Background
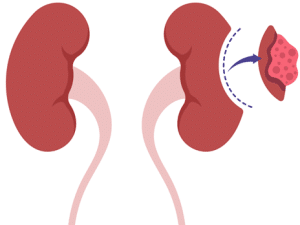
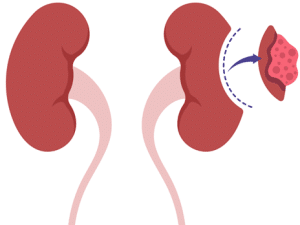
Nephrectomy is a surgical procedure that aims to remove partially or completely one or both kidneys, which serves as a vital procedure in addressing a spectrum of renal ailments. This span from benign growths to advanced cancers with significant injuries and dysfunctional kidneys. The approach to nephrectomy varies encompassing open surgery, laparoscopic methods, or robot-assisted techniques. The choice among these options hinges on factors like specific ailment, overall health, and proficiency of the surgical team.
Nephrectomy
Since its emergence in late 1800s, nephrectomy has developed by its benefits from advancements in surgical methods, anesthesia, and peri-operative management. These enhancements have contributed to better patient results and decreased morbidity rates.
Indications
Renal Cancer: Nephrectomy manages renal cell carcinoma which is a prevalent form of kidney cancer. The choice between partial or radical nephrectomy depends on factors like tumor stage and location.
Kidney Trauma: Serious kidney injuries stemming from trauma such as accidents or penetrating wounds may necessitate nephrectomy, in cases where conventional treatments prove ineffective in managing bleeding or when there is considerable damage to the kidney tissue.
Kidney Stones: In cases involving extensive and recurring kidney stones resistant to conventional treatments such as medication, lithotripsy, and nephrectomy might be contemplated as a viable option to relieve symptoms that avert potential complications.
Kidney Function: Nephrectomy may be required in cases of chronic kidney disease or end-stage renal disease when one kidney is significantly damaged, non-functional, and remaining kidney is unable to sustain sufficient renal function on its own.
Infection: Persistent kidney infections like pyelonephritis which fails to improve antibiotic treatment that may necessitate nephrectomy as a measure to eliminate the infected kidney and avert potential systemic complications.
Hypertension: When hypertension stemming from renal artery stenosis or other renal vascular conditions that remains uncontrollable despite attempts with medication or interventional procedures, where nephrectomy may be considered as a final option to regulate blood pressure.
Contraindications
Outcomes
Equipment
Surgical Instruments:
Anesthesia Equipment:
Imaging Equipment (if needed):
Monitoring Equipment:
Surgical Drapes and Sterile Supplies:
Sterile surgical drapes: To create a sterile field around the surgical site.
Sterile gloves and gowns for the surgical team.
Sterile towels and packs.
Suction Equipment:
Surgical suction device: To remove blood and fluids from the surgical site.
Laparoscopic Equipment (for laparoscopic nephrectomy):
Patient preparation
Initial Consultation and Assessment: The patient will meet healthcare provider typically a urologist or surgeon who will discuss the necessity of nephrectomy, risks, benefits, and alternatives. The patient’s medical history, medications, allergies, and pre-existing conditions will be reviewed.
Pre-operative Evaluation: The patient will undergo a comprehensive pre-operative evaluation to assess their overall health status and suitability for surgery. This may include a physical examination, electrocardiogram (ECG), chest X-ray, and other tests determined by the healthcare team.
Medication Review: The patient should inform their healthcare provider about all medications including prescription, over-the-counter, and herbal supplements. Some medications may need to be adjusted or temporarily stopped before surgery blood thinners or medications that affect blood pressure.
Informed Consent: Following the patient’s explanation of procedure’s risks, advantages, and alternatives the patient will be asked to sign a consent form before the surgery.
Patient position
The patient is placed under lateral decubitus position with the side of kidney to be removed facing upwards.
Technique
Open nephrectomy technique
Step 1: The usual practice involves administering general anesthesia to the patient to ensure their unconsciousness and freedom from pain-free throughout the procedure. The surgical team also prepares the area around kidney by cleaning and sterilizing it to reduce the risk of infection.
Step 2: The surgeon makes a large incision in the abdomen or flank, usually on the side of the affected kidney.
Step 3: After the incision, the surgeon carefully moves aside muscles, tissues, and other organs to expose the kidney and surrounding structures. This step requires precision to avoid damaging nearby organs and blood vessels.
Step 4: Once the kidney is exposed, the surgeon identifies and clamps the renal artery and vein which supply blood to the kidney. Clamping these blood vessels helps minimize blood loss during the procedure.
Step 5: The surgeon carefully dissects the kidney from the surrounding tissues by taking care to avoid damaging nearby structures such as the ureter and major blood vessels. Once the kidney is completely freed from its attachments and it is removed from the body through the incision.
Step 6: Following the removal of the kidney, surgeon proceeds to close the incision either by suturing or using staples. Occasionally, a drainage tube might be placed in the vicinity of surgical area to facilitate the removal of surplus fluids and mitigate risk of fluid accumulation including blood.
Laparoscopic nephrectomy technique
Step 1: Patient positioning and equipment check
The patient is under general anesthesia and positioned in a lateral decubitus position with the side of the kidney to be removed facing upwards.
The surgeon and surgical team will ensure that all the equipment including the laparoscope, camera, trocars, and surgical instruments is properly functioning.
Step 2: Veress needle and trocar placement
A small Veress needle, is inserted into the abdomen to create a pneumoperitoneum a CO2 insufflation that creates space for the laparoscope and instruments.
After the establishment of pneumoperitoneum, a trocar is a hollow tube is introduced through the incision to facilitate and insert the laparoscope. Subsequently, additional trocars are strategically positioned in different areas of abdomen to enable the passage of surgical instruments.
Step 3: Mobilization of the colon
The colon, the large intestine is carefully dissected and moved away from the kidney to expose the renal artery and vein.
Step 4: Identification of the ureter and gonadal vein
The gonadal vein, which drains blood from the testicles or ovaries and the ureter, the kidney’s tube that transports urine to the bladder which is identified & dissected.
Step 5: Renal hilar dissection
The renal hilum serves as the region through which both ureter and blood vessels traverse in their entry and exit from kidney. This is the most critical part of surgery as meticulous dissection is required to identify and isolate the renal artery and vein.
Once the renal artery and vein are isolated they are clipped or tied off with sutures to stop blood flow to the kidney.
Step 6: Remaining renal attachments dissection
The remaining attachments of the kidney such as fatty tissue and ligaments are carefully dissected and divided.
Step 7: Specimen removal
The kidney is then removed through one of the trocar incision sites which may be enlarged if necessary.
Step 8: Closure
The CO2 gas is insufflated from the abdomen and the trocars are removed. The small incision sites are closed with sutures or staples.
Laboratory tests
Complete Blood Count: This examination offers insights into the number and types of blood cells present including RBC’s, WBC’s, & platelets. Abnormalities in these levels can indicate various conditions that may affect the surgery or the patient’s ability to heal afterward.
BMP and CMP: These panels examine a range of blood components such as blood urea nitrogen, creatinine, glucose, electrolytes, and indicators of renal function. Abnormal levels may indicate kidney dysfunction or other conditions that could affect the surgery.
Coagulation Studies: These tests assess the blood’s ability to clot including PT and aPTT. To reduce the chance of bleeding issues both during and after the procedure it is crucial to assess coagulation status prior to surgery.
Urinalysis: Analysis of urine can provide information about kidney function, urinary tract infections, and other kidney-related conditions. It may include examination of urine sediment, urine pH, protein levels, and the presence of blood or bacteria.
Imaging Studies: Various imaging techniques including ultrasound, CT scans, and MRI may be prescribed to assess both the structure and functionality of the kidneys and adjacent organs. These studies help the surgical team to plan procedure and identify any abnormalities that may affect the surgery.
Complications
Bleeding: One possible side effect of surgery is excessive bleeding during or after the procedure.
Infection: There is a chance of infection with any surgical operation. This can occur at the site of incision or internally. Antibiotics are often administered before, during, and after surgery to prevent infection.
Pain: Pain is common after nephrectomy. While pain management strategies are employed some patients may experience significant discomfort in the immediate post-operative period.
Blood clots: Following surgical procedures the individuals may be at risk of developing blood clots in their legs known as deep vein thrombosis (DVT) or experiencing a pulmonary embolism (PE) these clots migrate to the lungs. This risk is particularly heightened when patients remain immobile for prolonged periods post-surgery.
Urinary complications: After nephrectomy, there may be changes in urinary function. These can include urinary retention, urinary tract infections, or incontinence.

Nephrectomy is a surgical procedure that aims to remove partially or completely one or both kidneys, which serves as a vital procedure in addressing a spectrum of renal ailments. This span from benign growths to advanced cancers with significant injuries and dysfunctional kidneys. The approach to nephrectomy varies encompassing open surgery, laparoscopic methods, or robot-assisted techniques. The choice among these options hinges on factors like specific ailment, overall health, and proficiency of the surgical team.
Nephrectomy
Since its emergence in late 1800s, nephrectomy has developed by its benefits from advancements in surgical methods, anesthesia, and peri-operative management. These enhancements have contributed to better patient results and decreased morbidity rates.
Renal Cancer: Nephrectomy manages renal cell carcinoma which is a prevalent form of kidney cancer. The choice between partial or radical nephrectomy depends on factors like tumor stage and location.
Kidney Trauma: Serious kidney injuries stemming from trauma such as accidents or penetrating wounds may necessitate nephrectomy, in cases where conventional treatments prove ineffective in managing bleeding or when there is considerable damage to the kidney tissue.
Kidney Stones: In cases involving extensive and recurring kidney stones resistant to conventional treatments such as medication, lithotripsy, and nephrectomy might be contemplated as a viable option to relieve symptoms that avert potential complications.
Kidney Function: Nephrectomy may be required in cases of chronic kidney disease or end-stage renal disease when one kidney is significantly damaged, non-functional, and remaining kidney is unable to sustain sufficient renal function on its own.
Infection: Persistent kidney infections like pyelonephritis which fails to improve antibiotic treatment that may necessitate nephrectomy as a measure to eliminate the infected kidney and avert potential systemic complications.
Hypertension: When hypertension stemming from renal artery stenosis or other renal vascular conditions that remains uncontrollable despite attempts with medication or interventional procedures, where nephrectomy may be considered as a final option to regulate blood pressure.
Surgical Instruments:
Anesthesia Equipment:
Imaging Equipment (if needed):
Monitoring Equipment:
Surgical Drapes and Sterile Supplies:
Sterile surgical drapes: To create a sterile field around the surgical site.
Sterile gloves and gowns for the surgical team.
Sterile towels and packs.
Suction Equipment:
Surgical suction device: To remove blood and fluids from the surgical site.
Laparoscopic Equipment (for laparoscopic nephrectomy):
Initial Consultation and Assessment: The patient will meet healthcare provider typically a urologist or surgeon who will discuss the necessity of nephrectomy, risks, benefits, and alternatives. The patient’s medical history, medications, allergies, and pre-existing conditions will be reviewed.
Pre-operative Evaluation: The patient will undergo a comprehensive pre-operative evaluation to assess their overall health status and suitability for surgery. This may include a physical examination, electrocardiogram (ECG), chest X-ray, and other tests determined by the healthcare team.
Medication Review: The patient should inform their healthcare provider about all medications including prescription, over-the-counter, and herbal supplements. Some medications may need to be adjusted or temporarily stopped before surgery blood thinners or medications that affect blood pressure.
Informed Consent: Following the patient’s explanation of procedure’s risks, advantages, and alternatives the patient will be asked to sign a consent form before the surgery.
The patient is placed under lateral decubitus position with the side of kidney to be removed facing upwards.
Open nephrectomy technique
Step 1: The usual practice involves administering general anesthesia to the patient to ensure their unconsciousness and freedom from pain-free throughout the procedure. The surgical team also prepares the area around kidney by cleaning and sterilizing it to reduce the risk of infection.
Step 2: The surgeon makes a large incision in the abdomen or flank, usually on the side of the affected kidney.
Step 3: After the incision, the surgeon carefully moves aside muscles, tissues, and other organs to expose the kidney and surrounding structures. This step requires precision to avoid damaging nearby organs and blood vessels.
Step 4: Once the kidney is exposed, the surgeon identifies and clamps the renal artery and vein which supply blood to the kidney. Clamping these blood vessels helps minimize blood loss during the procedure.
Step 5: The surgeon carefully dissects the kidney from the surrounding tissues by taking care to avoid damaging nearby structures such as the ureter and major blood vessels. Once the kidney is completely freed from its attachments and it is removed from the body through the incision.
Step 6: Following the removal of the kidney, surgeon proceeds to close the incision either by suturing or using staples. Occasionally, a drainage tube might be placed in the vicinity of surgical area to facilitate the removal of surplus fluids and mitigate risk of fluid accumulation including blood.
Laparoscopic nephrectomy technique
Step 1: Patient positioning and equipment check
The patient is under general anesthesia and positioned in a lateral decubitus position with the side of the kidney to be removed facing upwards.
The surgeon and surgical team will ensure that all the equipment including the laparoscope, camera, trocars, and surgical instruments is properly functioning.
Step 2: Veress needle and trocar placement
A small Veress needle, is inserted into the abdomen to create a pneumoperitoneum a CO2 insufflation that creates space for the laparoscope and instruments.
After the establishment of pneumoperitoneum, a trocar is a hollow tube is introduced through the incision to facilitate and insert the laparoscope. Subsequently, additional trocars are strategically positioned in different areas of abdomen to enable the passage of surgical instruments.
Step 3: Mobilization of the colon
The colon, the large intestine is carefully dissected and moved away from the kidney to expose the renal artery and vein.
Step 4: Identification of the ureter and gonadal vein
The gonadal vein, which drains blood from the testicles or ovaries and the ureter, the kidney’s tube that transports urine to the bladder which is identified & dissected.
Step 5: Renal hilar dissection
The renal hilum serves as the region through which both ureter and blood vessels traverse in their entry and exit from kidney. This is the most critical part of surgery as meticulous dissection is required to identify and isolate the renal artery and vein.
Once the renal artery and vein are isolated they are clipped or tied off with sutures to stop blood flow to the kidney.
Step 6: Remaining renal attachments dissection
The remaining attachments of the kidney such as fatty tissue and ligaments are carefully dissected and divided.
Step 7: Specimen removal
The kidney is then removed through one of the trocar incision sites which may be enlarged if necessary.
Step 8: Closure
The CO2 gas is insufflated from the abdomen and the trocars are removed. The small incision sites are closed with sutures or staples.
Complete Blood Count: This examination offers insights into the number and types of blood cells present including RBC’s, WBC’s, & platelets. Abnormalities in these levels can indicate various conditions that may affect the surgery or the patient’s ability to heal afterward.
BMP and CMP: These panels examine a range of blood components such as blood urea nitrogen, creatinine, glucose, electrolytes, and indicators of renal function. Abnormal levels may indicate kidney dysfunction or other conditions that could affect the surgery.
Coagulation Studies: These tests assess the blood’s ability to clot including PT and aPTT. To reduce the chance of bleeding issues both during and after the procedure it is crucial to assess coagulation status prior to surgery.
Urinalysis: Analysis of urine can provide information about kidney function, urinary tract infections, and other kidney-related conditions. It may include examination of urine sediment, urine pH, protein levels, and the presence of blood or bacteria.
Imaging Studies: Various imaging techniques including ultrasound, CT scans, and MRI may be prescribed to assess both the structure and functionality of the kidneys and adjacent organs. These studies help the surgical team to plan procedure and identify any abnormalities that may affect the surgery.
Bleeding: One possible side effect of surgery is excessive bleeding during or after the procedure.
Infection: There is a chance of infection with any surgical operation. This can occur at the site of incision or internally. Antibiotics are often administered before, during, and after surgery to prevent infection.
Pain: Pain is common after nephrectomy. While pain management strategies are employed some patients may experience significant discomfort in the immediate post-operative period.
Blood clots: Following surgical procedures the individuals may be at risk of developing blood clots in their legs known as deep vein thrombosis (DVT) or experiencing a pulmonary embolism (PE) these clots migrate to the lungs. This risk is particularly heightened when patients remain immobile for prolonged periods post-surgery.
Urinary complications: After nephrectomy, there may be changes in urinary function. These can include urinary retention, urinary tract infections, or incontinence.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



