Background
Strictureplasty is a surgical procedure performed to treat bowel strictures (The narrow part of the intestines), leading to the development of obstruction. This technique is used basically in the management of Crohn’s disease, which is a chronic inflammatory condition that is known to result in the formation of strictures from the constant formation of scar tissues from inflammation and subsequent healing.
Indications
Crohn’s Disease: It is the most frequent indication, and it is used when there are multiple, short or moderate numbers of strictures in the small bowel, mainly in the jejunum and ileum, which should not be more than 10-15 cm in length.
Recurrent Strictures: It is a reconstructive procedure used in postoperative patients when resections were made before, so further resections cannot be made due to short bowel syndrome.
Multiple Strictures: When there are many strictures along a long segment of the bowel, strictureplasty can deal with it without having to perform major bowel resection.
Fibrotic Strictures: If strictures involve mainly fibrosis and no active inflammation or abscess formation, the surgery of choice is strictureplasty.
Strictures in Areas Difficult to Resect: There are some strictures that cannot undergo resection that will involve a lot of complications or will be complicated, especially when the stricture is in areas such as duodenum where it will be difficult to perform the resection.
Contraindications
Extensive Inflammatory Disease: In the case of extensive inflammation of the bowel segment, the risk of complications is high, so it is better to perform a resection and not a strictureplasty.
Active Infection or Abscess: An acute ongoing intra-abdominal infection or abscess near the stricture status also poses additional risk factors for post-operative complications.
Carcinoma: Whenever there is degeneration or even clinical/suspected malignancy in the stricture, then the procedure of strictureplasty is absolutely contraindicated due to the inability to resect out and examine the strictured tissue completely.
Short Bowel Syndrome Risk: No more than two procedures should be performed because if several procedures are done and one is left with a critically short length of functioning small bowel, there is a high risk of developing short bowel syndrome.
Severely Thickened or Fibrotic Bowel: If the bowel wall is very thickened or fibrotic, then doing a strictureplasty may not be possible or will not yield good results.
Strictures Near the Ileocecal Valve or Colon: Strictureplasty is typically not performed near the ileocecal valve or in the colon because of the risk of poor outcomes.
Fistulae Involving the Stricture: Since strictureplasty is not possible in fistulae structures, strictures related to fistulae, especially complicated or multiple fistulae, are not considered to be suitable for surgery.
Outcomes
Equipment

Surgical equipment
Hemostatic Clamps
Suction Devices
Retractors
Needle Holders
Scissors
Forceps
Scalpels
Energy Devices
Ultrasonic Dissectors
Electrocautery Devices
Stapling Devices (if required)
Bowel Clamps
Suture Materials
Patient Preparation
Preoperative Evaluation:
Medical History and Physical Examination: Some of the tests include the patient’s general health, the previous operations that the patient has undergone, and the medication the patient is on prior to surgery or that may affect surgery or recovery.
Imaging Studies: The location, length and number of strictures are diagnosed by diagnostic examinations that are CT scan, MRI or small bowel enteroscopy.
Laboratory Tests: Investigations which are usually carried in the routine include Complete Blood count, electrolyte profile, Liver and renal function test and coagulation profile.
Nutritional Assessment: Crohn’s disease patients are usually malnourished; dietary advice and possible treatment to enhance nutritional status (for instance, by means of enteral nutrition or supplements) might be necessary due to the disease.
Bowel Preparation:
Laxatives or Enemas: At times, it may involve mechanical prep in which the bowel is cleansed; however, this is not very common, especially in the emergency settings.
Fasting: The major preoperative instructions given to the patient include fasting or no food and drink in the least periods of 6-8 hours before surgery.
Anesthesia Evaluation:
Pre-Anesthetic Assessment: Clinical assessment by the anesthesiologist to determine patient’s risk factors and the strategy that will be opted for selection of suitable anesthesia.
Patient Education and Consent:
Procedure Explanation: It is important to explain the procedure, potential complications of a given procedure and/or treatment, benefits, and other reasonable possibilities to a patient.
Consent: It is a requirement that the patient has to give consent after the various aspects concerning surgery have been discussed.
Patient position:
For strictureplasty, the patient is usually placed in the supine position. This assists the Surgeon in complete view and access to the abdominal cavity and enables the required exposure and handling of the intestines.
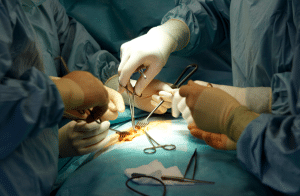
Technique
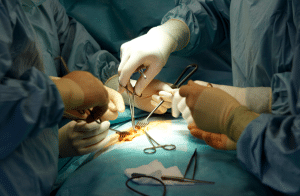
Heineke-Mikulicz Strictureplasty
Step 1-Patient Preparation and Positioning: The patient lies on the operating table on his/her back and gets under general anesthesia. To enter the abdominal cavity, a midline laparotomy is done.
Step 2-Identification of Stricture: The small intestine is then assessed to pinpoint the area and the degree of the constricted area, the stricture. The Heineke-Mikulicz technique is effective for short strictures (up to 10cm in length).
Step 3-Isolation of the Stricture: The bowel is then mobilized to ease the separation of the stricture from the rest of the loops of the intestine. Bowel clamps or moist gauze pads may be used to protect and/or isolate the area.
Step 4-Longitudinal Enterotomy: A longitudinal incision is made along the antimesenteric border of the stricture, extending beyond the strictured area by a few centimeters on either side. This incision is typically placed directly over the site of the stricture.
Step 5-Transverse Closure: As it is, the longitudinal incision is now closed in transverse fashion. This is done with interrupted or continuous sutures; typically using non-absorbable materials such as 3-0 or 4-0 Vicryl. The transverse closure is displaced outwards, which helps widen the lumen of the bowel and eradicates the stricture.
Step 6-Check for Patency: The bowel lumen is patent, and to make sure that there is no narrowing of the lumen at the site of the stricture. The edges of the wound should be smooth and tension-free, as well as the blood supply to the tissues.
Step 7-Hemostasis and Clean-Up: Any bleeding is controlled, and the surgical site is cleaned. The bowel is returned to the abdominal cavity.
Step 8-Closure of the Abdomen: Further turn to the hemostasis, and any bleeding spot in the abdominal cavity is coagulated. A final layer closure of the laparotomy incision is made. It is then important that the fascia is also closed using a non-absorbable suture, and the skin can be sutured or stapled.
Step 9-Postoperative Care:
Postoperative care includes pain management, nutritional support, and monitoring for recurrence of symptoms.
Complications
Anastomotic Leak: Failure of the healing site of the strictureplasty, leading to leakage in the abdomen, may result in peritonitis or sepsis.
Fistula formation: It is an atypical association that can be between the intestine and other organs or tissues like skin or bladder after surgery.
Delayed Emptying of the Stomach: Majorly associated with the duodenum, there may be a possibility of potential of delayed emptying after the surgery and presents as vomiting and nausea.
Stricture recurrence: While strictureplasty is designed to relieve strictures, new strictures can form over time, possibly necessitating additional surgery.
References
References

Strictureplasty is a surgical procedure performed to treat bowel strictures (The narrow part of the intestines), leading to the development of obstruction. This technique is used basically in the management of Crohn’s disease, which is a chronic inflammatory condition that is known to result in the formation of strictures from the constant formation of scar tissues from inflammation and subsequent healing.
Crohn’s Disease: It is the most frequent indication, and it is used when there are multiple, short or moderate numbers of strictures in the small bowel, mainly in the jejunum and ileum, which should not be more than 10-15 cm in length.
Recurrent Strictures: It is a reconstructive procedure used in postoperative patients when resections were made before, so further resections cannot be made due to short bowel syndrome.
Multiple Strictures: When there are many strictures along a long segment of the bowel, strictureplasty can deal with it without having to perform major bowel resection.
Fibrotic Strictures: If strictures involve mainly fibrosis and no active inflammation or abscess formation, the surgery of choice is strictureplasty.
Strictures in Areas Difficult to Resect: There are some strictures that cannot undergo resection that will involve a lot of complications or will be complicated, especially when the stricture is in areas such as duodenum where it will be difficult to perform the resection.
Extensive Inflammatory Disease: In the case of extensive inflammation of the bowel segment, the risk of complications is high, so it is better to perform a resection and not a strictureplasty.
Active Infection or Abscess: An acute ongoing intra-abdominal infection or abscess near the stricture status also poses additional risk factors for post-operative complications.
Carcinoma: Whenever there is degeneration or even clinical/suspected malignancy in the stricture, then the procedure of strictureplasty is absolutely contraindicated due to the inability to resect out and examine the strictured tissue completely.
Short Bowel Syndrome Risk: No more than two procedures should be performed because if several procedures are done and one is left with a critically short length of functioning small bowel, there is a high risk of developing short bowel syndrome.
Severely Thickened or Fibrotic Bowel: If the bowel wall is very thickened or fibrotic, then doing a strictureplasty may not be possible or will not yield good results.
Strictures Near the Ileocecal Valve or Colon: Strictureplasty is typically not performed near the ileocecal valve or in the colon because of the risk of poor outcomes.
Fistulae Involving the Stricture: Since strictureplasty is not possible in fistulae structures, strictures related to fistulae, especially complicated or multiple fistulae, are not considered to be suitable for surgery.

Surgical equipment
Hemostatic Clamps
Suction Devices
Retractors
Needle Holders
Scissors
Forceps
Scalpels
Energy Devices
Ultrasonic Dissectors
Electrocautery Devices
Stapling Devices (if required)
Bowel Clamps
Suture Materials
Preoperative Evaluation:
Medical History and Physical Examination: Some of the tests include the patient’s general health, the previous operations that the patient has undergone, and the medication the patient is on prior to surgery or that may affect surgery or recovery.
Imaging Studies: The location, length and number of strictures are diagnosed by diagnostic examinations that are CT scan, MRI or small bowel enteroscopy.
Laboratory Tests: Investigations which are usually carried in the routine include Complete Blood count, electrolyte profile, Liver and renal function test and coagulation profile.
Nutritional Assessment: Crohn’s disease patients are usually malnourished; dietary advice and possible treatment to enhance nutritional status (for instance, by means of enteral nutrition or supplements) might be necessary due to the disease.
Bowel Preparation:
Laxatives or Enemas: At times, it may involve mechanical prep in which the bowel is cleansed; however, this is not very common, especially in the emergency settings.
Fasting: The major preoperative instructions given to the patient include fasting or no food and drink in the least periods of 6-8 hours before surgery.
Anesthesia Evaluation:
Pre-Anesthetic Assessment: Clinical assessment by the anesthesiologist to determine patient’s risk factors and the strategy that will be opted for selection of suitable anesthesia.
Patient Education and Consent:
Procedure Explanation: It is important to explain the procedure, potential complications of a given procedure and/or treatment, benefits, and other reasonable possibilities to a patient.
Consent: It is a requirement that the patient has to give consent after the various aspects concerning surgery have been discussed.
Patient position:
For strictureplasty, the patient is usually placed in the supine position. This assists the Surgeon in complete view and access to the abdominal cavity and enables the required exposure and handling of the intestines.
Heineke-Mikulicz Strictureplasty
Step 1-Patient Preparation and Positioning: The patient lies on the operating table on his/her back and gets under general anesthesia. To enter the abdominal cavity, a midline laparotomy is done.
Step 2-Identification of Stricture: The small intestine is then assessed to pinpoint the area and the degree of the constricted area, the stricture. The Heineke-Mikulicz technique is effective for short strictures (up to 10cm in length).
Step 3-Isolation of the Stricture: The bowel is then mobilized to ease the separation of the stricture from the rest of the loops of the intestine. Bowel clamps or moist gauze pads may be used to protect and/or isolate the area.
Step 4-Longitudinal Enterotomy: A longitudinal incision is made along the antimesenteric border of the stricture, extending beyond the strictured area by a few centimeters on either side. This incision is typically placed directly over the site of the stricture.
Step 5-Transverse Closure: As it is, the longitudinal incision is now closed in transverse fashion. This is done with interrupted or continuous sutures; typically using non-absorbable materials such as 3-0 or 4-0 Vicryl. The transverse closure is displaced outwards, which helps widen the lumen of the bowel and eradicates the stricture.
Step 6-Check for Patency: The bowel lumen is patent, and to make sure that there is no narrowing of the lumen at the site of the stricture. The edges of the wound should be smooth and tension-free, as well as the blood supply to the tissues.
Step 7-Hemostasis and Clean-Up: Any bleeding is controlled, and the surgical site is cleaned. The bowel is returned to the abdominal cavity.
Step 8-Closure of the Abdomen: Further turn to the hemostasis, and any bleeding spot in the abdominal cavity is coagulated. A final layer closure of the laparotomy incision is made. It is then important that the fascia is also closed using a non-absorbable suture, and the skin can be sutured or stapled.
Step 9-Postoperative Care:
Postoperative care includes pain management, nutritional support, and monitoring for recurrence of symptoms.
Anastomotic Leak: Failure of the healing site of the strictureplasty, leading to leakage in the abdomen, may result in peritonitis or sepsis.
Fistula formation: It is an atypical association that can be between the intestine and other organs or tissues like skin or bladder after surgery.
Delayed Emptying of the Stomach: Majorly associated with the duodenum, there may be a possibility of potential of delayed emptying after the surgery and presents as vomiting and nausea.
Stricture recurrence: While strictureplasty is designed to relieve strictures, new strictures can form over time, possibly necessitating additional surgery.

Both our subscription plans include Free CME/CPD AMA PRA Category 1 credits.

On course completion, you will receive a full-sized presentation quality digital certificate.
A dynamic medical simulation platform designed to train healthcare professionals and students to effectively run code situations through an immersive hands-on experience in a live, interactive 3D environment.

When you have your licenses, certificates and CMEs in one place, it's easier to track your career growth. You can easily share these with hospitals as well, using your medtigo app.



