails:
Intramedullary (IM) nails are orthopedic devices used for internal fixation of long bone fractures. These nails are inserted into the medullary canal (the hollow center of long bones) to provide stability and alignment, promoting healing while allowing early mobilization. IM nails are commonly used for fractures of the femur, tibia, humerus, and other long bones.
Types of Intramedullary Nails
Standard IM Nails:
Used for long bone fractures.
Provide basic stabilization and alignment.
Reconstruction Nails:
Designed for fractures involving both the shaft and adjacent joints (e.g., femoral neck fractures combined with femoral shaft fractures).
Interlocking Nails:
Include holes for screws at both ends to secure the nail in place, preventing rotation and shortening of the fracture.
Expandable Nails:
Expand once inside the bone, allowing fixation without the need for interlocking screws.
Proximal or Distal Femoral Nails:
Used for fractures closer to the hip or knee, with specific designs to fit these anatomical regions.
Humeral Nails:
Specifically designed for humeral shaft fractures, often shorter and narrower than femoral or tibial nails.
Tibial Nails:
Designed for tibial shaft fractures, with locking options to accommodate different fracture patterns.
Indications for IM Nails
Diaphyseal Fractures: Fractures along the shaft of long bones, particularly the femur and tibia.
Comminuted Fractures: Where multiple bone fragments need stabilization.
Segmental Fractures: Fractures with separate bone segments.
Pathologic Fractures: Fractures due to bone weakening from conditions like osteoporosis or tumors.
Nonunion and Malunion: To correct or stabilize poorly healed fractures.
Open Fractures: Commonly used due to minimal disruption of soft tissue.
Biodegradable Fixation
Biodegradable fixation refers to the use of implants made from materials that naturally degrade in the body over time. These materials are used to stabilize fractures, osteotomies, or soft tissue injuries during the healing process, after which they are absorbed and eliminated by the body, reducing the need for implant removal surgeries.
Materials Used in Biodegradable Fixation:
Polymers:
Polylactic Acid (PLA): Commonly used, with variants like PLLA (poly-L-lactic acid) for high strength.
Polyglycolic Acid (PGA): Degrades faster than PLA, often used in soft tissue applications.
Polycaprolactone (PCL): Offers slower degradation and flexibility.
Poly (lactic-co-glycolic acid) (PLGA): A combination of PLA and PGA, allowing customizable degradation rates.
Bioceramics:
Calcium Phosphate-Based Materials: Such as hydroxyapatite or tricalcium phosphate, often used in combination with polymers to promote bone regeneration.
Applications of Biodegradable Fixation
Orthopedics:
Fractures in non-load-bearing areas.
Pediatric fractures to avoid complications from implant removal.
Craniofacial Surgery:
Repair of fractures or reconstructive surgeries involving the skull or face.
Sports Medicine:
Tendon or ligament repairs, such as in rotator cuff or ACL surgeries.
Maxillofacial Surgery:
Fixation in jaw fractures or reconstructive procedures.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



