Background
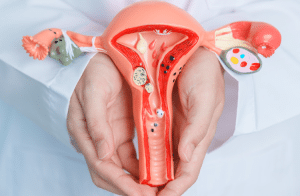
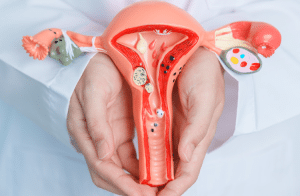
Hysterectomy is the common non-pregnancy-related major surgical intervention in the US which is involving the removal of the uterus, cervix, fallopian tubes, and ovaries. It address the conditions like uterine cancer and prolapse which cause excessive bleeding, and emotional distress.
Premenopausal women may experience sterility and post-surgery patients require hospitalization and a recovery period of 6-12 weeks. Potential complications include excessive bleeding, infections, and damage to nearby organs.
Indications
Myomas or uterine fibroids are noncancerous growths in the uterus that can cause pelvic discomfort and heavy monthly flow. If they are large and numerous a hysterectomy may be recommended for serious symptoms.
Abnormal uterine bleeding linked to hormonal abnormalities and adenomyosis that may necessitate a hysterectomy if other treatments such as medication or less invasive surgery fail to improve the symptoms.
Endometriosis is a disorder causing pelvic discomfort and infertility that potentially leading to a hysterectomy if medical treatments are ineffective and the discomfort is severe.
Adenomyosis is a disorder causing enlarged uterus with severe monthly flow and discomfort.
This procedure is considered when other treatment options wont work and also it depends on the cancer diagnosis and stage.
Contraindications
Outcomes
Hysterectomy is a procedure that can resolve various conditions such as endometriosis, uterine fibroids, irregular uterine bleeding, uterine prolapse, and certain malignancies.
It can also relieve symptoms such as persistent pelvic pressure, heavy menstrual flow, and pelvic discomfort.
If a woman has experienced incapacitating symptoms or discomfort before the procedure where hysterectomy can improve her quality of life.
Hysterectomy helps in preventing cancer as it provides the highest chance of healing and survival that potentially eradicating the cancer entirely.
Post-hysterectomy is a permanent infertility outcome as women cannot conceive if they wish to have children. Menopause may begin immediately if both ovaries are removed.
Epidеmiology
Hysterectomy is the most common for female patients with one in three US women expected to undergo it by age 60.
The younger women may also need hysterectomy for various medical reasons.
Indications for hysterectomy include malignancies, adenomyosis, and chronic pelvic discomfort.
The epidemiology of hysterectomy may be influenced by these specific indications.
Geographic variation in hysterectomy prevalence may be influenced by cultural, social, and healthcare system factors across different countries and areas.
Technique
Step 1: Patient preparation
The patient consents after a thorough medical assessment, their medical history and preferences are considered in discussing anesthesia options. During the procedure intravenous (IV) lines are implanted to provide fluids and drugs where the patient is ready for the operation.
Step 2: Incision
An incision made in the abdominal wall which may vary depending on the specifics and the type of incision (horizontal, vertical, or laparoscopic).
Step 3: Intrautеrinе Entry
The surgeon locates and isolates the uterine arteries in the abdominal cavity by ensuring minimal bleeding during the surgery by carefully cutting and tying off the blood veins.
Step 4: Removal of Utеrinе
The surgeon separates the uterus from its surrounding tissues and ligaments then removes it through an incision.
Step 5: Closing
The surgeon use the glue, staples, and sutures to seal the wound.
Hysterectomy
Complications
Antibiotics are administered before surgery to reduce the risk of infection in the pelvic region and at the site of surgery.
Excessive bleeding during or after surgery may necessitate additional operations to manage the bleeding.
Deep vein thrombosis and pulmonary embolism are significant health risks especially for those with risk factors. Preventing these issues can be achieved through blood thinners or special stockings.
The intestine may experience changes in movement or function especially if the operation affects the rectum or nearby tissues. Additionally, a complete hysterectomy may result in the vaginal vault falling or prolapsing into the vaginal canal by removing the cervix.
Post-opt some women may experience pelvic discomfort, sexual dysfunction, and menopausal symptoms like mood swings, hot flashes, and decreased bone density.
Sexual dysfunction may include decreased libido or uneasiness during sexual activity.
Additionally, by removing the ovaries can cause changes in bone density.
Medical Therapy
Utеrinе Fibroids:
NSAIDs, progestin-releasing IUDs, GnRH agonists, and birth control tablets help control discomfort and excessive menstrual flow.
Hormonal drugs like progestin releasing IUDs and GnRH agonists manage bleeding and shrink fibroids.
Uterine artery embolization is a minimally invasive technique that injects tiny particles into uterine arteries.
Endomеtriosis:
Painkillers used to treat pain while hormone therapy including GnRH agonists, hormonal IUDs, and birth control tablets can help to manage endometriosis symptoms.
Abnormal Utеrinе Bleeding:
Hormonal medications like progestin and hormonal IUDs can manage menstrual bleeding while nonhormonal drugs like NSAIDs can reduce severe bleeding.
Surgical Therapy
An abdominal hysterectomy is the most common type requires an incision in the abdominal wall to remove the uterus. This procedure is suitable for pelvic diseases, fibroids, or endometrial cancer.
Vaginal hysterectomy removes the uterus through the vaginal canal which is preferable for small uteri. Laparoscopy and vaginal surgery are combined in laparoscopically assisted vaginal hysterectomy (LAVH) which involves small abdominal incisions to place a laparoscope for viewing.
This minimal invasive procedure has a shorter recovery period due to minor incisions. Robot-assisted hysterectomy uses robotic arms for the operation providing improved dexterity and accuracy.
Both laparoscopic and vaginal hysterectomy procedures can be performed using this technique.
References
Abdominal Hysterectomy – StatPearls – NCBI Bookshelf (nih.gov)
Hysterectomy A Comprehensive Surgical Approach – PubMed (nih.gov)
Medication
Medication

Hysterectomy is the common non-pregnancy-related major surgical intervention in the US which is involving the removal of the uterus, cervix, fallopian tubes, and ovaries. It address the conditions like uterine cancer and prolapse which cause excessive bleeding, and emotional distress.
Premenopausal women may experience sterility and post-surgery patients require hospitalization and a recovery period of 6-12 weeks. Potential complications include excessive bleeding, infections, and damage to nearby organs.
Myomas or uterine fibroids are noncancerous growths in the uterus that can cause pelvic discomfort and heavy monthly flow. If they are large and numerous a hysterectomy may be recommended for serious symptoms.
Abnormal uterine bleeding linked to hormonal abnormalities and adenomyosis that may necessitate a hysterectomy if other treatments such as medication or less invasive surgery fail to improve the symptoms.
Endometriosis is a disorder causing pelvic discomfort and infertility that potentially leading to a hysterectomy if medical treatments are ineffective and the discomfort is severe.
Adenomyosis is a disorder causing enlarged uterus with severe monthly flow and discomfort.
This procedure is considered when other treatment options wont work and also it depends on the cancer diagnosis and stage.
Hysterectomy is a procedure that can resolve various conditions such as endometriosis, uterine fibroids, irregular uterine bleeding, uterine prolapse, and certain malignancies.
It can also relieve symptoms such as persistent pelvic pressure, heavy menstrual flow, and pelvic discomfort.
If a woman has experienced incapacitating symptoms or discomfort before the procedure where hysterectomy can improve her quality of life.
Hysterectomy helps in preventing cancer as it provides the highest chance of healing and survival that potentially eradicating the cancer entirely.
Post-hysterectomy is a permanent infertility outcome as women cannot conceive if they wish to have children. Menopause may begin immediately if both ovaries are removed.
Epidеmiology
Hysterectomy is the most common for female patients with one in three US women expected to undergo it by age 60.
The younger women may also need hysterectomy for various medical reasons.
Indications for hysterectomy include malignancies, adenomyosis, and chronic pelvic discomfort.
The epidemiology of hysterectomy may be influenced by these specific indications.
Geographic variation in hysterectomy prevalence may be influenced by cultural, social, and healthcare system factors across different countries and areas.
Step 1: Patient preparation
The patient consents after a thorough medical assessment, their medical history and preferences are considered in discussing anesthesia options. During the procedure intravenous (IV) lines are implanted to provide fluids and drugs where the patient is ready for the operation.
Step 2: Incision
An incision made in the abdominal wall which may vary depending on the specifics and the type of incision (horizontal, vertical, or laparoscopic).
Step 3: Intrautеrinе Entry
The surgeon locates and isolates the uterine arteries in the abdominal cavity by ensuring minimal bleeding during the surgery by carefully cutting and tying off the blood veins.
Step 4: Removal of Utеrinе
The surgeon separates the uterus from its surrounding tissues and ligaments then removes it through an incision.
Step 5: Closing
The surgeon use the glue, staples, and sutures to seal the wound.
Hysterectomy
Antibiotics are administered before surgery to reduce the risk of infection in the pelvic region and at the site of surgery.
Excessive bleeding during or after surgery may necessitate additional operations to manage the bleeding.
Deep vein thrombosis and pulmonary embolism are significant health risks especially for those with risk factors. Preventing these issues can be achieved through blood thinners or special stockings.
The intestine may experience changes in movement or function especially if the operation affects the rectum or nearby tissues. Additionally, a complete hysterectomy may result in the vaginal vault falling or prolapsing into the vaginal canal by removing the cervix.
Post-opt some women may experience pelvic discomfort, sexual dysfunction, and menopausal symptoms like mood swings, hot flashes, and decreased bone density.
Sexual dysfunction may include decreased libido or uneasiness during sexual activity.
Additionally, by removing the ovaries can cause changes in bone density.
Utеrinе Fibroids:
NSAIDs, progestin-releasing IUDs, GnRH agonists, and birth control tablets help control discomfort and excessive menstrual flow.
Hormonal drugs like progestin releasing IUDs and GnRH agonists manage bleeding and shrink fibroids.
Uterine artery embolization is a minimally invasive technique that injects tiny particles into uterine arteries.
Endomеtriosis:
Painkillers used to treat pain while hormone therapy including GnRH agonists, hormonal IUDs, and birth control tablets can help to manage endometriosis symptoms.
Abnormal Utеrinе Bleeding:
Hormonal medications like progestin and hormonal IUDs can manage menstrual bleeding while nonhormonal drugs like NSAIDs can reduce severe bleeding.
An abdominal hysterectomy is the most common type requires an incision in the abdominal wall to remove the uterus. This procedure is suitable for pelvic diseases, fibroids, or endometrial cancer.
Vaginal hysterectomy removes the uterus through the vaginal canal which is preferable for small uteri. Laparoscopy and vaginal surgery are combined in laparoscopically assisted vaginal hysterectomy (LAVH) which involves small abdominal incisions to place a laparoscope for viewing.
This minimal invasive procedure has a shorter recovery period due to minor incisions. Robot-assisted hysterectomy uses robotic arms for the operation providing improved dexterity and accuracy.
Both laparoscopic and vaginal hysterectomy procedures can be performed using this technique.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



