Background
Rigid sigmoidoscopy is a medical procedure in which the physician inspects the rectum and the lower part of the sigmoid colon.
Rigid sigmoidoscopy has been employed as a diagnostic modality for gastroenterology for over one hundred years. It was created to allow physicians to diagnose hemorrhoids, polyps, tumors, inflammation, or any other abnormality in the rectum and the lower part of the large colon.
It has been used less frequently over recent years due to flexible sigmoidoscopy and colonoscopy, through which examination of the colon can be performed to a greater extent, and the procedures are comfortable for the patients.
Indications
Evaluation of Rectal Bleeding: In bleeding disorders such as hemorrhoids, polyps, tumors, or any other type of lesson.
Assessment of Anorectal Pain: To establish the causes of pain, ranging from fissures to abscesses and many other conditions.
Diagnosis and Biopsy of Suspected Lesions: In the process of taking a biopsy from anomalous growths or ulcers to get a histopathological exam.
Foreign Body Removal: Most commonly identify and possibly evacuate foreign bodies lodged within the rectum or sigmoid colon.
Follow-Up for Previously Identified Pathologies: For the surveillance of those already identified conditions, for instance, polyps, strictures, or any other lesion.
Screening for Colorectal Cancer: It is applied for screening or surveillance, especially if flexible sigmoidoscopy or colonoscopy is unavailable or unsuitable.
Evaluation of Chronic Diarrhea or Constipation: Thus, it is important to assist in defining chronic bowel habit alterations when other investigations are inconclusive.
Assessment of Rectal Prolapse: To assess the degree and state of the protruding rectum.
Contraindications
Suspected Perforation: Bowel perforation is considered a contraindication to therapy since any suspicion of the perforation will worsen the condition.
Acute Diverticulitis: It may cause inflammation or perforation of the gastrointestinal tract at certain points of this procedure.
Acute Peritonitis: There is a tendency of worsening peritoneal inflammation when bowel is altered.
Severe Pain or Discomfort: Discomfort or pain that a patient experiences and cannot endure will slow the procedure.
Significant Rectal or Anal Pathology: Peripheral conditions by which it may be difficult to examine or insert instruments into the anus include severe hemorrhoids, anal fissures, and strictures.
Recent Colonic Surgery: It may interfere with the wound healing process or with the integrity of the areas affected by surgery.
Outcomes
Equipment
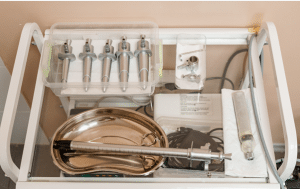
Rigid Sigmoidoscope
Light Source
Obturator
Insufflation Bulb
Lubricant
Biopsy Forceps and Accessories
Light Cable and Connector
Suction Device
Video/Camera System (Optional)
Irrigation System (Optional)
Patient Preparation:
Bowel Preparation
Enema: The basic approach for the preparation of the bowel prior to the rigid sigmoidoscopy is through cleansing enema. Normally before the procedure, one or two enemas are given several hours prior to the procedure to clean the lower bowel.
Dietary Restrictions: Usually, a light diet or fasting may be advised on the day of the procedure.
Technique
Step 1: Preparation:
Convey to the patient what will happen in the procedure, any discomfort that may be involved, etc.
Obtain informed consent.
Put the patient in the left lateral (Sims’) position with the knees drawn towards the chest to enable easy examination of the rectum and the sigmoid colon.
A digital rectal examination is usually the initial test to check if anything is blocking the colon.
Equipment:
Rigid sigmoidoscope: It is a short, straight metal tube containing a light source and an eyepiece for visual purposes.
Insufflation bulb: To distend the colon to obtain better views.
Lubricant: To allow for easier insertion into the body and less discomfort for the patient.
Suction device: To clear the view from any fecal matter, mucus, or blood present.
Step 2: Insertion:
Make sure that the sigmoidoscope is well lubricated.
Twirl the buttocks and lubricating the scope, undertake anal insertion of the device with the obturator which is blunt and is mounted within the scope to spare the mucosal chance of injury.
Place the lubricated tip of the sigmoidoscope into the anus and slowly advance it along the anal canal until the sigmoidoscope reaches the rectum; to do this, the sigmoidoscope should be slightly directed in the posterior plane, following the anatomical curvature of the rectum.
When the scope is beyond the anal canal, retract the obturator and fix the position of the scope and connect the light source to it.
Step 3: Inspection and Advancement:
If necessary, conduct a Rectal examination as you proceed with the colonoscopy. you may use an insufflation bulb to tamponade distend or rectum and sigmoid colon for visibility.
Rotate and advance the scope gently, visualizing the mucosa as you go. Avoid forceful insertion to reduce the risk of perforation or injury.
If feces, mucus, or blood obscure the view, then the suction device should be used.
Extend the colonic mobilization up to the level of the splenic flexure, about 15-25 cm from the margin of the anus, depending on the condition of the patient and their capability to tolerate the procedure.
Step 4: Assessment:
Examine the mucosa for lesions and polyps, tumors, inflammation, bleeding, or other signs of disease.
Note the color, texture, and any lesions or abnormalities encountered.
If required, tissue samples can be obtained through the forceps passed through the scope.
Step 5: Withdrawal:
Gradually pull out the sigmoidoscope and take another look at the color and appearance of the mucosa.
Remove the insufflation gas gently to minimize patient discomfort.
Once the scope is fully pulled out, clean the surrounding area around the anus if necessary.
Step 6: Post-Procedure
During the assessment, discussing the obtained findings with the patient should be necessary.
If biopsies or abnormal findings were taken, make the necessary examinations, surgeries, or consultations.
Supervise the patient for a short period of time in case any side reactions would have manifested mainly if any therapeutic procedures were done.
Complications
Perforation: This is a very rare but rather severe condition in which an opening or rupture occurs at the rectal or colon lining. It may require surgical intervention.
Bleeding: Any minor bleeding may be seen mainly if a biopsy has been done or if conditions such as hemorrhoids or polyps are present.
Infection: There is less possibility to get an infection where the procedure is invasive or where it has contact with fecal matter, such as when a biopsy is taken.
Pain or Discomfort: Some patients may complain of pain or discomfort during the procedure, especially if there is a stricture or inflammation.
Vasovagal Response: A vasovagal reaction is possible in some of the patients and may result in such signs as dizziness, nausea, sweating, or even fainting due to the discomfort or anxiety associated with the procedure.
Rectal Injury: The rigid scope may produce minor damage to the rectal mucosa, including abrasion or tear.
Medication
Anticoagulants and Antiplatelet Agents: Patients should tell their doctor any medications they are on especially if they are taking anti-coagulating medications.
Pain Management: Rigid sigmoidoscopy is largely tolerated but, minor sedation/analgesia may be appropriate when needed.
Instructions to the Patient
Clothing: The patient is instructed to wear loose and comfortable cloths during the procedure.
Consent and Explanation: A healthcare provider should provide the patient with information about the procedure, its advantages and disadvantages and get the patient’s consent.
Pre-Procedure Assessment
Medical History: A patient’s medical history concerns their gastrointestinal complaints, and what operation or pathology the patient underwent previously is pertinent.
Vital Signs: Take vital signs, especially when sedation is expected to be given, and assess the patient’s status.
Patient position:
In a rigid sigmoidoscopy, the most appropriate position for the patient is Sims’ or left lateral decubitus.
This position is ideal for examining the rectum and sigmoid colon since the physician and the patient don’t feel uncomfortable.
Medication

Rigid sigmoidoscopy is a medical procedure in which the physician inspects the rectum and the lower part of the sigmoid colon.
Rigid sigmoidoscopy has been employed as a diagnostic modality for gastroenterology for over one hundred years. It was created to allow physicians to diagnose hemorrhoids, polyps, tumors, inflammation, or any other abnormality in the rectum and the lower part of the large colon.
It has been used less frequently over recent years due to flexible sigmoidoscopy and colonoscopy, through which examination of the colon can be performed to a greater extent, and the procedures are comfortable for the patients.
Evaluation of Rectal Bleeding: In bleeding disorders such as hemorrhoids, polyps, tumors, or any other type of lesson.
Assessment of Anorectal Pain: To establish the causes of pain, ranging from fissures to abscesses and many other conditions.
Diagnosis and Biopsy of Suspected Lesions: In the process of taking a biopsy from anomalous growths or ulcers to get a histopathological exam.
Foreign Body Removal: Most commonly identify and possibly evacuate foreign bodies lodged within the rectum or sigmoid colon.
Follow-Up for Previously Identified Pathologies: For the surveillance of those already identified conditions, for instance, polyps, strictures, or any other lesion.
Screening for Colorectal Cancer: It is applied for screening or surveillance, especially if flexible sigmoidoscopy or colonoscopy is unavailable or unsuitable.
Evaluation of Chronic Diarrhea or Constipation: Thus, it is important to assist in defining chronic bowel habit alterations when other investigations are inconclusive.
Assessment of Rectal Prolapse: To assess the degree and state of the protruding rectum.
Suspected Perforation: Bowel perforation is considered a contraindication to therapy since any suspicion of the perforation will worsen the condition.
Acute Diverticulitis: It may cause inflammation or perforation of the gastrointestinal tract at certain points of this procedure.
Acute Peritonitis: There is a tendency of worsening peritoneal inflammation when bowel is altered.
Severe Pain or Discomfort: Discomfort or pain that a patient experiences and cannot endure will slow the procedure.
Significant Rectal or Anal Pathology: Peripheral conditions by which it may be difficult to examine or insert instruments into the anus include severe hemorrhoids, anal fissures, and strictures.
Recent Colonic Surgery: It may interfere with the wound healing process or with the integrity of the areas affected by surgery.
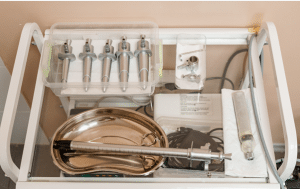
Rigid Sigmoidoscope
Light Source
Obturator
Insufflation Bulb
Lubricant
Biopsy Forceps and Accessories
Light Cable and Connector
Suction Device
Video/Camera System (Optional)
Irrigation System (Optional)
Patient Preparation:
Bowel Preparation
Enema: The basic approach for the preparation of the bowel prior to the rigid sigmoidoscopy is through cleansing enema. Normally before the procedure, one or two enemas are given several hours prior to the procedure to clean the lower bowel.
Dietary Restrictions: Usually, a light diet or fasting may be advised on the day of the procedure.
Step 1: Preparation:
Convey to the patient what will happen in the procedure, any discomfort that may be involved, etc.
Obtain informed consent.
Put the patient in the left lateral (Sims’) position with the knees drawn towards the chest to enable easy examination of the rectum and the sigmoid colon.
A digital rectal examination is usually the initial test to check if anything is blocking the colon.
Equipment:
Rigid sigmoidoscope: It is a short, straight metal tube containing a light source and an eyepiece for visual purposes.
Insufflation bulb: To distend the colon to obtain better views.
Lubricant: To allow for easier insertion into the body and less discomfort for the patient.
Suction device: To clear the view from any fecal matter, mucus, or blood present.
Step 2: Insertion:
Make sure that the sigmoidoscope is well lubricated.
Twirl the buttocks and lubricating the scope, undertake anal insertion of the device with the obturator which is blunt and is mounted within the scope to spare the mucosal chance of injury.
Place the lubricated tip of the sigmoidoscope into the anus and slowly advance it along the anal canal until the sigmoidoscope reaches the rectum; to do this, the sigmoidoscope should be slightly directed in the posterior plane, following the anatomical curvature of the rectum.
When the scope is beyond the anal canal, retract the obturator and fix the position of the scope and connect the light source to it.
Step 3: Inspection and Advancement:
If necessary, conduct a Rectal examination as you proceed with the colonoscopy. you may use an insufflation bulb to tamponade distend or rectum and sigmoid colon for visibility.
Rotate and advance the scope gently, visualizing the mucosa as you go. Avoid forceful insertion to reduce the risk of perforation or injury.
If feces, mucus, or blood obscure the view, then the suction device should be used.
Extend the colonic mobilization up to the level of the splenic flexure, about 15-25 cm from the margin of the anus, depending on the condition of the patient and their capability to tolerate the procedure.
Step 4: Assessment:
Examine the mucosa for lesions and polyps, tumors, inflammation, bleeding, or other signs of disease.
Note the color, texture, and any lesions or abnormalities encountered.
If required, tissue samples can be obtained through the forceps passed through the scope.
Step 5: Withdrawal:
Gradually pull out the sigmoidoscope and take another look at the color and appearance of the mucosa.
Remove the insufflation gas gently to minimize patient discomfort.
Once the scope is fully pulled out, clean the surrounding area around the anus if necessary.
Step 6: Post-Procedure
During the assessment, discussing the obtained findings with the patient should be necessary.
If biopsies or abnormal findings were taken, make the necessary examinations, surgeries, or consultations.
Supervise the patient for a short period of time in case any side reactions would have manifested mainly if any therapeutic procedures were done.
Complications
Perforation: This is a very rare but rather severe condition in which an opening or rupture occurs at the rectal or colon lining. It may require surgical intervention.
Bleeding: Any minor bleeding may be seen mainly if a biopsy has been done or if conditions such as hemorrhoids or polyps are present.
Infection: There is less possibility to get an infection where the procedure is invasive or where it has contact with fecal matter, such as when a biopsy is taken.
Pain or Discomfort: Some patients may complain of pain or discomfort during the procedure, especially if there is a stricture or inflammation.
Vasovagal Response: A vasovagal reaction is possible in some of the patients and may result in such signs as dizziness, nausea, sweating, or even fainting due to the discomfort or anxiety associated with the procedure.
Rectal Injury: The rigid scope may produce minor damage to the rectal mucosa, including abrasion or tear.
Anticoagulants and Antiplatelet Agents: Patients should tell their doctor any medications they are on especially if they are taking anti-coagulating medications.
Pain Management: Rigid sigmoidoscopy is largely tolerated but, minor sedation/analgesia may be appropriate when needed.
Instructions to the Patient
Clothing: The patient is instructed to wear loose and comfortable cloths during the procedure.
Consent and Explanation: A healthcare provider should provide the patient with information about the procedure, its advantages and disadvantages and get the patient’s consent.
Pre-Procedure Assessment
Medical History: A patient’s medical history concerns their gastrointestinal complaints, and what operation or pathology the patient underwent previously is pertinent.
Vital Signs: Take vital signs, especially when sedation is expected to be given, and assess the patient’s status.
Patient position:
In a rigid sigmoidoscopy, the most appropriate position for the patient is Sims’ or left lateral decubitus.
This position is ideal for examining the rectum and sigmoid colon since the physician and the patient don’t feel uncomfortable.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



