Background
A pyloroplasty is a surgical procedure that consists of either widening or reconstruction of the pylorus, whose role is to serve as the muscular valve for the passage of food from the stomach to the small intestine. Most often, the pylorus becomes infected and, as a result, may become either narrowed or obstruction. This may occur due to several diseases, including peptic ulcers, inflammation, or scarring, which leads to such symptoms as nausea, vomiting, and abdominal pain. The process of decreasing the pyloric contraction is used during the pyloroplasty surgery. In this way, the patient’s condition is improved.
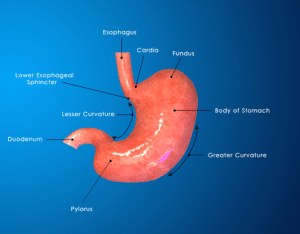
Anatomy of stomach
The practice of pyloroplasty dates back as early as the start of the 20th century when surgeons were the first to introduce surgical interventions to address the other side of pyloric stenosis, narrowing the pylorus. In 1912, the first-ever pyloroplasty was conducted successfully in the United States by the American surgeon Conrad Ramstedt. He developed a surgical methodology that served the purpose of resolving congenital pyloric stenosis in infants.
Indications
Pyloric Stenosis: Pyloroplasty is primarily done to deal with pyloric stenosis, a condition characterized by the abnormal reduction of diameter of the pylorus, therefore leading to the block of gastric outlet.
Peptic Ulcers: Pyloroplasty will be given as a treatment option when patients with peptic ulcers have caused scarring or inflammation of the pylorus that leads to stenosis or obstruction.
Gastric Outlet Obstruction: A pyloroplasty approach is used if there is a gastric outlet obstruction where the movement of food from the stomach to the small intestine is blocked or impaired.
Pyloric Strictures: Pyloroplasty can be used in cases with pyloric strictures that may be result of scarring or inflammation which makes the passage of food from stomach narrow.
Gastric Dysmotility: In the case of patients with gastric dysfunction caused by gastroparesis, pyloroplasty can be a viable option as the condition is characterized by the slow or lack of normal food movement through the stomach.
Contraindications
Active Gastric or Duodenal Ulcers: It is a case when pyloroplasty is unadvised in presence of active gastric or duodenal ulcers because the exceeding risk of ulceration or bleedings may be the adverse effect of the procedure.
Bleeding Disorders: Those who are suffering from bleeding disorders or who are taking drugs counteracting the process can face the risk of bleeding during the pyloroplasty.
Previous Gastric Surgery: The previous surgery gastric patients may face some issues during the procedure, making pyloroplasty will be technically challenging or less effective.
Outcomes
Equipment
Patient preparation
Preoperative Evaluation: Preoperative evaluation of the patient by the physician is the first step in the pyloroplasty procedure.
Informed Consent: The patient meets for a preoperative consultation with his surgeon to get a clear idea about every aspect of pyloroplasty such as the risk-benefit ratio and alternative modes of treatment.
Medication Management: The patient’s medications are reviewed; hence, the ones that can interfere with the surgery or anesthesia are identified.
Final Preoperative Assessment: Prior to the start of the surgery, the surgical team performs a check-up on the patient which ensures that the necessary preparations are in place, and the details of the surgery plan have been finalized.
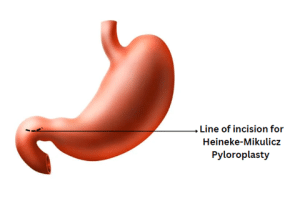
Heineke-Mikulicz Pyloroplasty
Heineke-Mikulicz pyloroplasty is a surgical method for treating the spasm of the pylorus or gastric outlet obstruction by widening the pyloric opening.
Step:1 – Patient positioning: The patient is lying under the general anesthesia on supine position, on the operating table.
Step:2 – Surgical Incision: Generally, a midline or transverse abdominal incision is made, depending on the surgeon’s choice, the patient’s anatomy, and the complexity of the surgery.
Step:3 – Pylorus showing: The stomach and pyloric region are properly exposed using retractors to view the pylorus.
Step:4 – Identification of Pylorus: At that point, there is a transition between the stomach and duodenum, which can be used as a landmark to spot the pyloric region.
Step:5 – Incision in the Pyloric Muscle: This incision is made longitudinally on the pyloric muscle in the pylorus anterior surface. An incision is performed to an appropriate size to assure that the dilatation of the pylorus opening is adequate.
Step:6 – Dilating Pyloric Orifice: The foreps are now used to hold the extremities of the longitudinal incision and by pulling them apart the pylorus is dilated.
Step:7 – The completed pyloric epithelization is finally closed with absorbable sutures transversely.
Step:8 – Abdominal incision closure: Once the pyloroplasty is complete, the abdominal incision is closed using absorbable sutures or staples passed in layers.
Step:9 – Post operative stage: The patient is shifted to the recovery room for monitoring. Pain management, postoperative care and instructions are being provided.
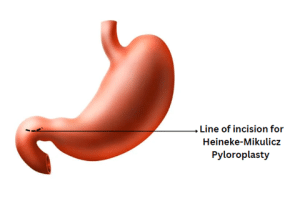
Heineke-Mikulicz Pyloroplasty
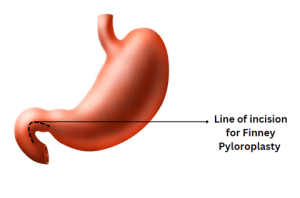
Finney Pyloroplasty
The Finney pyloroplasty is a surgical technique where pyloric sphincter is widened to allow unimpeded passage of the chyme. The procedure is named after surgeon Harvey Cushing,
A longitudinal cut on the pyloric muscle and transverse suturing it enlarges the pylorus. This procedural measure helps reestablish regular gastric emptying and release symptoms usually associated with gastric outlet (pyloric) obstruction.
The Finney pyloroplasty technique is performed with the patient under general anesthesia, and the abdomen is cleaned and draped first in a sterile manner. To accessing the pylorus, the surgeon will usually make a midline or transverse abdominal incision and identify the pyloric region. An incision along the pyloric muscle is then a longitudinal one, and the edges of the opening are then sutured in a transverse direction to increase the pyloric opening size. The incision is sutured up, and then the abdomen is closed in a layer-by-layer fashion.
Surgery is followed by postoperative observation in case of any complications. The treatment for pain and prescription instructions for postoperative care are provided, and the patients are gradually stepped onto a regular diet as they can be able to tolerate it.
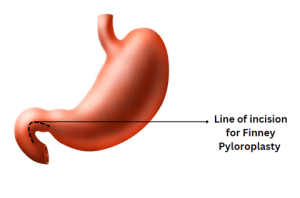
Finney Pyloroplasty
Pyloromyotomy (Ramstedt)
Pyloromyotomy or Ramstedt pyloromyotomy is a surgery for infantile hypertrophic pyloric stenosis (IHPS) by cutting the thickened muscle of the pylorus, which is the narrow part of the stomach that eases the food to enter the intestine. This procedure is named after the Swedish surgeon Harald Hirschsprung. It describes the technique: the longitudinal incision of the pyloric muscle is done, then it is sutured transversely to widen the pylorus. This method restores the normal emptying process and relieves the symptoms related to the disturbance of the gastric outlet obstruction.
A general anesthesia is induced in the infant that allows to conduct a small incision in the abdomen, providing an access to the pylorus. Transverse stitches are performed at the longitudinal pylorus muscle, after which the edges of the incision are sutured transversely. The incision is secured with sutures, and the abdomen is closed with layers of sutures.
Complications
Bleeding: Pyloroplasty involves the creation of incision to the pyloric muscle that could cause bleeding to occur either before or after the procedure. A minor bleeding may be stopped by adding pressure or cauterizing, but severe hemorrhage might still need further surgical treatment.
Wound Dehiscence: In certain cases, the incision that is made during the procedure can separate and relocate. This can lead to a long-term recovery process and may cause an increased chance of a secondary infection.
Dumping Syndrome: Rarely, a patient may develop symptoms of dumping syndrome because of pyloroplasty. The dumping syndrome is characterized by early and rapid emptying of stomach contents into the small bowel. Patients may experience abdominal cramping, diarrhea, sweating and light-headedness as their major symptoms.
Pyloric Stenosis Recurrence: Although the complete elimination of the recurrent pyloric stenosis is possible, the risk remains, especially for the cases after treatment with pyloromyotomy in IHPS.
Gastroesophageal Reflux: Pyloroplasty could be the reason for the esophagus reflux in particular patients and the symptoms they face including regurgitation, heartburn, and chest pain.
References

A pyloroplasty is a surgical procedure that consists of either widening or reconstruction of the pylorus, whose role is to serve as the muscular valve for the passage of food from the stomach to the small intestine. Most often, the pylorus becomes infected and, as a result, may become either narrowed or obstruction. This may occur due to several diseases, including peptic ulcers, inflammation, or scarring, which leads to such symptoms as nausea, vomiting, and abdominal pain. The process of decreasing the pyloric contraction is used during the pyloroplasty surgery. In this way, the patient’s condition is improved.
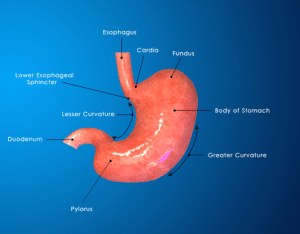
Anatomy of stomach
The practice of pyloroplasty dates back as early as the start of the 20th century when surgeons were the first to introduce surgical interventions to address the other side of pyloric stenosis, narrowing the pylorus. In 1912, the first-ever pyloroplasty was conducted successfully in the United States by the American surgeon Conrad Ramstedt. He developed a surgical methodology that served the purpose of resolving congenital pyloric stenosis in infants.
Pyloric Stenosis: Pyloroplasty is primarily done to deal with pyloric stenosis, a condition characterized by the abnormal reduction of diameter of the pylorus, therefore leading to the block of gastric outlet.
Peptic Ulcers: Pyloroplasty will be given as a treatment option when patients with peptic ulcers have caused scarring or inflammation of the pylorus that leads to stenosis or obstruction.
Gastric Outlet Obstruction: A pyloroplasty approach is used if there is a gastric outlet obstruction where the movement of food from the stomach to the small intestine is blocked or impaired.
Pyloric Strictures: Pyloroplasty can be used in cases with pyloric strictures that may be result of scarring or inflammation which makes the passage of food from stomach narrow.
Gastric Dysmotility: In the case of patients with gastric dysfunction caused by gastroparesis, pyloroplasty can be a viable option as the condition is characterized by the slow or lack of normal food movement through the stomach.
Active Gastric or Duodenal Ulcers: It is a case when pyloroplasty is unadvised in presence of active gastric or duodenal ulcers because the exceeding risk of ulceration or bleedings may be the adverse effect of the procedure.
Bleeding Disorders: Those who are suffering from bleeding disorders or who are taking drugs counteracting the process can face the risk of bleeding during the pyloroplasty.
Previous Gastric Surgery: The previous surgery gastric patients may face some issues during the procedure, making pyloroplasty will be technically challenging or less effective.
Preoperative Evaluation: Preoperative evaluation of the patient by the physician is the first step in the pyloroplasty procedure.
Informed Consent: The patient meets for a preoperative consultation with his surgeon to get a clear idea about every aspect of pyloroplasty such as the risk-benefit ratio and alternative modes of treatment.
Medication Management: The patient’s medications are reviewed; hence, the ones that can interfere with the surgery or anesthesia are identified.
Final Preoperative Assessment: Prior to the start of the surgery, the surgical team performs a check-up on the patient which ensures that the necessary preparations are in place, and the details of the surgery plan have been finalized.
Heineke-Mikulicz pyloroplasty is a surgical method for treating the spasm of the pylorus or gastric outlet obstruction by widening the pyloric opening.
Step:1 – Patient positioning: The patient is lying under the general anesthesia on supine position, on the operating table.
Step:2 – Surgical Incision: Generally, a midline or transverse abdominal incision is made, depending on the surgeon’s choice, the patient’s anatomy, and the complexity of the surgery.
Step:3 – Pylorus showing: The stomach and pyloric region are properly exposed using retractors to view the pylorus.
Step:4 – Identification of Pylorus: At that point, there is a transition between the stomach and duodenum, which can be used as a landmark to spot the pyloric region.
Step:5 – Incision in the Pyloric Muscle: This incision is made longitudinally on the pyloric muscle in the pylorus anterior surface. An incision is performed to an appropriate size to assure that the dilatation of the pylorus opening is adequate.
Step:6 – Dilating Pyloric Orifice: The foreps are now used to hold the extremities of the longitudinal incision and by pulling them apart the pylorus is dilated.
Step:7 – The completed pyloric epithelization is finally closed with absorbable sutures transversely.
Step:8 – Abdominal incision closure: Once the pyloroplasty is complete, the abdominal incision is closed using absorbable sutures or staples passed in layers.
Step:9 – Post operative stage: The patient is shifted to the recovery room for monitoring. Pain management, postoperative care and instructions are being provided.
Heineke-Mikulicz Pyloroplasty
The Finney pyloroplasty is a surgical technique where pyloric sphincter is widened to allow unimpeded passage of the chyme. The procedure is named after surgeon Harvey Cushing,
A longitudinal cut on the pyloric muscle and transverse suturing it enlarges the pylorus. This procedural measure helps reestablish regular gastric emptying and release symptoms usually associated with gastric outlet (pyloric) obstruction.
The Finney pyloroplasty technique is performed with the patient under general anesthesia, and the abdomen is cleaned and draped first in a sterile manner. To accessing the pylorus, the surgeon will usually make a midline or transverse abdominal incision and identify the pyloric region. An incision along the pyloric muscle is then a longitudinal one, and the edges of the opening are then sutured in a transverse direction to increase the pyloric opening size. The incision is sutured up, and then the abdomen is closed in a layer-by-layer fashion.
Surgery is followed by postoperative observation in case of any complications. The treatment for pain and prescription instructions for postoperative care are provided, and the patients are gradually stepped onto a regular diet as they can be able to tolerate it.
Finney Pyloroplasty
Pyloromyotomy or Ramstedt pyloromyotomy is a surgery for infantile hypertrophic pyloric stenosis (IHPS) by cutting the thickened muscle of the pylorus, which is the narrow part of the stomach that eases the food to enter the intestine. This procedure is named after the Swedish surgeon Harald Hirschsprung. It describes the technique: the longitudinal incision of the pyloric muscle is done, then it is sutured transversely to widen the pylorus. This method restores the normal emptying process and relieves the symptoms related to the disturbance of the gastric outlet obstruction.
A general anesthesia is induced in the infant that allows to conduct a small incision in the abdomen, providing an access to the pylorus. Transverse stitches are performed at the longitudinal pylorus muscle, after which the edges of the incision are sutured transversely. The incision is secured with sutures, and the abdomen is closed with layers of sutures.
Bleeding: Pyloroplasty involves the creation of incision to the pyloric muscle that could cause bleeding to occur either before or after the procedure. A minor bleeding may be stopped by adding pressure or cauterizing, but severe hemorrhage might still need further surgical treatment.
Wound Dehiscence: In certain cases, the incision that is made during the procedure can separate and relocate. This can lead to a long-term recovery process and may cause an increased chance of a secondary infection.
Dumping Syndrome: Rarely, a patient may develop symptoms of dumping syndrome because of pyloroplasty. The dumping syndrome is characterized by early and rapid emptying of stomach contents into the small bowel. Patients may experience abdominal cramping, diarrhea, sweating and light-headedness as their major symptoms.
Pyloric Stenosis Recurrence: Although the complete elimination of the recurrent pyloric stenosis is possible, the risk remains, especially for the cases after treatment with pyloromyotomy in IHPS.
Gastroesophageal Reflux: Pyloroplasty could be the reason for the esophagus reflux in particular patients and the symptoms they face including regurgitation, heartburn, and chest pain.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



