Background
Obstructive Sleep Apnea (OSA) is a type of sleep disorder characterized through recurrent interruptions of the airway during sleep, leading to poor quality sleep and low oxygen levels. It is associated with obesity, increased neck circumference, and certain craniofacial dysmorphism and also leads to cardiovascular diseases, metabolic disorders, and postoperative complications. Patients with OSA are at higher risk during the perioperative period due to risks like airway obstruction, respiratory depression, cardiovascular risks such as hypertension and arrhythmias and increased sensitivity to sedatives and other factors which make them prone to difficulties in intubation, long stay in the recovery period and increased risk of complications.
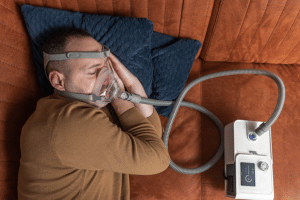
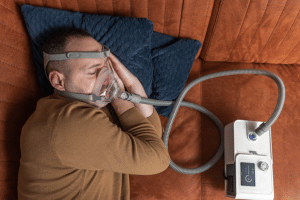
Perioperative management of patients with OSA is complex and requires the input of various healthcare professionals and involves several key approaches. These include initial evaluation by screening instruments to detect OSA, anticipating difficulty in airway management and selecting methods of anaesthesia less likely to cause respiratory compromise. Intra-operative monitoring of oxygenation and ventilation is important especially during surgery. High-risk patients may require continued monitoring in a focused ward while the use of CPAP may require reinstitution immediately after surgery. It is recommended that pain management should use non-opioid analgesics and regional anaesthesia because of the associated respiratory problems.
Indications
Known Diagnosis of OSA: Patient with OSA should undergo certain preoperative evaluation and management to address the risks that come with use of anesthesia and surgery in patients with OSA.
High-Risk Patients: Patients classified as high-risk for OSA by preoperative screening or clinical assessment, even those with an OSA diagnosis only on record but without a final diagnosis, should undergo proper management in the preoperative period.
Surgical Procedures Requiring General Anesthesia: Special patients in need of this therapy are the patients with obstructive sleep apnea, the ones who need general anesthesia, deep sedation or need their airway manipulated.
Use of Opioids or Sedatives: Patients with OSA who undergo surgical procedures during the period where administration of opioids or sedatives is necessary should be managed with considerable precautions regarding respiratory depression, airway obstruction and other related complications.
Complex Airway Management: This is because patients who are anticipated to have difficult airway management because of OSA require special management approaches to ensure safe intubation and ventilation.
Cardiovascular Risk Factors: Some patients with OSA may have appropriate cardiovascular co-morbid conditions like hypertension or arrhythmias and therefore may require extra attention before, during, and after the surgery.
Contraindications
Allergy or Intolerance to CPAP/BiPAP Devices: The list includes any mild, moderate or severe allergies or extremely poor tolerance with these devices.
Inability to Tolerate Non-Supine Positioning: Problems in positioning of screws during surgery.
Severe Respiratory or Cardiac Instability: Circumstances that would make some of these interventions not feasible.
Recent Nasal or Facial Surgery: Safety concerns of using CPAP in surgical patients including recurrent positioning over the surgical sites.
Patient Refusal or Non-Adherence: Noncompliance which comprises rejection of indicated treatments.
Severe Claustrophobia: Comorbidities associated with the failure to use CPAP masks or another device.
Outcomes
Reduced Complications: Enhanced utilisation reduces the likelihood of adverse effects that are experienced in the perioperative period including airway occlusion, respiratory arrest and cardiovascular disorders.
Improved Airway Management: Measures in place help to avoid difficult intubation and ventilation to reduce the rate of incidents.
Enhanced Recovery: Effective handling of OSA in the perioperative period eliminates postoperative respiratory complications and improves general postoperative care making the recovery faster.
Better Pain Control: Conduction of multimodal analgesia and reduced opioids utilization enables achievement of the goal of pain management without compromising respiratory depression.
Decreased Length of Hospital Stay: Patients with controlled OSA may also have less complications and tend to have shorter hospital stays.
Equipment
Patient preparation
Preoperative Assessment: Assess prior medical history, utilize various screening tools also involve the help of sleep specialists if necessary.
Education: Explain to the patient about the necessity of using CPAP/BiPAP and provide them with their devices.
Optimization: Ensure proper settings of the prescription of CPAP/BiPAP device and review the medications.
Anesthesia Planning: When creating a management strategy, a guideline for preventing or reducing risks associated with respiratory depression and for handling airway complications should be included.
Intraoperative Management: It is important to constantly monitor the status of various OSA related equipment’s in the organization and ensure that they are ready for use when the need arises.
Postoperative Care: Resume use of CPAP/BiPAP as soon as possible and observe for respiratory complications.
Instructions: To support this need, home care instructions and emergency contact information need to be clearly stated.
Patient position
Supine Position: Regularly applied during numerous operations, which can make OSA patients’ airway obstructed. The support and the assessment of the airway should also be good.
Head Elevation: However, raising the head of the bed can also potentially decrease airway obstruction and increase ventilation. Patients with OSA may also benefit from the use of this mode particularly if they are having difficulty in maintaining a good signal quality throughout the night.
Lateral Position: Sometimes required in the treatment of acute airway obstruction. It can be helpful, particularly when the patient is at risk of developing airway obstruction if placed in supine position.
Technique
Step 1-Preoperative Assessment: Take a focused history of OSA, including the severity of the condition, treatment such as CPAP usage and the details regarding the therapy, including an update on the patient’s health status. When it comes to identifying OSA suspects or high risk patients the following indicators could be used, some of those include the STOP-BANG questionnaire.
Step 2-Patient Education: Explain to the patient regarding the necessity of compliance with the measures used in OSA treatment like the CPAP/BiPAP devices. The patient should be explained how to use the CPAP/BiPAP equipment and the possible events that may occur during and after the operation.
Step 3-Anesthesia Planning: Build a treatment program to reduce the risk of respiratory depression, and avoid using deep sedation is possible, using regional anesthesia for example. Be ready for the difficulties within airway management and if it’s necessary use video laryngoscopy or some other additional equipment.
Step 4-Intraoperative Management:
Patient Positioning: Ensure that the patient characteristics do not to worsen the airway compromise, use such positions as head up position or lateral position depending on the procedure that is being carried out. Assess and document the patient’s by observing signs such as temperature, blood pressures, pulse oximetry to observe changes in oxygen saturation, and capnography to observe changes in ventilation. Make sure that the required medical equipment such as CPAP/BiPAP machines, airway management devices and others are available and in good working condition.
Step 5-Postoperative Care: Resume use of CPAP/BiPAP therapy as soon as possible after surgery to promote airway opening. If the patient is on the ward, stay with the patient in the recovery area or high-dependency unit and look for the development of complications or respiratory distress.
Step 6-Pain Management: Apartment of pain relief: Minimal use of systemic opioids using multimodal analgesia which involves the integration of non-opioid analgesics and local or regional anesthesia.
Step 7-Patient and Family Instructions: Ensure clients understand home guidance regarding use of the CPAP/BiPAP devices as well as any modifications for recuperation. Provide means through which they can be followed up and instructions on what should be done any time there are complications.
Perioperative-management-of-obstructive-sleep-apnea
Approach considerations
Risk Assessment: There is the stop bang criteria for determining possible OSA risk and examining other conditions. Evaluate OSA severity and currently used DPAP effectiveness, as well as CPAP parameters.
Anesthesia Management: Create a strategy aimed at reducing the risks for the patient in relation to respiratory malfunction with a preference given to regional anesthesia and combined pain management protocols. It is advisable to be ready for episodes that are related to airway management.
Intraoperative Monitoring: The pulse oximetry and capnography should be assessed on an on-going basis to determine oxygenation and ventilation requirements. Bring the patient to the correct position to ensure the airway is open.
Pain Management: Minimise opioid exposure and the consequent risk of respiratory depression by adopting multimodal analgesia. This means adequate pain relief should be achieved but at the same time the patient should not be over sedated.
Complications

Obstructive Sleep Apnea (OSA) is a type of sleep disorder characterized through recurrent interruptions of the airway during sleep, leading to poor quality sleep and low oxygen levels. It is associated with obesity, increased neck circumference, and certain craniofacial dysmorphism and also leads to cardiovascular diseases, metabolic disorders, and postoperative complications. Patients with OSA are at higher risk during the perioperative period due to risks like airway obstruction, respiratory depression, cardiovascular risks such as hypertension and arrhythmias and increased sensitivity to sedatives and other factors which make them prone to difficulties in intubation, long stay in the recovery period and increased risk of complications.
Perioperative management of patients with OSA is complex and requires the input of various healthcare professionals and involves several key approaches. These include initial evaluation by screening instruments to detect OSA, anticipating difficulty in airway management and selecting methods of anaesthesia less likely to cause respiratory compromise. Intra-operative monitoring of oxygenation and ventilation is important especially during surgery. High-risk patients may require continued monitoring in a focused ward while the use of CPAP may require reinstitution immediately after surgery. It is recommended that pain management should use non-opioid analgesics and regional anaesthesia because of the associated respiratory problems.
Known Diagnosis of OSA: Patient with OSA should undergo certain preoperative evaluation and management to address the risks that come with use of anesthesia and surgery in patients with OSA.
High-Risk Patients: Patients classified as high-risk for OSA by preoperative screening or clinical assessment, even those with an OSA diagnosis only on record but without a final diagnosis, should undergo proper management in the preoperative period.
Surgical Procedures Requiring General Anesthesia: Special patients in need of this therapy are the patients with obstructive sleep apnea, the ones who need general anesthesia, deep sedation or need their airway manipulated.
Use of Opioids or Sedatives: Patients with OSA who undergo surgical procedures during the period where administration of opioids or sedatives is necessary should be managed with considerable precautions regarding respiratory depression, airway obstruction and other related complications.
Complex Airway Management: This is because patients who are anticipated to have difficult airway management because of OSA require special management approaches to ensure safe intubation and ventilation.
Cardiovascular Risk Factors: Some patients with OSA may have appropriate cardiovascular co-morbid conditions like hypertension or arrhythmias and therefore may require extra attention before, during, and after the surgery.
Allergy or Intolerance to CPAP/BiPAP Devices: The list includes any mild, moderate or severe allergies or extremely poor tolerance with these devices.
Inability to Tolerate Non-Supine Positioning: Problems in positioning of screws during surgery.
Severe Respiratory or Cardiac Instability: Circumstances that would make some of these interventions not feasible.
Recent Nasal or Facial Surgery: Safety concerns of using CPAP in surgical patients including recurrent positioning over the surgical sites.
Patient Refusal or Non-Adherence: Noncompliance which comprises rejection of indicated treatments.
Severe Claustrophobia: Comorbidities associated with the failure to use CPAP masks or another device.
Reduced Complications: Enhanced utilisation reduces the likelihood of adverse effects that are experienced in the perioperative period including airway occlusion, respiratory arrest and cardiovascular disorders.
Improved Airway Management: Measures in place help to avoid difficult intubation and ventilation to reduce the rate of incidents.
Enhanced Recovery: Effective handling of OSA in the perioperative period eliminates postoperative respiratory complications and improves general postoperative care making the recovery faster.
Better Pain Control: Conduction of multimodal analgesia and reduced opioids utilization enables achievement of the goal of pain management without compromising respiratory depression.
Decreased Length of Hospital Stay: Patients with controlled OSA may also have less complications and tend to have shorter hospital stays.
Preoperative Assessment: Assess prior medical history, utilize various screening tools also involve the help of sleep specialists if necessary.
Education: Explain to the patient about the necessity of using CPAP/BiPAP and provide them with their devices.
Optimization: Ensure proper settings of the prescription of CPAP/BiPAP device and review the medications.
Anesthesia Planning: When creating a management strategy, a guideline for preventing or reducing risks associated with respiratory depression and for handling airway complications should be included.
Intraoperative Management: It is important to constantly monitor the status of various OSA related equipment’s in the organization and ensure that they are ready for use when the need arises.
Postoperative Care: Resume use of CPAP/BiPAP as soon as possible and observe for respiratory complications.
Instructions: To support this need, home care instructions and emergency contact information need to be clearly stated.
Supine Position: Regularly applied during numerous operations, which can make OSA patients’ airway obstructed. The support and the assessment of the airway should also be good.
Head Elevation: However, raising the head of the bed can also potentially decrease airway obstruction and increase ventilation. Patients with OSA may also benefit from the use of this mode particularly if they are having difficulty in maintaining a good signal quality throughout the night.
Lateral Position: Sometimes required in the treatment of acute airway obstruction. It can be helpful, particularly when the patient is at risk of developing airway obstruction if placed in supine position.
Step 1-Preoperative Assessment: Take a focused history of OSA, including the severity of the condition, treatment such as CPAP usage and the details regarding the therapy, including an update on the patient’s health status. When it comes to identifying OSA suspects or high risk patients the following indicators could be used, some of those include the STOP-BANG questionnaire.
Step 2-Patient Education: Explain to the patient regarding the necessity of compliance with the measures used in OSA treatment like the CPAP/BiPAP devices. The patient should be explained how to use the CPAP/BiPAP equipment and the possible events that may occur during and after the operation.
Step 3-Anesthesia Planning: Build a treatment program to reduce the risk of respiratory depression, and avoid using deep sedation is possible, using regional anesthesia for example. Be ready for the difficulties within airway management and if it’s necessary use video laryngoscopy or some other additional equipment.
Step 4-Intraoperative Management:
Patient Positioning: Ensure that the patient characteristics do not to worsen the airway compromise, use such positions as head up position or lateral position depending on the procedure that is being carried out. Assess and document the patient’s by observing signs such as temperature, blood pressures, pulse oximetry to observe changes in oxygen saturation, and capnography to observe changes in ventilation. Make sure that the required medical equipment such as CPAP/BiPAP machines, airway management devices and others are available and in good working condition.
Step 5-Postoperative Care: Resume use of CPAP/BiPAP therapy as soon as possible after surgery to promote airway opening. If the patient is on the ward, stay with the patient in the recovery area or high-dependency unit and look for the development of complications or respiratory distress.
Step 6-Pain Management: Apartment of pain relief: Minimal use of systemic opioids using multimodal analgesia which involves the integration of non-opioid analgesics and local or regional anesthesia.
Step 7-Patient and Family Instructions: Ensure clients understand home guidance regarding use of the CPAP/BiPAP devices as well as any modifications for recuperation. Provide means through which they can be followed up and instructions on what should be done any time there are complications.
Perioperative-management-of-obstructive-sleep-apnea
Risk Assessment: There is the stop bang criteria for determining possible OSA risk and examining other conditions. Evaluate OSA severity and currently used DPAP effectiveness, as well as CPAP parameters.
Anesthesia Management: Create a strategy aimed at reducing the risks for the patient in relation to respiratory malfunction with a preference given to regional anesthesia and combined pain management protocols. It is advisable to be ready for episodes that are related to airway management.
Intraoperative Monitoring: The pulse oximetry and capnography should be assessed on an on-going basis to determine oxygenation and ventilation requirements. Bring the patient to the correct position to ensure the airway is open.
Pain Management: Minimise opioid exposure and the consequent risk of respiratory depression by adopting multimodal analgesia. This means adequate pain relief should be achieved but at the same time the patient should not be over sedated.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



