Background
Laparotomy decompression is typically a surgical intervention to relieve high pressure inside the abdominal cavity, which could be due to a medical condition known as ACS, or abdominal compartment syndrome. If left without treatment, impaired function of organs by high intra-abdominal pressures in ACS can be fatal.
Indications
Abdominal Compartment Syndrome (ACS):
In patients with chronic kidney disease with IAP persistently >20 mm Hg or other signs of end-organ dysfunction including decreased urine output, poor ventilation or worsening of acidosis. ACS can follow severe trauma, pancreatitis, sepsis or massive abdominal operations with the development of fluid collections or edema.
Severe Intra-Abdominal Hemorrhage: Some surgical cases, trauma or ruptured aneurysms with uncontrolled hemorrhage that results in raised IAP, anything that impacts on perfusion in other organs.
Severe Bowel Distention or Ischemia: Bowel obstruction or ischemia is typical for a situation where IAP is on the rise and demands performance of decompressive laparotomy in order not to worsen the state of the gastrointestinal tract and other affected organs.
Severe edema from Fluid Resuscitation: Patients with conditions necessitating vigorous fluid replacement such as the burn patient or septic patient often have capillary permeability and examine fluid into the peritoneal cavity, thereby increasing IAP.
Abdominal Trauma with Severe Swelling: Trauma patients with significant abdominal swelling from hemorrhage or swelling after blunt or penetrating trauma.
Contraindications
Coagulopathy: A bleeding diathesis or coagulopathy, for an open laparotomy will increase the risk of bleeding.
Hemodynamic Instability: There is always a risk that the patient with severe cardiovascular disease may not survive the procedure or the surgery necessary for anesthesia, which can directly signal the resulting changes in blood circulation during decompression.
Diffuse Peritonitis: While peritonitis itself is not a strict contraindication, severe, generalized infections within the abdominal cavity increase the risk of sepsis and complications, especially after opening the abdomen.
Inability to Control Infection Source: If increased IAP is secondary to an infectious source that cannot be adequately managed through surgery (such as extensive and non-surgically curable infection), laparotomy should be avoided.
Outcomes
Equipment
Self-Retaining Retractors
Decompression Needles and Cannulas
Suction Devices
Abdominal Wall Pressure Monitors
Laparotomy Sponges and Pads
Vacuum-Assisted Closure (VAC) Devices
Wound Protectors
Surgical Staplers and Suturing Devices
Patient preparation
Patient Assessment: Perform medical assessment focusing on the patient’s history and general body examination.
Observe for such symptoms as difficulty in breathing or hypoperfusion or shock- like symptoms.
Laboratory Tests: To start the diagnosis, Analyse basic laboratory investigations such as complete blood count, electrolyte levels, renal function and coagulation profile. If transfusion might be required, get the blood typed and crossmatched.
Informed Consent: Explain the procedure the risks involved, benefits of the procedure, and any other procedures which the concerned patient or guardian should consider.
Obtain informed consent.
Fasting: Make sure the patient has been fasting appropriately prior to surgery (minimum of 6-8 hours prior to the surgery).
Fluid Management: Give IV fluids if required regarding the volume status of the patient.
Medication Management: Give pre-operative medication, if any, in the following: antibiotic cover, antiemetic depending on the surgical procedure planned.
Patient position
Supine Position:
The patient lies flat on their back. This position provides optimal access to the abdomen for the surgeon.
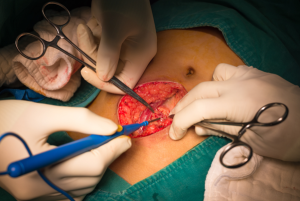
Technique
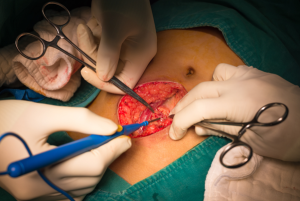
Laparotomy decompression
Step 1-Anesthesia and Positioning: It is recommended to induce a general anesthesia while closely observing the patient’s vital signs especially regarding their fluid and cardiovascular conditions.
Ensure that the patient is in supine position with their arms placed alongside their body to ensure that the abdominal cavity is fully exposed.
Step 2-Midline Incision: Make a vertical midline incision from the xiphoid process to the pubic symphysis.
The incision should be deep enough to enter the peritoneal cavity promptly to relieve pressure.
Step 3-Decompression: When opening the peritoneum make sure you regulate the release of the contents in the abdominal cavity.
Gradually decrease to prevent significant fluctuations of intra-abdominal pressure because this may cause hemodynamic compromise due to abrupt change in blood shift.
Step 4- Exploring and decompressing specific areas:
Once decompression is achieved, explore the abdominal contents methodically for identification of a source of compression or obstruction.
Drain any specific sources of intra-abdominal pressure, such as fluid collections, hematomas, or ischemic bowel loops.
Step 5-Temporary Closure with Vacuum-Assisted Dressing: Continue to use an abdominal closure device for temporary closure.
VAC dressings assist in prevention of fluid loss, chances of infection and keeping the abdominal area non-adherent in case of further assessment.
Step 6-Postoperative Monitoring and Support:
To monitor abdominal pressure, organ function and hemodynamic of the patient, transfer the patient to ICU.
Keep on supporting the posture with volume restoration or other relevant assistance such as ventilation as required.
Overlook for complications from a severe infection, bowel ischemia, or a reoccurrence of compartment syndrome.
Step 7-Definitive Closure:
Once intra-abdominal pressures have stabilized and the underlying problems are addressed, definitive abdominal closure can be considered.
This may require a delayed primary closure or staged closure based on the patient’s clinical stability and condition of the abdominal wall.
Complications
Infection: Postoperative infections, including wound, intra-abdominal abscess or sepsis, are frequent because internal organs are exposed. Complications such as infections can slow down their wound healing process and will worsen their condition.
Hemorrhage: Hemorrhage may be present either during or after the procedure if blood vessels or organs are accidentally injured. Hemorrhage may require open surgery, or blood transfusion in certain situations.
Bowel Injury: Injury of the intestines is a potential complication of spine surgery, and bowel perforation can cause leakage of its contents into the peritoneal cavity, resulting in peritonitis. This is a serious complication that may require further surgical intervention.
Abdominal Wall Dehiscence: There may be complete or partial rupture of the surgical wound together with evisceration which entails the protrusion of organs through the burn. This may well constitute an emergency and often additional surgery is needed.
Adhesions and Obstruction: Small bowel obstruction can occur in the future due to postoperative adhesions also known as scar tissue formation after laparotomy. Scar tissues are known to produce long term pain and may need further surgeries.
References
References

Laparotomy decompression is typically a surgical intervention to relieve high pressure inside the abdominal cavity, which could be due to a medical condition known as ACS, or abdominal compartment syndrome. If left without treatment, impaired function of organs by high intra-abdominal pressures in ACS can be fatal.
Abdominal Compartment Syndrome (ACS):
In patients with chronic kidney disease with IAP persistently >20 mm Hg or other signs of end-organ dysfunction including decreased urine output, poor ventilation or worsening of acidosis. ACS can follow severe trauma, pancreatitis, sepsis or massive abdominal operations with the development of fluid collections or edema.
Severe Intra-Abdominal Hemorrhage: Some surgical cases, trauma or ruptured aneurysms with uncontrolled hemorrhage that results in raised IAP, anything that impacts on perfusion in other organs.
Severe Bowel Distention or Ischemia: Bowel obstruction or ischemia is typical for a situation where IAP is on the rise and demands performance of decompressive laparotomy in order not to worsen the state of the gastrointestinal tract and other affected organs.
Severe edema from Fluid Resuscitation: Patients with conditions necessitating vigorous fluid replacement such as the burn patient or septic patient often have capillary permeability and examine fluid into the peritoneal cavity, thereby increasing IAP.
Abdominal Trauma with Severe Swelling: Trauma patients with significant abdominal swelling from hemorrhage or swelling after blunt or penetrating trauma.
Coagulopathy: A bleeding diathesis or coagulopathy, for an open laparotomy will increase the risk of bleeding.
Hemodynamic Instability: There is always a risk that the patient with severe cardiovascular disease may not survive the procedure or the surgery necessary for anesthesia, which can directly signal the resulting changes in blood circulation during decompression.
Diffuse Peritonitis: While peritonitis itself is not a strict contraindication, severe, generalized infections within the abdominal cavity increase the risk of sepsis and complications, especially after opening the abdomen.
Inability to Control Infection Source: If increased IAP is secondary to an infectious source that cannot be adequately managed through surgery (such as extensive and non-surgically curable infection), laparotomy should be avoided.
Self-Retaining Retractors
Decompression Needles and Cannulas
Suction Devices
Abdominal Wall Pressure Monitors
Laparotomy Sponges and Pads
Vacuum-Assisted Closure (VAC) Devices
Wound Protectors
Surgical Staplers and Suturing Devices
Patient preparation
Patient Assessment: Perform medical assessment focusing on the patient’s history and general body examination.
Observe for such symptoms as difficulty in breathing or hypoperfusion or shock- like symptoms.
Laboratory Tests: To start the diagnosis, Analyse basic laboratory investigations such as complete blood count, electrolyte levels, renal function and coagulation profile. If transfusion might be required, get the blood typed and crossmatched.
Informed Consent: Explain the procedure the risks involved, benefits of the procedure, and any other procedures which the concerned patient or guardian should consider.
Obtain informed consent.
Fasting: Make sure the patient has been fasting appropriately prior to surgery (minimum of 6-8 hours prior to the surgery).
Fluid Management: Give IV fluids if required regarding the volume status of the patient.
Medication Management: Give pre-operative medication, if any, in the following: antibiotic cover, antiemetic depending on the surgical procedure planned.
Patient position
Supine Position:
The patient lies flat on their back. This position provides optimal access to the abdomen for the surgeon.
Laparotomy decompression
Step 1-Anesthesia and Positioning: It is recommended to induce a general anesthesia while closely observing the patient’s vital signs especially regarding their fluid and cardiovascular conditions.
Ensure that the patient is in supine position with their arms placed alongside their body to ensure that the abdominal cavity is fully exposed.
Step 2-Midline Incision: Make a vertical midline incision from the xiphoid process to the pubic symphysis.
The incision should be deep enough to enter the peritoneal cavity promptly to relieve pressure.
Step 3-Decompression: When opening the peritoneum make sure you regulate the release of the contents in the abdominal cavity.
Gradually decrease to prevent significant fluctuations of intra-abdominal pressure because this may cause hemodynamic compromise due to abrupt change in blood shift.
Step 4- Exploring and decompressing specific areas:
Once decompression is achieved, explore the abdominal contents methodically for identification of a source of compression or obstruction.
Drain any specific sources of intra-abdominal pressure, such as fluid collections, hematomas, or ischemic bowel loops.
Step 5-Temporary Closure with Vacuum-Assisted Dressing: Continue to use an abdominal closure device for temporary closure.
VAC dressings assist in prevention of fluid loss, chances of infection and keeping the abdominal area non-adherent in case of further assessment.
Step 6-Postoperative Monitoring and Support:
To monitor abdominal pressure, organ function and hemodynamic of the patient, transfer the patient to ICU.
Keep on supporting the posture with volume restoration or other relevant assistance such as ventilation as required.
Overlook for complications from a severe infection, bowel ischemia, or a reoccurrence of compartment syndrome.
Step 7-Definitive Closure:
Once intra-abdominal pressures have stabilized and the underlying problems are addressed, definitive abdominal closure can be considered.
This may require a delayed primary closure or staged closure based on the patient’s clinical stability and condition of the abdominal wall.
Complications
Infection: Postoperative infections, including wound, intra-abdominal abscess or sepsis, are frequent because internal organs are exposed. Complications such as infections can slow down their wound healing process and will worsen their condition.
Hemorrhage: Hemorrhage may be present either during or after the procedure if blood vessels or organs are accidentally injured. Hemorrhage may require open surgery, or blood transfusion in certain situations.
Bowel Injury: Injury of the intestines is a potential complication of spine surgery, and bowel perforation can cause leakage of its contents into the peritoneal cavity, resulting in peritonitis. This is a serious complication that may require further surgical intervention.
Abdominal Wall Dehiscence: There may be complete or partial rupture of the surgical wound together with evisceration which entails the protrusion of organs through the burn. This may well constitute an emergency and often additional surgery is needed.
Adhesions and Obstruction: Small bowel obstruction can occur in the future due to postoperative adhesions also known as scar tissue formation after laparotomy. Scar tissues are known to produce long term pain and may need further surgeries.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



