Background
Nasogastric intubation involves the placement of a tube from the outside through the nostrils down to the esophagus and terminating in the stomach. The NG tube is used for diagnostic and therapeutic purposes and maybe inserted for the evacuation of gastric contents, medication administration, or nutrition supply and for aspirations of the gastric contents.

Indications
Gastric Decompression: This is done to relieve pressure caused by accumulated air or fluid in the stomach that is usually associated with bowel obstruction, ileus, or postoperative care.
Medication and Nutrient Administration: This tube applies to patients where swallowing is not possible, or in conditions where the gastrointestinal system is impaired but still needing nourishment.
Gastric lavage: NG intubation can be utilized for the washing out of the stomach in cases of poisoning and overdose.
Aspiration of Gastric Contents: This is done to avoid aspiration for those patients who have the risk of vomiting or a decreased level of consciousness.
Contraindications
Severe Facial Trauma: Especially injury to the nasal passages or fracture of the midface (Le Fort fractures), because it may be associated with increased risk of incorrect tube placement and further injury.
Esophageal Varices: Esophageal varices are those varices that carry a high risk of rupture with heavy internal bleeding of the patient.
Esophageal Strictures or Obstructions: Insertion of the NG tube may cause perforation or worsen the obstruction.
Recent Nasal or Esophageal Surgery: Recent surgery to the nose or esophagus may result in a high risk of disrupting the surgical site or healing tissues.
Severe Coagulopathy: The risk of bleeding during the time of insertion is higher in cases of significant bleeding disorders.
Outcomes
Equipment
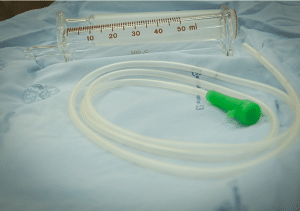
NG tube (various sizes, usually 10-18 French gauge for adults).
Emesis basin or plastic bag
Suction tubing and container
Gloves and other protective equipment.
Cup of water with a straw (if patient is conscious and able to swallow).
Tape or fixation device.
Syringe (usually 20-50 mL).
pH testing strips (to confirm tube placement).
Water-soluble lubricant
Patient Preparation
Explain the Procedure:
Explain the purpose of the NG intubation to the patient, such as to remove stomach contents, administer medications or provide nutrition.
Describe the procedure, what to expect and any sensations that may be experienced including gagging or discomfort.
Answer all the questions and address any concerns the patient may have to minimize anxiety.
Informed Consent
The patient should be informed about the risks and benefits of the procedure, as well as its alternatives.
Assess the Patient
Rule out contraindications like nasal or facial fractures, nasal surgery within the last six months, esophageal varices.
Past Medical History: Review for history of medical conditions and allergies.
Physical Examination
Nasal patency-look for obstruction in the nasal passages; check also for septal deviation.
Patient position
The patient should be seated straight with a somewhat flexed neck.
Make the patient comfortable and support the head and neck.
Technique
Step 1: Preparation:
Explain the procedure to the patient to minimize anxiety and obtain consent.
The patient should be seated straight with a somewhat flexed neck.
The length of the tube to be inserted in the patient should be measured from the tip of the nose to the ear lobe and then down to the xiphoid process (lower end of the sternum), marking this length on the tube with tape or a marker.
Step 2: Insertion:
Apply water-soluble lubricant to the distal end of the NG tube.
Insert the tube into the nostril with the head tilted forward; this position facilitates an easy navigation of the tube through the nasal cavity.
Guide the tube along the nasal floor and gently thread the tube backward toward the back of the throat.
As the tube approaches the oropharynx, the patient will start to cough or gag. Stop and ask the patient to sip water and swallow. This helps advance the tube into the esophagus instead of the trachea.
Continue to advance the tube to the premeasured length.
Step 3: Verification of Placement:
Aspirate gastric contents using a syringe and test the pH. A pH of less than 5 typically indicates proper placement in the stomach.
Alternatively, confirm placement with auscultation (listening for air injected into the tube) or imaging (e.g., chest X-ray).
Step 4: Securing the Tube:
Secure the tube to the nose or cheek using adhesive tape or a commercial fixation device.
The tube should not be kinked, and it should be well-secured to prevent dislodgment.
Step 5: Post procedure Care:
The patient is monitored for discomfort, respiratory distress, or complications.
The tube is regularly checked for patency and proper function.
Complications
Nasal and Throat Irritation or Injury:
Nasal mucosal injury: It may cause bleeding, discomfort, or ulceration.
Sore throat and hoarseness can be caused by irritation of the oropharynx.
Misplacement or Displacement of the Tube:
Pulmonary placement: Sometimes the tube may be placed inadvertently into the trachea or bronchus and may cause severe complications like aspiration pneumonia or pneumothorax.
Coiling in the esophagus: This may lead to inadequate drainage or feeding.
Sinusitis and Otitis Media:
Sinusitis may arise due to impaired sinus drainage with prolonged intubation.
Ear infections may arise from the communication between the nasopharynx and the middle ear.
Esophageal Complications:
Esophageal perforation or rupture: A rare but potentially serious event, especially in the presence of some esophageal disorders
Esophagitis: This is an infection and inflammation of the esophagus as a result of an indwelling tube.
Gastrointestinal complications:
Gastric or duodenal ulcerations: Due to a pressure sore or constant irritation by the tube.
This is specifically true in cases of aspiration of gastric contents when the tube has been used for feeding in patients with impaired consciousness or swallowing dysfunction.

Nasogastric intubation involves the placement of a tube from the outside through the nostrils down to the esophagus and terminating in the stomach. The NG tube is used for diagnostic and therapeutic purposes and maybe inserted for the evacuation of gastric contents, medication administration, or nutrition supply and for aspirations of the gastric contents.

Gastric Decompression: This is done to relieve pressure caused by accumulated air or fluid in the stomach that is usually associated with bowel obstruction, ileus, or postoperative care.
Medication and Nutrient Administration: This tube applies to patients where swallowing is not possible, or in conditions where the gastrointestinal system is impaired but still needing nourishment.
Gastric lavage: NG intubation can be utilized for the washing out of the stomach in cases of poisoning and overdose.
Aspiration of Gastric Contents: This is done to avoid aspiration for those patients who have the risk of vomiting or a decreased level of consciousness.
Severe Facial Trauma: Especially injury to the nasal passages or fracture of the midface (Le Fort fractures), because it may be associated with increased risk of incorrect tube placement and further injury.
Esophageal Varices: Esophageal varices are those varices that carry a high risk of rupture with heavy internal bleeding of the patient.
Esophageal Strictures or Obstructions: Insertion of the NG tube may cause perforation or worsen the obstruction.
Recent Nasal or Esophageal Surgery: Recent surgery to the nose or esophagus may result in a high risk of disrupting the surgical site or healing tissues.
Severe Coagulopathy: The risk of bleeding during the time of insertion is higher in cases of significant bleeding disorders.
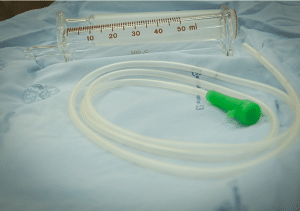
NG tube (various sizes, usually 10-18 French gauge for adults).
Emesis basin or plastic bag
Suction tubing and container
Gloves and other protective equipment.
Cup of water with a straw (if patient is conscious and able to swallow).
Tape or fixation device.
Syringe (usually 20-50 mL).
pH testing strips (to confirm tube placement).
Water-soluble lubricant
Explain the Procedure:
Explain the purpose of the NG intubation to the patient, such as to remove stomach contents, administer medications or provide nutrition.
Describe the procedure, what to expect and any sensations that may be experienced including gagging or discomfort.
Answer all the questions and address any concerns the patient may have to minimize anxiety.
Informed Consent
The patient should be informed about the risks and benefits of the procedure, as well as its alternatives.
Assess the Patient
Rule out contraindications like nasal or facial fractures, nasal surgery within the last six months, esophageal varices.
Past Medical History: Review for history of medical conditions and allergies.
Physical Examination
Nasal patency-look for obstruction in the nasal passages; check also for septal deviation.
The patient should be seated straight with a somewhat flexed neck.
Make the patient comfortable and support the head and neck.
Step 1: Preparation:
Explain the procedure to the patient to minimize anxiety and obtain consent.
The patient should be seated straight with a somewhat flexed neck.
The length of the tube to be inserted in the patient should be measured from the tip of the nose to the ear lobe and then down to the xiphoid process (lower end of the sternum), marking this length on the tube with tape or a marker.
Step 2: Insertion:
Apply water-soluble lubricant to the distal end of the NG tube.
Insert the tube into the nostril with the head tilted forward; this position facilitates an easy navigation of the tube through the nasal cavity.
Guide the tube along the nasal floor and gently thread the tube backward toward the back of the throat.
As the tube approaches the oropharynx, the patient will start to cough or gag. Stop and ask the patient to sip water and swallow. This helps advance the tube into the esophagus instead of the trachea.
Continue to advance the tube to the premeasured length.
Step 3: Verification of Placement:
Aspirate gastric contents using a syringe and test the pH. A pH of less than 5 typically indicates proper placement in the stomach.
Alternatively, confirm placement with auscultation (listening for air injected into the tube) or imaging (e.g., chest X-ray).
Step 4: Securing the Tube:
Secure the tube to the nose or cheek using adhesive tape or a commercial fixation device.
The tube should not be kinked, and it should be well-secured to prevent dislodgment.
Step 5: Post procedure Care:
The patient is monitored for discomfort, respiratory distress, or complications.
The tube is regularly checked for patency and proper function.
Nasal and Throat Irritation or Injury:
Nasal mucosal injury: It may cause bleeding, discomfort, or ulceration.
Sore throat and hoarseness can be caused by irritation of the oropharynx.
Misplacement or Displacement of the Tube:
Pulmonary placement: Sometimes the tube may be placed inadvertently into the trachea or bronchus and may cause severe complications like aspiration pneumonia or pneumothorax.
Coiling in the esophagus: This may lead to inadequate drainage or feeding.
Sinusitis and Otitis Media:
Sinusitis may arise due to impaired sinus drainage with prolonged intubation.
Ear infections may arise from the communication between the nasopharynx and the middle ear.
Esophageal Complications:
Esophageal perforation or rupture: A rare but potentially serious event, especially in the presence of some esophageal disorders
Esophagitis: This is an infection and inflammation of the esophagus as a result of an indwelling tube.
Gastrointestinal complications:
Gastric or duodenal ulcerations: Due to a pressure sore or constant irritation by the tube.
This is specifically true in cases of aspiration of gastric contents when the tube has been used for feeding in patients with impaired consciousness or swallowing dysfunction.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



