Background
Gonadectomy is surgical procedure to remove gonads that produce eggs or sperm.
This procedure stops sex hormone production and causes sterility.
Castration has been performed for social, religious, or punitive reasons historically.
Gonadectomy suitable for intersex children and teenagers.
Laparoscopic gonadectomy is safe and effective for children and teenagers.
It eliminates risks of pregnancies, pyometra, and ovarian or uterine tumors.
Gonadectomy in males reduces perianal adenomas, benign prostatic hyperplasia, and certain sexually dimorphic behaviors.
Detailed risk profiles for post-gonadectomy weight gain aid veterinarians and owners in optimizing surgery timing and husbandry practices.
Establishing baseline risk of weight gain from sterilization aids evaluation of nonsurgical alternatives.
Effects of Gonadectomy as follows:
In Males:
Loss of muscle mass
Osteoporosis
Loss of libido
Mood changes
In Females:
Early menopause
Osteoporosis
Increased cardiovascular risk
Mood disturbances
Indications
For Males (Orchiectomy):
Testicular Cancer
Prostate Cancer
Severe Trauma or Infection
For Females (Oophorectomy):
Ovarian Cancer
Severe Endometriosis
Ovarian Cysts
Severe Pelvic Inflammatory Disease
Contraindications
Uncontrolled bleeding disorder
Severe cardiopulmonary instability
Active severe infection (sepsis)
Severe psychiatric disorder without capacity for consent
Poorly controlled diabetes
Obesity
History of extensive abdominal surgery
Severe osteoporosis (in oophorectomy)
Desire for future fertility
Outcomes
Gonadectomy outcomes depend on the procedure’s reason, patient health, and post-surgery use of hormone replacement therapy (HRT).
Gonadectomy enhances gender dysphoria, body satisfaction, and psychological well-being for many individuals.
It reduces ovarian cancer risk but slightly increases some non-reproductive cancers.
Equipment required
Incision Instruments
Dissection & Grasping Tissue forceps
Retractors Senn retractors
Laparoscope
Trocars
Graspers
Scissors
Energy Devic
Suction/Irrigation
Specimen Bag
Suture Materials
Electrosurgical Unit
Patient Preparation:
Patient assessment including medical history, medication review, and psychosocial and fertility counseling.
Hormonal therapies require adjustments for patients. Hormone therapy may pause before surgery per surgical team protocol.
Informed Consent:
Explain the procedure’s risks and potential complications clearly to the patient.
Patient Positioning:
Patients should be positioned in supine positions. General anesthesia is used.
Make sterile preparation of groin and scrotal area.
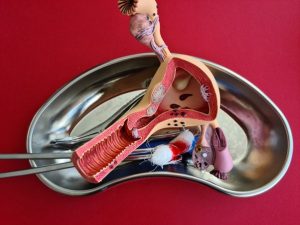
Surgery of genital organs

Reproductive organs
Technique
For Inguinal Orchiectomy:
Step 1: Incision
A small oblique shape incision is made over the inguinal canal.
Step 2: Identification of Spermatic Cord
The spermatic cord is isolated and ligated to prevent tumor spreading in cancer cases.
Step 3: Delivery of Testicle
Then testicles are mobilized and gently pulled out through the inguinal incision.
Avoid direct scrotal incision in suspected cancer cases to avoid seeding tumor cells.
Step 4: Ligation and Removal
The cord structures are double ligated with absorbable or non-absorbable sutures. Finally, testicles and cords are removed en bloc.
Step 5: Closure
At last layered closure of fascia, subcutaneous tissue, and skin.
For Laparoscopic Oophorectomy:
Step 1: Trocar Placement
Usually, 3 to 4 ports are required. For lower quadrants for working ports.
Step 2: Identification of Ovary
Ovary is visualized and gently mobilized. Then adjacent structures are identified to avoid injury.
Step 3: Ligation of Ovarian Pedicle
Blood supply is sealed and divided.
Step 4: Removal of Ovary
The ovary is detached from the fallopian tube and uterine attachments.
Then specimen is removed through an endobag to prevent spillage.
Step 5: Closure
Port sites are closed in layers.
Complications:
Bleeding
Injury to Adjacent Structures
Scrotal Hematoma
Vascular Compromise
Thromboembolism
Wound Dehiscence
Chronic Pain
Lymphocele
Incisional Hernia
Hormonal Deficiency Syndrome
Osteoporosis
Cardiovascular Disease
Sexual Dysfunction
Weight Gain & Metabolic Changes

Gonadectomy is surgical procedure to remove gonads that produce eggs or sperm.
This procedure stops sex hormone production and causes sterility.
Castration has been performed for social, religious, or punitive reasons historically.
Gonadectomy suitable for intersex children and teenagers.
Laparoscopic gonadectomy is safe and effective for children and teenagers.
It eliminates risks of pregnancies, pyometra, and ovarian or uterine tumors.
Gonadectomy in males reduces perianal adenomas, benign prostatic hyperplasia, and certain sexually dimorphic behaviors.
Detailed risk profiles for post-gonadectomy weight gain aid veterinarians and owners in optimizing surgery timing and husbandry practices.
Establishing baseline risk of weight gain from sterilization aids evaluation of nonsurgical alternatives.
Effects of Gonadectomy as follows:
In Males:
Loss of muscle mass
Osteoporosis
Loss of libido
Mood changes
In Females:
Early menopause
Osteoporosis
Increased cardiovascular risk
Mood disturbances
For Males (Orchiectomy):
Testicular Cancer
Prostate Cancer
Severe Trauma or Infection
For Females (Oophorectomy):
Ovarian Cancer
Severe Endometriosis
Ovarian Cysts
Severe Pelvic Inflammatory Disease
Uncontrolled bleeding disorder
Severe cardiopulmonary instability
Active severe infection (sepsis)
Severe psychiatric disorder without capacity for consent
Poorly controlled diabetes
Obesity
History of extensive abdominal surgery
Severe osteoporosis (in oophorectomy)
Desire for future fertility
Gonadectomy outcomes depend on the procedure’s reason, patient health, and post-surgery use of hormone replacement therapy (HRT).
Gonadectomy enhances gender dysphoria, body satisfaction, and psychological well-being for many individuals.
It reduces ovarian cancer risk but slightly increases some non-reproductive cancers.
Incision Instruments
Dissection & Grasping Tissue forceps
Retractors Senn retractors
Laparoscope
Trocars
Graspers
Scissors
Energy Devic
Suction/Irrigation
Specimen Bag
Suture Materials
Electrosurgical Unit
Patient Preparation:
Patient assessment including medical history, medication review, and psychosocial and fertility counseling.
Hormonal therapies require adjustments for patients. Hormone therapy may pause before surgery per surgical team protocol.
Informed Consent:
Explain the procedure’s risks and potential complications clearly to the patient.
Patient Positioning:
Patients should be positioned in supine positions. General anesthesia is used.
Make sterile preparation of groin and scrotal area.
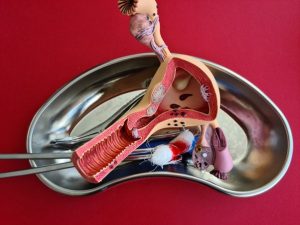
Surgery of genital organs

Reproductive organs
For Inguinal Orchiectomy:
Step 1: Incision
A small oblique shape incision is made over the inguinal canal.
Step 2: Identification of Spermatic Cord
The spermatic cord is isolated and ligated to prevent tumor spreading in cancer cases.
Step 3: Delivery of Testicle
Then testicles are mobilized and gently pulled out through the inguinal incision.
Avoid direct scrotal incision in suspected cancer cases to avoid seeding tumor cells.
Step 4: Ligation and Removal
The cord structures are double ligated with absorbable or non-absorbable sutures. Finally, testicles and cords are removed en bloc.
Step 5: Closure
At last layered closure of fascia, subcutaneous tissue, and skin.
For Laparoscopic Oophorectomy:
Step 1: Trocar Placement
Usually, 3 to 4 ports are required. For lower quadrants for working ports.
Step 2: Identification of Ovary
Ovary is visualized and gently mobilized. Then adjacent structures are identified to avoid injury.
Step 3: Ligation of Ovarian Pedicle
Blood supply is sealed and divided.
Step 4: Removal of Ovary
The ovary is detached from the fallopian tube and uterine attachments.
Then specimen is removed through an endobag to prevent spillage.
Step 5: Closure
Port sites are closed in layers.
Complications:
Bleeding
Injury to Adjacent Structures
Scrotal Hematoma
Vascular Compromise
Thromboembolism
Wound Dehiscence
Chronic Pain
Lymphocele
Incisional Hernia
Hormonal Deficiency Syndrome
Osteoporosis
Cardiovascular Disease
Sexual Dysfunction
Weight Gain & Metabolic Changes

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



