Background
Polypectomy is the surgical removal of polyps which are benign growths of tissues that may arise in many locations; however, they are frequently found in the colon, stomach, uterus, or nasal passages. Polyps are mostly benign or non-cancerous growths; however certain types of polyps are seen in the colon, and these may well turn malignant if not removed at the right time. Surgical polypectomy may be diagnostic or therapeutic depending on the fact whether the polyp was removed for relief of symptoms, to prevent further development of the disease, or for histopathological examination.
Polypectomy
Indications
Adenomatous Polyps: Adenomas are benign tumors that have a likelihood of turning malignant and transforming into colorectal cancer. Its removal decreases the probability of advancement.
Sessile Serrated Polyps: These have the ability to become malignant especially where they are bigger than 10mm or exhibit dysplasia.
Hyperplastic Polyps: Usually non-missile lesions; however, those that involve lesions greater than 10 mm in size in the proximal colon may be removed given a slight increase in cancer risk.
Bleeding Polyps: The following can be managed by removal since polyps are said to cause rectal bleeding, if symptomatic.
Obstructive Polyps: Large polyps, particularly those arising from the colon or small bowel may precipitate symptoms such as pain, cramps, and or bowel obstruction.
Contraindications
Active Colitis or Infection: Mild inflammation of a patient’s large intestine due to Crohn’s disease or ulcerative colitis can elevate chances of perforation and bleeding.
Coagulopathy or Uncontrolled Bleeding Disorders: Those patients who have coagulation disorders or thrombocytopenia and those who use anticoagulant medications may experience post-procedure bleeding.
Poor General Health or Comorbidities: Contraindications to a polypectomy include patients with uncontrolled heart diseases, severe pulmonary diseases, or other diseases that may make the anesthesia of the procedure dangerous.
Outcomes
Periprocedural care
Equipment
Polypectomy Snares
Cold Snares
Hot Snares
Electrosurgical Unit (ESU)
Injection Needles
Hemostatic Clips
Endoscopic Loop Devices
Baskets and Retrieval Nets
Endoscope with Channels
Patient preparation
Medical Evaluation
Medical History Review: Ask about case history of bleeding disorders, any history of allergy, present medications, and general health status. Medication Adjustments: Medications such as aspirin, warfarin, or NSAIDs that affect blood clotting might be held as a precaution against bleeding.
Pre-procedure Testing: Some patients may require microscopic analysis, for example, coagulation tests or blood tests to determine coagulation parameters and kidney function, respectively.
Dietary Restrictions
Clear Liquid Diet: More often, the day before the procedure, the patient may be required to follow a clear liquid diet.
Preoperative Management (In Preparation for Colon Polypectomy) Laxative Solution: It is then expected that a patient takes a prescribed laxative solution the morning of the procedure. This helps to empty the colon of contents making it easier to visualize the polyps.
Patient position
Left Lateral Decubitus: The patient lies on their left side with knees flexed to some extent. This position is typical of most colonoscopy cases because it allows easy bowel visibility especially if it is only the rectum and lower colon that must be examined.
Supine Position: Used sometimes if there is a desire for better visualization in different areas of the colon, for example with polyps in the ascending colon.
Patient Preparation
Bowel Preparation: The patient needs to be prepared for colonoscopy by taking a bowel wash that clears the colon. This is achieved through intermittent fasting or being on a clear liquid diet and the intake of prescription laxatives like polyethylene glycol.
Medication Review: Patients should disclose to their surgeon if they have such other medications as anticoagulant or antiplatelet because these may require alteration before the procedure.
Anesthesia: Sedation is usually given to make the patient relaxed all through the procedure.
Procedure
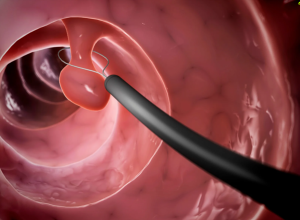
Insertion of the Colonoscope: Endoscopy involves a colonoscope, a long, thin, flexible endoscopic tube with a focal camera and light at the tip.
The doctor carries out a visual inspection of the lining of the colon for polyps or other characteristics that may be causing bleeding.
Identification of Polyps: Polyps are classified according to their morphological appearances, that is shape, size, and color.
They can be classified into several types:
Adenomatous Polyps: These can grow into cancer. Hyperplastic Polyps: Generally benign and not associated with cancer.
Serrated Polyps: Some are benign while others can be precursors to cancer.
Polypectomy Techniques
Snare Polypectomy: A snare (a wire loop) is used to loop around the base of the polyp.
The snare is tightened, and that tool can be used with electrocautery to remove the base of the polyp completely.
This method is applicable for bigger-sized polyps normally a size measure of greater than 1 cm.
Cold Forceps Polypectomy: Polyps of dimensions less than 5mm can be removed using a forceps method without the application of electric current.
With the help of forceps, the polyp is taken and then excised. Endoscopic Mucosal Resection (EMR):
EMR might be used for larger or more complex polyps in either technique, loops of the colon are mobilized and withdrawn through a small incision. It entails injecting a solution within the area of tissue underlying the polyp up to the time it is lifted and then snared. Endoscopic Submucosal Dissection (ESD): Larger tumor lesions, that necessitate broader invasion of tissue planes. The submucosa is then carefully separated removes the polyp en bloc.
Step 4-Specimen Collection: Polyps removed during the procedure end up being submitted to histopathological analysis to check on whether they are malignant or benign.
Step 5-Hemostasis: After polypectomy, the site is assessed for bleeding. If bleeding occurs, it can be managed with various techniques, including:
Thermal coagulation.
Hemoclips.
Argon plasma coagulation.
Step 6-Post-Procedure Care Recovery: Most patients may be observed in a specific recovery area for some time as the effect of the sedation wears off.
Post-Procedure Instructions: As for after treatment, the patients are restricted from such activities as intense movements for one or two days.
Clear liquid diets are prescribed in many cases.
Follow-Up: A routine colonoscopy may be advised depending on the number and nature of the polyps and the patient’s family history of Colorectal cancer.
Complications
Bleeding: Such can be observed during or soon after the procedure.
Delayed bleeding: This may occur up to two weeks post-procedure most specifically in the colon.
Perforation: This happens when a hole is created while operating on an organ, for instance, the colon, to remove polyps.
Risk factors: Large-sized polyps or complicated procedures or if the tissues are also weak in recovering chances are that there might be increased risks.
Infection: Though rare, infections can develop at the polyp removal site.
Post-polypectomy Syndrome
This happens when the tissue heals in a perforation-like way with symptoms of fever, pain, and tenderness but does not have a perforation.
Adverse Reactions to Anesthesia
In cases of sedation, side effects or reactions to anesthesia can occur in patients.

Polypectomy is the surgical removal of polyps which are benign growths of tissues that may arise in many locations; however, they are frequently found in the colon, stomach, uterus, or nasal passages. Polyps are mostly benign or non-cancerous growths; however certain types of polyps are seen in the colon, and these may well turn malignant if not removed at the right time. Surgical polypectomy may be diagnostic or therapeutic depending on the fact whether the polyp was removed for relief of symptoms, to prevent further development of the disease, or for histopathological examination.
Polypectomy
Adenomatous Polyps: Adenomas are benign tumors that have a likelihood of turning malignant and transforming into colorectal cancer. Its removal decreases the probability of advancement.
Sessile Serrated Polyps: These have the ability to become malignant especially where they are bigger than 10mm or exhibit dysplasia.
Hyperplastic Polyps: Usually non-missile lesions; however, those that involve lesions greater than 10 mm in size in the proximal colon may be removed given a slight increase in cancer risk.
Bleeding Polyps: The following can be managed by removal since polyps are said to cause rectal bleeding, if symptomatic.
Obstructive Polyps: Large polyps, particularly those arising from the colon or small bowel may precipitate symptoms such as pain, cramps, and or bowel obstruction.
Active Colitis or Infection: Mild inflammation of a patient’s large intestine due to Crohn’s disease or ulcerative colitis can elevate chances of perforation and bleeding.
Coagulopathy or Uncontrolled Bleeding Disorders: Those patients who have coagulation disorders or thrombocytopenia and those who use anticoagulant medications may experience post-procedure bleeding.
Poor General Health or Comorbidities: Contraindications to a polypectomy include patients with uncontrolled heart diseases, severe pulmonary diseases, or other diseases that may make the anesthesia of the procedure dangerous.
Equipment
Polypectomy Snares
Cold Snares
Hot Snares
Electrosurgical Unit (ESU)
Injection Needles
Hemostatic Clips
Endoscopic Loop Devices
Baskets and Retrieval Nets
Endoscope with Channels
Patient preparation
Medical Evaluation
Medical History Review: Ask about case history of bleeding disorders, any history of allergy, present medications, and general health status. Medication Adjustments: Medications such as aspirin, warfarin, or NSAIDs that affect blood clotting might be held as a precaution against bleeding.
Pre-procedure Testing: Some patients may require microscopic analysis, for example, coagulation tests or blood tests to determine coagulation parameters and kidney function, respectively.
Dietary Restrictions
Clear Liquid Diet: More often, the day before the procedure, the patient may be required to follow a clear liquid diet.
Preoperative Management (In Preparation for Colon Polypectomy) Laxative Solution: It is then expected that a patient takes a prescribed laxative solution the morning of the procedure. This helps to empty the colon of contents making it easier to visualize the polyps.
Patient position
Left Lateral Decubitus: The patient lies on their left side with knees flexed to some extent. This position is typical of most colonoscopy cases because it allows easy bowel visibility especially if it is only the rectum and lower colon that must be examined.
Supine Position: Used sometimes if there is a desire for better visualization in different areas of the colon, for example with polyps in the ascending colon.
Bowel Preparation: The patient needs to be prepared for colonoscopy by taking a bowel wash that clears the colon. This is achieved through intermittent fasting or being on a clear liquid diet and the intake of prescription laxatives like polyethylene glycol.
Medication Review: Patients should disclose to their surgeon if they have such other medications as anticoagulant or antiplatelet because these may require alteration before the procedure.
Anesthesia: Sedation is usually given to make the patient relaxed all through the procedure.
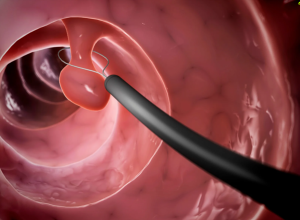
Insertion of the Colonoscope: Endoscopy involves a colonoscope, a long, thin, flexible endoscopic tube with a focal camera and light at the tip.
The doctor carries out a visual inspection of the lining of the colon for polyps or other characteristics that may be causing bleeding.
Identification of Polyps: Polyps are classified according to their morphological appearances, that is shape, size, and color.
They can be classified into several types:
Adenomatous Polyps: These can grow into cancer. Hyperplastic Polyps: Generally benign and not associated with cancer.
Serrated Polyps: Some are benign while others can be precursors to cancer.
Snare Polypectomy: A snare (a wire loop) is used to loop around the base of the polyp.
The snare is tightened, and that tool can be used with electrocautery to remove the base of the polyp completely.
This method is applicable for bigger-sized polyps normally a size measure of greater than 1 cm.
Cold Forceps Polypectomy: Polyps of dimensions less than 5mm can be removed using a forceps method without the application of electric current.
With the help of forceps, the polyp is taken and then excised. Endoscopic Mucosal Resection (EMR):
EMR might be used for larger or more complex polyps in either technique, loops of the colon are mobilized and withdrawn through a small incision. It entails injecting a solution within the area of tissue underlying the polyp up to the time it is lifted and then snared. Endoscopic Submucosal Dissection (ESD): Larger tumor lesions, that necessitate broader invasion of tissue planes. The submucosa is then carefully separated removes the polyp en bloc.
Step 4-Specimen Collection: Polyps removed during the procedure end up being submitted to histopathological analysis to check on whether they are malignant or benign.
Step 5-Hemostasis: After polypectomy, the site is assessed for bleeding. If bleeding occurs, it can be managed with various techniques, including:
Thermal coagulation.
Hemoclips.
Argon plasma coagulation.
Step 6-Post-Procedure Care Recovery: Most patients may be observed in a specific recovery area for some time as the effect of the sedation wears off.
Post-Procedure Instructions: As for after treatment, the patients are restricted from such activities as intense movements for one or two days.
Clear liquid diets are prescribed in many cases.
Follow-Up: A routine colonoscopy may be advised depending on the number and nature of the polyps and the patient’s family history of Colorectal cancer.
Complications
Bleeding: Such can be observed during or soon after the procedure.
Delayed bleeding: This may occur up to two weeks post-procedure most specifically in the colon.
Perforation: This happens when a hole is created while operating on an organ, for instance, the colon, to remove polyps.
Risk factors: Large-sized polyps or complicated procedures or if the tissues are also weak in recovering chances are that there might be increased risks.
Infection: Though rare, infections can develop at the polyp removal site.
Post-polypectomy Syndrome
This happens when the tissue heals in a perforation-like way with symptoms of fever, pain, and tenderness but does not have a perforation.
Adverse Reactions to Anesthesia
In cases of sedation, side effects or reactions to anesthesia can occur in patients.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



