Background
Surgical anastomosis related marginal ulceration is defined as ulceration at the margin of the sutured area of the gastrointestinal anastomosis. This condition is most frequently linked to surgeries which require the construction of anastomoses, including operations performed on the stomach, like gastric bypasses. Several factors contribute towards the development of marginal ulcers including abnormal exposure to gastric acid, use of NSAIDs, and H. pylori infection. These may be focalized in the abdomen and accompanied by nausea, vomiting or bleeding which may result into complications like obstruction or perforation. Endoscopy along with imaging studies and maybe biopsy is used in confirmation of the diagnosis in asymptomatic cases. Treatment includes the use of PPIs to decrease acid production, adjustments in medication use, and dietary changes.
Indications
Abdominal pain: They are characterized by being chronic or occurring in the upper abdomen, the severity of which may be aggravated by food intake.
Nausea and vomiting: Occasionally, it may leads to symptoms such as pains from the ulcer especially after taking a meal.
Gastrointestinal bleeding: Patient may be seen to have a black, tarry stool (melena) or even vomiting blood (hematemesis) due to ulcer formation.
Anemia: Due to long standing disease characterized by bleeding, which lead to fatigue, weakness and pallor.
Weight loss: Considering pain or nausea, which is obviously impossible to eat, even though conscious, can lead to unintentional weight loss.
Food intolerance: Inability to take some specific foods especially the solid ones due to discomfort in their digestive system.
Dyspepsia: It leads to feelings of discomfort in the stomach such as indigestion, bloating, or a burning sensation.
Contraindications
Use of Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Due to their action on prostaglandins which are protective for the stomach lining prostaglandin on NSAID such as ibuprofen, aspirin naproxen and many more should not be taken, worsens the ulcer formation or exacerbates an existing ulcer.
Smoking: Gastric acid production is increased, and smoking has effects on the healing process; thus, it is contraindicated in cases of marginal ulceration. It also inhibits the blood supply to the stomach lining thus delaying the ulcer’s healing.
Excessive Alcohol Consumption: Alcohol also has tendency to cause inflammation of the mucous membrane of stomach and stimulates acidity and thus worsens ulcers or slows down the healing. It should be avoided by patients with marginal ulceration and those with evidence of impaired renal function.
Corticosteroids (without gastroprotective agents): It may lead to gastro-intestinal ulceration; this is particularly the case when they are administered without PPIs. They should be taken with care and especially under doctor recommendation for patients who have history of marginal ulcers.
Outcomes
As for the outcomes of marginal ulceration, they depend on the diagnosis and further treatment. With proper use of medicines like proton pump inhibitors, change in lifestyle and reduction of NSAIDs use, it is possible to successfully treat most ulcers and get rid of the symptoms. However, it should be noted that marginal ulcers can recur, particularly if factors such as smoking, or undiagnosed and untreated Helicobacter pylori infection remain present. Bleeding or perforation may occur, and stenosis can develop necessitating endoscopic intervention or surgery. Rarely complications may extend to such an extent as to necessitate reoperation or cause malnutrition in patients. When cared for properly patients experience lessor symptoms or manifestations and improved quality of life, however, long-term maintenance may be required to avoid relapses. In most cases, such problems as perforation or severe bleeding may be lethal if the intervention of an experienced doctor or surgeon is not received.
Equipment
Endoscope: An endoscopic examination that is called upper gastrointestinal endoscopy is the method of choice to visualize the ulcer at the site of the anastomosis using a flexible tube with a camera. It makes it possible to assess the organ in question and take a biopsy if that is necessary.
Biopsy Forceps: An array of equipment that is applied during endoscopy to obtain tissues from the ulcerated area to exclude other causes including malignancy or infection by Helicobacter pylori.
Helicobacter pylori Testing Kits: Some screening tests include the endoscopy, where a biopsy is taken and examined for acute inflammation or the rapid urease tests or urea breath tests or the stool antigen tests for the presence of Helicobacter pylori which is a major cause of ulcer formation.
Radiologic Imaging (CT scan or X-ray): In case there is suspicion of complication like perforation then an abdominal X-ray or CT scan can be used to find out whether there is presence of free air which confirms perforation or other complications like obstruction.
Patient preparation
Preparation of the patient with marginal ulceration requires several general guidelines to achieve the most successful outcomes. Before any procedure such as endoscopy, patients are normally advised to fast for about 6 to 8 hours in order to have empty stomach thereby minimizing chances of aspiration and enhance visualization. It is necessary to review all the medications, and this includes stopping the use of NSAIDs and if the patient is on anticoagulants or antiplatelets their doses should be altered to reduce bleeding potential.
Administration of IV fluids may be required especially where the patient has been vomiting or if he has lost some blood. This includes forming the allergies especially to the sedatives or the anesthetics, and the patient must consent to serve as an informer after he or she is well informed of the risks and benefits that lie ahead of him or her in the procedure.
If surgery is needed, nutritional enhancement might be needed, especially in the case of the patient’s deficiency and smoking cessation is also essential as it contributes to slow the healing process. Follow up include management and administration of medications for example proton pump inhibitors, alteration of diet and follow up to check on the process of healing and preventing reoccurrence of the procedure.
Patient position
Endoscopy Positioning
Left Lateral Position (Recovery Position): When positioning the patient, the latter is usually in a left lateral position while the knees are moderately flexed. This position also ensures that the endoscope can easily pass through the esophagus and the stomach and minimizes aspiration. It also offers the best access to the upper gastrointestinal tract.
Surgical Positioning
Supine Position: Regarding abdominal surgeries involving marginal ulceration, most of the surgeries are carried out on patients lying in post-operative positions except in cases that involve revisional surgery or anastomosis repair in which the patient is positioned supine (lying on his/her back). It also offers the most satisfactory approach to the area that is the abdominal cavity.
Additional Positions: It should be realized that in cases where the surgeons need to access certain areas, or to ensure the patient’s safety and comfort during the procedure more positioning or padding may be needed. For instance, in laparoscopic surgery the patient may be positioned in slight Trendelenburg position that is head down and feet up assists in mobilizing organs in the abdomen out of operation area.
Post-Procedure Positioning
Recovery Position: Post endoscopy/surgical patients may be positioned in recovery position usually lying sideways left for better recovery and preventing aspiration in case they wake up from the effect of the administered sedatives.
Marginal ulceration
Technique
Diagnosis: It is therefore necessary to review some of the symptoms like abdominal pain, nausea, vomiting or even gastrointestinal bleed.
Endoscopy: Endoscopic evaluation should be done to examine the ulcer and its characteristics and to perform upper gastrointestinal endoscopy for this purpose the following steps should be taken.
Medical Management:
Proton Pump Inhibitors (PPIs): Begin high dose PPIs to minimize the secretion and plan for the healing process. These may be omeprazole, or lansoprazole, or another proton pump inhibitor as they are known.
H2-Receptor Antagonists: If PPIs are not sufficient one can consider the addition or substitution with H2-receptor antagonists like ranitidine.
Sucralfate: Give sucralfate as an adjunct to help coat the ulcer surface.
Address Contributing Factors:
Medication Review: If the patient is taking any medications such as NSAIDS or other medications that may cause formation of ulcer, the doctor should recommend discontinuation or change of the medication.
Dietary Modifications: Have a restricted diet and avoid the consumption of alcohol, caffeine and spicy food.
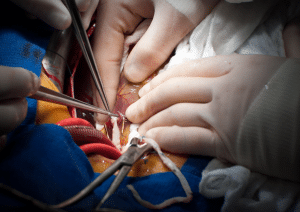
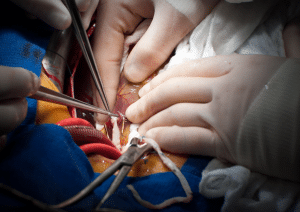
Surgical Intervention:
Revision Surgery: In the cases when medical intervention is not effective, it is possible to perform a surgical revision. This could involve:
Resection: Gut ablation which can be described as the surgical resection of the segment of the gastrointestinal tract.
Reconstruction: Changes in the anastomosis or modification of the approach that contributes to the minimization of pressure on the ulcerated region.
Follow-Up:
Ongoing Monitoring: Subsequent follow up with endoscopy to check on the epithelialization and to look for signs of restenosis.
Patient Education: Instruct patient about identification of symptoms of recurrence, the need to take the prescribed drugs, and changes in behaviour to avoid a relapse.
Approach considerations
The management of marginal ulceration is complex and should generally be based on a patient-centered approach. The treatment plan consists of the examination of a patient and their medical history, including the history of gastric operations, medications, and history of smoking or alcohol use. Medical management is then checked based on the clinical manifestations which include pain and bleed, and any complication like perforation or obstruction is effectively dealt with. Endoscopy applied for diagnosis is also very important with respect to visual assessment of the ulcer and the choice of the treatment regimen. The main course involves the treatment of the ulcer, and this is normally done using high power PPIs and if needed other complementary medicines such as sucralfate. Measures should be taken to eliminate underlying causes, including stopping ulcer-inducing drugs and altering the diet. If medical management remains ineffective, surgical procedures may be recommended and involve re-anastomosis or excision of the affected tissue. Closely related to follow-up care is the need for repeated endoscopies to assess the healing process and exclude a relapse, as well as for patient counselling on the signs that may indicate the onset of a recurrence and the importance of strict adherence to the prescribed treatment.
Complications
Gastrointestinal bleeding
Perforation
Obstruction
Stricture formation
Fistula formation
Infection

Surgical anastomosis related marginal ulceration is defined as ulceration at the margin of the sutured area of the gastrointestinal anastomosis. This condition is most frequently linked to surgeries which require the construction of anastomoses, including operations performed on the stomach, like gastric bypasses. Several factors contribute towards the development of marginal ulcers including abnormal exposure to gastric acid, use of NSAIDs, and H. pylori infection. These may be focalized in the abdomen and accompanied by nausea, vomiting or bleeding which may result into complications like obstruction or perforation. Endoscopy along with imaging studies and maybe biopsy is used in confirmation of the diagnosis in asymptomatic cases. Treatment includes the use of PPIs to decrease acid production, adjustments in medication use, and dietary changes.
Abdominal pain: They are characterized by being chronic or occurring in the upper abdomen, the severity of which may be aggravated by food intake.
Nausea and vomiting: Occasionally, it may leads to symptoms such as pains from the ulcer especially after taking a meal.
Gastrointestinal bleeding: Patient may be seen to have a black, tarry stool (melena) or even vomiting blood (hematemesis) due to ulcer formation.
Anemia: Due to long standing disease characterized by bleeding, which lead to fatigue, weakness and pallor.
Weight loss: Considering pain or nausea, which is obviously impossible to eat, even though conscious, can lead to unintentional weight loss.
Food intolerance: Inability to take some specific foods especially the solid ones due to discomfort in their digestive system.
Dyspepsia: It leads to feelings of discomfort in the stomach such as indigestion, bloating, or a burning sensation.
Use of Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Due to their action on prostaglandins which are protective for the stomach lining prostaglandin on NSAID such as ibuprofen, aspirin naproxen and many more should not be taken, worsens the ulcer formation or exacerbates an existing ulcer.
Smoking: Gastric acid production is increased, and smoking has effects on the healing process; thus, it is contraindicated in cases of marginal ulceration. It also inhibits the blood supply to the stomach lining thus delaying the ulcer’s healing.
Excessive Alcohol Consumption: Alcohol also has tendency to cause inflammation of the mucous membrane of stomach and stimulates acidity and thus worsens ulcers or slows down the healing. It should be avoided by patients with marginal ulceration and those with evidence of impaired renal function.
Corticosteroids (without gastroprotective agents): It may lead to gastro-intestinal ulceration; this is particularly the case when they are administered without PPIs. They should be taken with care and especially under doctor recommendation for patients who have history of marginal ulcers.
As for the outcomes of marginal ulceration, they depend on the diagnosis and further treatment. With proper use of medicines like proton pump inhibitors, change in lifestyle and reduction of NSAIDs use, it is possible to successfully treat most ulcers and get rid of the symptoms. However, it should be noted that marginal ulcers can recur, particularly if factors such as smoking, or undiagnosed and untreated Helicobacter pylori infection remain present. Bleeding or perforation may occur, and stenosis can develop necessitating endoscopic intervention or surgery. Rarely complications may extend to such an extent as to necessitate reoperation or cause malnutrition in patients. When cared for properly patients experience lessor symptoms or manifestations and improved quality of life, however, long-term maintenance may be required to avoid relapses. In most cases, such problems as perforation or severe bleeding may be lethal if the intervention of an experienced doctor or surgeon is not received.
Endoscope: An endoscopic examination that is called upper gastrointestinal endoscopy is the method of choice to visualize the ulcer at the site of the anastomosis using a flexible tube with a camera. It makes it possible to assess the organ in question and take a biopsy if that is necessary.
Biopsy Forceps: An array of equipment that is applied during endoscopy to obtain tissues from the ulcerated area to exclude other causes including malignancy or infection by Helicobacter pylori.
Helicobacter pylori Testing Kits: Some screening tests include the endoscopy, where a biopsy is taken and examined for acute inflammation or the rapid urease tests or urea breath tests or the stool antigen tests for the presence of Helicobacter pylori which is a major cause of ulcer formation.
Radiologic Imaging (CT scan or X-ray): In case there is suspicion of complication like perforation then an abdominal X-ray or CT scan can be used to find out whether there is presence of free air which confirms perforation or other complications like obstruction.
Patient preparation
Preparation of the patient with marginal ulceration requires several general guidelines to achieve the most successful outcomes. Before any procedure such as endoscopy, patients are normally advised to fast for about 6 to 8 hours in order to have empty stomach thereby minimizing chances of aspiration and enhance visualization. It is necessary to review all the medications, and this includes stopping the use of NSAIDs and if the patient is on anticoagulants or antiplatelets their doses should be altered to reduce bleeding potential.
Administration of IV fluids may be required especially where the patient has been vomiting or if he has lost some blood. This includes forming the allergies especially to the sedatives or the anesthetics, and the patient must consent to serve as an informer after he or she is well informed of the risks and benefits that lie ahead of him or her in the procedure.
If surgery is needed, nutritional enhancement might be needed, especially in the case of the patient’s deficiency and smoking cessation is also essential as it contributes to slow the healing process. Follow up include management and administration of medications for example proton pump inhibitors, alteration of diet and follow up to check on the process of healing and preventing reoccurrence of the procedure.
Endoscopy Positioning
Left Lateral Position (Recovery Position): When positioning the patient, the latter is usually in a left lateral position while the knees are moderately flexed. This position also ensures that the endoscope can easily pass through the esophagus and the stomach and minimizes aspiration. It also offers the best access to the upper gastrointestinal tract.
Surgical Positioning
Supine Position: Regarding abdominal surgeries involving marginal ulceration, most of the surgeries are carried out on patients lying in post-operative positions except in cases that involve revisional surgery or anastomosis repair in which the patient is positioned supine (lying on his/her back). It also offers the most satisfactory approach to the area that is the abdominal cavity.
Additional Positions: It should be realized that in cases where the surgeons need to access certain areas, or to ensure the patient’s safety and comfort during the procedure more positioning or padding may be needed. For instance, in laparoscopic surgery the patient may be positioned in slight Trendelenburg position that is head down and feet up assists in mobilizing organs in the abdomen out of operation area.
Post-Procedure Positioning
Recovery Position: Post endoscopy/surgical patients may be positioned in recovery position usually lying sideways left for better recovery and preventing aspiration in case they wake up from the effect of the administered sedatives.
Marginal ulceration
Diagnosis: It is therefore necessary to review some of the symptoms like abdominal pain, nausea, vomiting or even gastrointestinal bleed.
Endoscopy: Endoscopic evaluation should be done to examine the ulcer and its characteristics and to perform upper gastrointestinal endoscopy for this purpose the following steps should be taken.
Medical Management:
Proton Pump Inhibitors (PPIs): Begin high dose PPIs to minimize the secretion and plan for the healing process. These may be omeprazole, or lansoprazole, or another proton pump inhibitor as they are known.
H2-Receptor Antagonists: If PPIs are not sufficient one can consider the addition or substitution with H2-receptor antagonists like ranitidine.
Sucralfate: Give sucralfate as an adjunct to help coat the ulcer surface.
Address Contributing Factors:
Medication Review: If the patient is taking any medications such as NSAIDS or other medications that may cause formation of ulcer, the doctor should recommend discontinuation or change of the medication.
Dietary Modifications: Have a restricted diet and avoid the consumption of alcohol, caffeine and spicy food.
Surgical Intervention:
Revision Surgery: In the cases when medical intervention is not effective, it is possible to perform a surgical revision. This could involve:
Resection: Gut ablation which can be described as the surgical resection of the segment of the gastrointestinal tract.
Reconstruction: Changes in the anastomosis or modification of the approach that contributes to the minimization of pressure on the ulcerated region.
Follow-Up:
Ongoing Monitoring: Subsequent follow up with endoscopy to check on the epithelialization and to look for signs of restenosis.
Patient Education: Instruct patient about identification of symptoms of recurrence, the need to take the prescribed drugs, and changes in behaviour to avoid a relapse.
The management of marginal ulceration is complex and should generally be based on a patient-centered approach. The treatment plan consists of the examination of a patient and their medical history, including the history of gastric operations, medications, and history of smoking or alcohol use. Medical management is then checked based on the clinical manifestations which include pain and bleed, and any complication like perforation or obstruction is effectively dealt with. Endoscopy applied for diagnosis is also very important with respect to visual assessment of the ulcer and the choice of the treatment regimen. The main course involves the treatment of the ulcer, and this is normally done using high power PPIs and if needed other complementary medicines such as sucralfate. Measures should be taken to eliminate underlying causes, including stopping ulcer-inducing drugs and altering the diet. If medical management remains ineffective, surgical procedures may be recommended and involve re-anastomosis or excision of the affected tissue. Closely related to follow-up care is the need for repeated endoscopies to assess the healing process and exclude a relapse, as well as for patient counselling on the signs that may indicate the onset of a recurrence and the importance of strict adherence to the prescribed treatment.
Complications
Gastrointestinal bleeding
Perforation
Obstruction
Stricture formation
Fistula formation
Infection

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



