Background
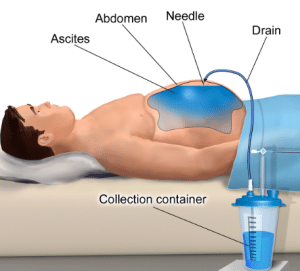
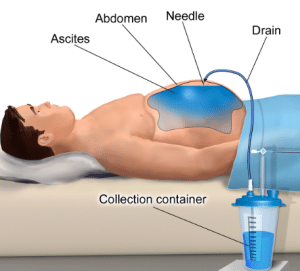
Paracentesis is a medical procedure. It removes excess fluid from the peritoneal cavity of the outer lining of the abdomen organs and abdomen. This fluid is known as ascites. Medical conditions like cirrhosis of the liver, cancer, and heart failure can lead to this. Paracentesis is performed in a clinic or hospital. A needle is inserted in the peritoneal cavity of the abdominal wall, and excess fluid is removed. Paracentesis can give relieve to discomfort and improve the breathing in individuals who have ascites. It is used to diagnose the main cause of the ascites.
Indications
Paracentesis is performed to get rid of the symptoms caused by ascites, like discomfort, abdominal pain, and shortness of breath. The procedure may improve the quality of life of patient by removing excessive fluid. Accumulation of fluid may lead to severe complications like respiratory distress and spontaneous bacterial peritonitis in serious cases. This procedure can prevent these complications by lowering the amount of fluid in the peritoneal cavity.
Paracentesis is common procedure for ascites which occurred by liver cirrhosis. It can lead to scarring and impaired liver function. Ascites can also lead to heart failure. Paracentesis is used to relieve symptoms and improve the breathing patterns in patients who have heart failure-related ascites. It can be also linked with different types of cancer like pancreatic cancer and ovarian cancer. Paracentesis is performed to relieve the symptoms. It is used to remove the infected fluid from the peritoneal cavity in peritonitis cases. This procedure is also used to remove chyle. It is a milky fluid which contains fats from the peritoneal cavity in chyloperitoneum cases.
Contraindications
Severe coagulopathy: Patients who have impaired blood clotting mechanisms or bleeding disorders can be at high risk of bleeding complications during or after the paracentesis procedure.
Uncontrolled infection: Patients who have uncontrolled or active infections in abdominal cavity or nearby tissues can not go for this procedure. It can lead to worse infection or bacteria can go into sterile peritoneal cavity.
Intestinal obstruction: Paracentesis is not suggested in patients who have conformed or suspected intestinal obstruction. This is because the needle insertion may puncture or damage the intestines, which can lead to complications.
Severe abdominal adhesions: Patients who have bands of scar tissue formed after the earlier surgery or infections or extensive abdominal adhesions can be at high risk of needle puncture to abdominal organ during the procedure.
Recent abdominal surgery: Patients who have recent abdominal surgery can need a waiting time before the procedure to heal properly after the surgery to reduce the complications.
Distended bladder: A distended bladder can lead to difficulty to see the peritoneal cavity and elevate the risk of bladder puncture during the procedure. It is suggested to empty the bladder before the procedure begin.
Multiple previous abdominal surgeries: Patients who have a history of multiple abdominal surgeries can have a high risk of the procedure.
Severe organ dysfunction: Patients who have severe kidney or liver dysfunction may have unbalanced fluid and electrolyte abnormality, which need careful consideration before the procedure.
Outcomes
Paracentesis procedure relieve the symptoms like discomfort, abdominal pain, and shortness of beath. Patient may experience immediate effect in the breathing pattern and discomfort. It also helps to prevent the severe complications linked with ascites, like respiratory distress and spontaneous bacterial peritonitis (SBP). It reduced the amount of fluid in peritoneal cavity which can lower the risk of complications.
Paracentesis may improve the quality of life of patient who has ascites. It reduced the symptoms and burden of fluid and engage the patient in the daily activities more effectively and comfortably. Paracentesis can also play an important role to diagnose the main cause of ascites. Analysis of ascites may reveal the presence of inflammation, infection, or cancer cells.
Periprocedural Evaluation
The medical history of patient must be reviewed to determine if there is any factor which can increase the risk of complications from paracentesis like severe heart failure, bleeding disorders, or earlier abdominal surgery.
The current condition of patient must be checked to determine if they are stable to go for the procedure. Patient who has unstable vital sign or severe organ dysfunction may need stabilization before the procedure.
The main cause of ascites must be identified for the proper treatment plan and check for complications. This procedure is not good for patients who have chylous ascites which occurred by a leak of lymphatic fluid into peritoneal cavity.
The patients are prepared by emptying the bladder and remove any clothes which can interfere with the procedure. Ask the patient to position themself in proper and comfort pose on the examination table.
Local anesthesia is used to numb the skin at the puncture area. Sedation can be administrated to lower the discomfort and anxiety in some cases. The needle is inserted in the peritoneal cavity under the guidance of ultrasound to make sure the accurate placement of needle and to avoid any injury to internal organ.
The excessive fluid is removed to prevent complications like electrolyte imbalance or hypotension. The amount of removed fluid is dependent on the condition of patient and severity of ascites.
Monitor the patient closely after the procedure for any signs of complications like infection, bleeding, or hemodynamic instability.
Equipment
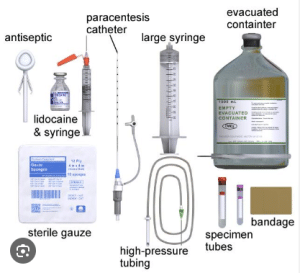
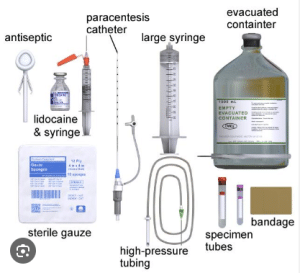
Sterile drapes and towels: These can maintain the sterile areas around the puncture site to reduce the risk of infection.
Local anesthetic: Local anesthetic like lidocaine is used to numb the skin at the puncture area to lower the discomfort and pain.
Paracentesis needle: It is a long and narrow needle with a sharp tip and side opening or trocar. It penetrates the abdominal wall and go to peritoneal cavity.
Three-way stopcock: A three-way stopcock controls the flow of fluid during the procedure. It connects the needle to the drainage bag or syringe and controls the flow rate.
Drainage tubing and bag: It connects the needle and drainage bag and collects the excess fluid from the peritoneal cavity.
Syringes: It is used to aspirate a small amount of fluid to diagnose or to administer local anesthetic.
Antiseptic solution and swabs: They are used to clean the skin at the puncture area to prevent infection.
Gauze pads and dressings: It is used to absorb any fluid which leaks from the puncture area after the procedure.
Technique
Step:1- Before the Procedure
Assessment of patients: The medical history, current condition and main cause of ascites are assessed of patients to determine if the procedure is necessary and to check for potential complications.
Informed Consent: The patient should be informed about the benefits and risks of the procedure and sign the consent form.
Pre-Procedure Preparation: The patient should empty their bladder and remove any clothes or jewelry which can interfere with the procedure. Sedation is also given to lower anxiety and discomfort.
Site Marking: The puncture area is located in the lower quadrant of abdomen which is away from blood vessels and nerves. The area is marked on the skin of the patient.
Step:2 During the Procedure
Skin Preparation: The puncture area is cleaned with an antiseptic solution to lower the risk of infection.
Local Anesthesia: Local anesthetics like lidocaine are administered into the subcutaneous tissue and skin at the puncture area to numb the skin and reduce the pain.

Needle Insertion: A needle is inserted in the peritoneal cavity with the help of ultrasound. This helps to see the cavity and avoid any injury to internal organs.
Fluid Drainage: The three-way stopcock is connected to drainage tube and needle. It is opened and excess fluid is removed slowly into the drainage tube. The flow rate is controlled as per need to prevent any complications like imbalance in electrolyte or hypotension.
Fluid Analysis: A small sample of fluid is sent to the laboratory to know the cause of ascites.
Monitoring: Monitor the patient closely after the procedure for any sign of complications like infection, bleeding, or hemodynamic instability.

Step-3: After the Procedure
Needle Removal: The needle is carefully removed, and puncture area is dressed with bandage.
Post-Procedure Care: The patient is monitored for some time after the procedure to make sure they are stable. They may need any additional fluids or medications as per need.
Follow-Up: Patient must take follow up from the healthcare provider to monitor the condition and assess further need of procedure.
Complications
Pain or discomfort at the puncture area: This is a usual side effect and stays for a few days.
Infection at the puncture site: Infection may occur if the puncture area is not properly cleaned in rare cases.
Hypotension (low blood pressure): Rapid removal of fluid may lead to hypotension which can weaken the function of heart.
Electrolyte imbalance: Sudden fluid removal may alter the levels of electrolyte which need monitoring and correction.
Hemothorax: Puncture of lung may lead to air leak into the surrounding space of lung which can lead to shortness of breathing and chest pain.
Spontaneous bacterial peritonitis (SBP): Bacteria into peritoneal cavity during the procedure may lead to SBP. It is a serious infection condition.
Severe ascites: Patients who have large amounts of ascites are at high risk of complications like imbalance in electrolyte and hypotension.
Medication Summary
Local Anesthetics
Lidocaine: It is a local anesthesia. It is administrated into the skin at the puncture area to numb the skin. It is available in different forms like gels, injections, or patches.
Sedatives
Midazolam: It is a short-acting sedative. It is administrated intravenously. It reduces anxiety and drowsiness.
Propofol: It is a short-acting sedative. It is administrated intravenously. It is more sedative than midazolam and may lead to loss of consciousness.
Analgesics
Acetaminophen: It is a non-steroidal anti-inflammatory drug (NSAID). It relieves the fever and pain. It is available in different forms, like capsules, tablets, and liquids.
Ibuprofen: It is an NSAID. It relieves inflammation and pain. It is available in different forms, like capsules, tablets, and gels.
Electrolyte Repletion
Sodium chloride: It is a solution of sodium and chloride ions. It is used to restore the levels of sodium and chlorine in the blood.
Potassium chloride: It is a solution of potassium and chloride ions. It is used to restore the levels of potassium and chloride in the blood.
Medication

Paracentesis is a medical procedure. It removes excess fluid from the peritoneal cavity of the outer lining of the abdomen organs and abdomen. This fluid is known as ascites. Medical conditions like cirrhosis of the liver, cancer, and heart failure can lead to this. Paracentesis is performed in a clinic or hospital. A needle is inserted in the peritoneal cavity of the abdominal wall, and excess fluid is removed. Paracentesis can give relieve to discomfort and improve the breathing in individuals who have ascites. It is used to diagnose the main cause of the ascites.
Paracentesis is performed to get rid of the symptoms caused by ascites, like discomfort, abdominal pain, and shortness of breath. The procedure may improve the quality of life of patient by removing excessive fluid. Accumulation of fluid may lead to severe complications like respiratory distress and spontaneous bacterial peritonitis in serious cases. This procedure can prevent these complications by lowering the amount of fluid in the peritoneal cavity.
Paracentesis is common procedure for ascites which occurred by liver cirrhosis. It can lead to scarring and impaired liver function. Ascites can also lead to heart failure. Paracentesis is used to relieve symptoms and improve the breathing patterns in patients who have heart failure-related ascites. It can be also linked with different types of cancer like pancreatic cancer and ovarian cancer. Paracentesis is performed to relieve the symptoms. It is used to remove the infected fluid from the peritoneal cavity in peritonitis cases. This procedure is also used to remove chyle. It is a milky fluid which contains fats from the peritoneal cavity in chyloperitoneum cases.
Severe coagulopathy: Patients who have impaired blood clotting mechanisms or bleeding disorders can be at high risk of bleeding complications during or after the paracentesis procedure.
Uncontrolled infection: Patients who have uncontrolled or active infections in abdominal cavity or nearby tissues can not go for this procedure. It can lead to worse infection or bacteria can go into sterile peritoneal cavity.
Intestinal obstruction: Paracentesis is not suggested in patients who have conformed or suspected intestinal obstruction. This is because the needle insertion may puncture or damage the intestines, which can lead to complications.
Severe abdominal adhesions: Patients who have bands of scar tissue formed after the earlier surgery or infections or extensive abdominal adhesions can be at high risk of needle puncture to abdominal organ during the procedure.
Recent abdominal surgery: Patients who have recent abdominal surgery can need a waiting time before the procedure to heal properly after the surgery to reduce the complications.
Distended bladder: A distended bladder can lead to difficulty to see the peritoneal cavity and elevate the risk of bladder puncture during the procedure. It is suggested to empty the bladder before the procedure begin.
Multiple previous abdominal surgeries: Patients who have a history of multiple abdominal surgeries can have a high risk of the procedure.
Severe organ dysfunction: Patients who have severe kidney or liver dysfunction may have unbalanced fluid and electrolyte abnormality, which need careful consideration before the procedure.
Paracentesis procedure relieve the symptoms like discomfort, abdominal pain, and shortness of beath. Patient may experience immediate effect in the breathing pattern and discomfort. It also helps to prevent the severe complications linked with ascites, like respiratory distress and spontaneous bacterial peritonitis (SBP). It reduced the amount of fluid in peritoneal cavity which can lower the risk of complications.
Paracentesis may improve the quality of life of patient who has ascites. It reduced the symptoms and burden of fluid and engage the patient in the daily activities more effectively and comfortably. Paracentesis can also play an important role to diagnose the main cause of ascites. Analysis of ascites may reveal the presence of inflammation, infection, or cancer cells.
The medical history of patient must be reviewed to determine if there is any factor which can increase the risk of complications from paracentesis like severe heart failure, bleeding disorders, or earlier abdominal surgery.
The current condition of patient must be checked to determine if they are stable to go for the procedure. Patient who has unstable vital sign or severe organ dysfunction may need stabilization before the procedure.
The main cause of ascites must be identified for the proper treatment plan and check for complications. This procedure is not good for patients who have chylous ascites which occurred by a leak of lymphatic fluid into peritoneal cavity.
The patients are prepared by emptying the bladder and remove any clothes which can interfere with the procedure. Ask the patient to position themself in proper and comfort pose on the examination table.
Local anesthesia is used to numb the skin at the puncture area. Sedation can be administrated to lower the discomfort and anxiety in some cases. The needle is inserted in the peritoneal cavity under the guidance of ultrasound to make sure the accurate placement of needle and to avoid any injury to internal organ.
The excessive fluid is removed to prevent complications like electrolyte imbalance or hypotension. The amount of removed fluid is dependent on the condition of patient and severity of ascites.
Monitor the patient closely after the procedure for any signs of complications like infection, bleeding, or hemodynamic instability.
Sterile drapes and towels: These can maintain the sterile areas around the puncture site to reduce the risk of infection.
Local anesthetic: Local anesthetic like lidocaine is used to numb the skin at the puncture area to lower the discomfort and pain.
Paracentesis needle: It is a long and narrow needle with a sharp tip and side opening or trocar. It penetrates the abdominal wall and go to peritoneal cavity.
Three-way stopcock: A three-way stopcock controls the flow of fluid during the procedure. It connects the needle to the drainage bag or syringe and controls the flow rate.
Drainage tubing and bag: It connects the needle and drainage bag and collects the excess fluid from the peritoneal cavity.
Syringes: It is used to aspirate a small amount of fluid to diagnose or to administer local anesthetic.
Antiseptic solution and swabs: They are used to clean the skin at the puncture area to prevent infection.
Gauze pads and dressings: It is used to absorb any fluid which leaks from the puncture area after the procedure.
Step:1- Before the Procedure
Assessment of patients: The medical history, current condition and main cause of ascites are assessed of patients to determine if the procedure is necessary and to check for potential complications.
Informed Consent: The patient should be informed about the benefits and risks of the procedure and sign the consent form.
Pre-Procedure Preparation: The patient should empty their bladder and remove any clothes or jewelry which can interfere with the procedure. Sedation is also given to lower anxiety and discomfort.
Site Marking: The puncture area is located in the lower quadrant of abdomen which is away from blood vessels and nerves. The area is marked on the skin of the patient.
Step:2 During the Procedure
Skin Preparation: The puncture area is cleaned with an antiseptic solution to lower the risk of infection.
Local Anesthesia: Local anesthetics like lidocaine are administered into the subcutaneous tissue and skin at the puncture area to numb the skin and reduce the pain.

Needle Insertion: A needle is inserted in the peritoneal cavity with the help of ultrasound. This helps to see the cavity and avoid any injury to internal organs.
Fluid Drainage: The three-way stopcock is connected to drainage tube and needle. It is opened and excess fluid is removed slowly into the drainage tube. The flow rate is controlled as per need to prevent any complications like imbalance in electrolyte or hypotension.
Fluid Analysis: A small sample of fluid is sent to the laboratory to know the cause of ascites.
Monitoring: Monitor the patient closely after the procedure for any sign of complications like infection, bleeding, or hemodynamic instability.

Step-3: After the Procedure
Needle Removal: The needle is carefully removed, and puncture area is dressed with bandage.
Post-Procedure Care: The patient is monitored for some time after the procedure to make sure they are stable. They may need any additional fluids or medications as per need.
Follow-Up: Patient must take follow up from the healthcare provider to monitor the condition and assess further need of procedure.
Pain or discomfort at the puncture area: This is a usual side effect and stays for a few days.
Infection at the puncture site: Infection may occur if the puncture area is not properly cleaned in rare cases.
Hypotension (low blood pressure): Rapid removal of fluid may lead to hypotension which can weaken the function of heart.
Electrolyte imbalance: Sudden fluid removal may alter the levels of electrolyte which need monitoring and correction.
Hemothorax: Puncture of lung may lead to air leak into the surrounding space of lung which can lead to shortness of breathing and chest pain.
Spontaneous bacterial peritonitis (SBP): Bacteria into peritoneal cavity during the procedure may lead to SBP. It is a serious infection condition.
Severe ascites: Patients who have large amounts of ascites are at high risk of complications like imbalance in electrolyte and hypotension.
Local Anesthetics
Lidocaine: It is a local anesthesia. It is administrated into the skin at the puncture area to numb the skin. It is available in different forms like gels, injections, or patches.
Sedatives
Midazolam: It is a short-acting sedative. It is administrated intravenously. It reduces anxiety and drowsiness.
Propofol: It is a short-acting sedative. It is administrated intravenously. It is more sedative than midazolam and may lead to loss of consciousness.
Analgesics
Acetaminophen: It is a non-steroidal anti-inflammatory drug (NSAID). It relieves the fever and pain. It is available in different forms, like capsules, tablets, and liquids.
Ibuprofen: It is an NSAID. It relieves inflammation and pain. It is available in different forms, like capsules, tablets, and gels.
Electrolyte Repletion
Sodium chloride: It is a solution of sodium and chloride ions. It is used to restore the levels of sodium and chlorine in the blood.
Potassium chloride: It is a solution of potassium and chloride ions. It is used to restore the levels of potassium and chloride in the blood.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



